Sexually transmitted infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease (STIs) or sexually transmitted diseases (STDs) are infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease that spread either by vaginal intercourse, anal sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria, or oral sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria. Symptoms and signs may include vaginal discharge, penile discharge, dysuria Dysuria Painful urination. It is often associated with infections of the lower urinary tract. Urinary Tract Infections (UTIs), skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions (e.g., warts Warts Benign epidermal proliferations or tumors; some are viral in origin. Female Genitourinary Examination, ulcers) on or around the genitals, and pelvic pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. Some infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease can lead to infertility Infertility Infertility is the inability to conceive in the context of regular intercourse. The most common causes of infertility in women are related to ovulatory dysfunction or tubal obstruction, whereas, in men, abnormal sperm is a common cause. Infertility and chronic debilitating disease. And some STIs can affect infants by vertical transmission Vertical transmission The transmission of infectious disease or pathogens from one generation to another. It includes transmission in utero or intrapartum by exposure to blood and secretions, and postpartum exposure via breastfeeding. Congenital TORCH Infections. Diagnosis of STIs includes a combination of comprehensive medical and sexual history, assessing risk factors, focused genitourinary physical exam, and disease-specific laboratory tests/cultures. Treatment and prevention include a combination of antibiotic/ antiviral Antiviral Antivirals for Hepatitis B agents and patient education on safe sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria practices.
Last updated: Sep 29, 2022
Infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are mainly transmitted sexually, which can include unprotected vaginal, anal, or oral sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria.
| Type of STI | Organism | Signs and symptoms |
|---|---|---|
| Chancroid Chancroid Chancroid is a highly transmissible STD caused by Haemophilus ducreyi. The disease presents with painful ulcer(s) on the genital tract (termed chancroid or “soft chancre”). Up to 50% of patients will develop painful inguinal lymphadenopathy. Chancroid | Haemophilus ducreyi Haemophilus ducreyi A species of Haemophilus that appears to be the pathogen or causative agent of the sexually transmitted disease, chancroid. Haemophilus |
|
| Chlamydia Chlamydia Chlamydiae are obligate intracellular gram-negative bacteria. They lack a peptidoglycan layer and are best visualized using Giemsa stain. The family of Chlamydiaceae comprises 3 pathogens that can infect humans: Chlamydia trachomatis, Chlamydia psittaci, and Chlamydia pneumoniae. Chlamydia | Chlamydia trachomatis Chlamydia trachomatis Type species of Chlamydia causing a variety of ocular and urogenital diseases. Chlamydia |
|
| Gonorrhea Gonorrhea Gonorrhea is a sexually transmitted infection (STI) caused by the gram-negative bacteria Neisseria gonorrhoeae (N. gonorrhoeae). Gonorrhea may be asymptomatic but commonly manifests as cervicitis or urethritis with less common presentations such as proctitis, conjunctivitis, or pharyngitis. Gonorrhea | Neisseria gonorrhoeae Neisseria gonorrhoeae A species of gram-negative, aerobic bacteria primarily found in purulent venereal discharges. It is the causative agent of gonorrhea. Neisseria |
|
| Granuloma inguinale Granuloma inguinale Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis or donovanosis Donovanosis Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis | Klebsiella Klebsiella Klebsiella are encapsulated gram-negative, lactose-fermenting bacilli. They form pink colonies on MacConkey agar due to lactose fermentation. The main virulence factor is a polysaccharide capsule. Klebsiella pneumoniae is the most important pathogenic species. Klebsiella granulomatis |
|
| Lymphogranuloma venereum Lymphogranuloma venereum Subacute inflammation of the inguinal lymph glands caused by certain immunotypes of Chlamydia trachomatis. It is a sexually transmitted disease in the U.S. But is more widespread in developing countries. It is distinguished from granuloma venereum, which is caused by calymmatobacterium granulomatis. Chlamydial Infections ( LGV LGV Subacute inflammation of the inguinal lymph glands caused by certain immunotypes of Chlamydia trachomatis. It is a sexually transmitted disease in the U.S. But is more widespread in developing countries. It is distinguished from granuloma venereum, which is caused by calymmatobacterium granulomatis. Chlamydial Infections) | L1, L2, and L3 serovars of Chlamydia trachomatis Chlamydia trachomatis Type species of Chlamydia causing a variety of ocular and urogenital diseases. Chlamydia |
|
| Mycoplasma genitalium Mycoplasma genitalium A species of gram-negative bacteria originally isolated from urethral specimens of patients with non-gonococcal urethritis. In primates it exists in parasitic association with ciliated epithelial cells in the genital and respiratory tracts. Mycoplasma infection | Mycoplasma genitalium Mycoplasma genitalium A species of gram-negative bacteria originally isolated from urethral specimens of patients with non-gonococcal urethritis. In primates it exists in parasitic association with ciliated epithelial cells in the genital and respiratory tracts. Mycoplasma |
|
| Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis | Treponema pallidum Treponema pallidum The causative agent of venereal and non-venereal syphilis as well as yaws. Treponema |
|

Chancroid: 1-cm lesion on the glans penis confirmed to be from Haemophilus ducreyi
Image: “Chancroid lesion haemophilus ducreyi PHIL 3728 lores” by Joe Miller. License: Public Domain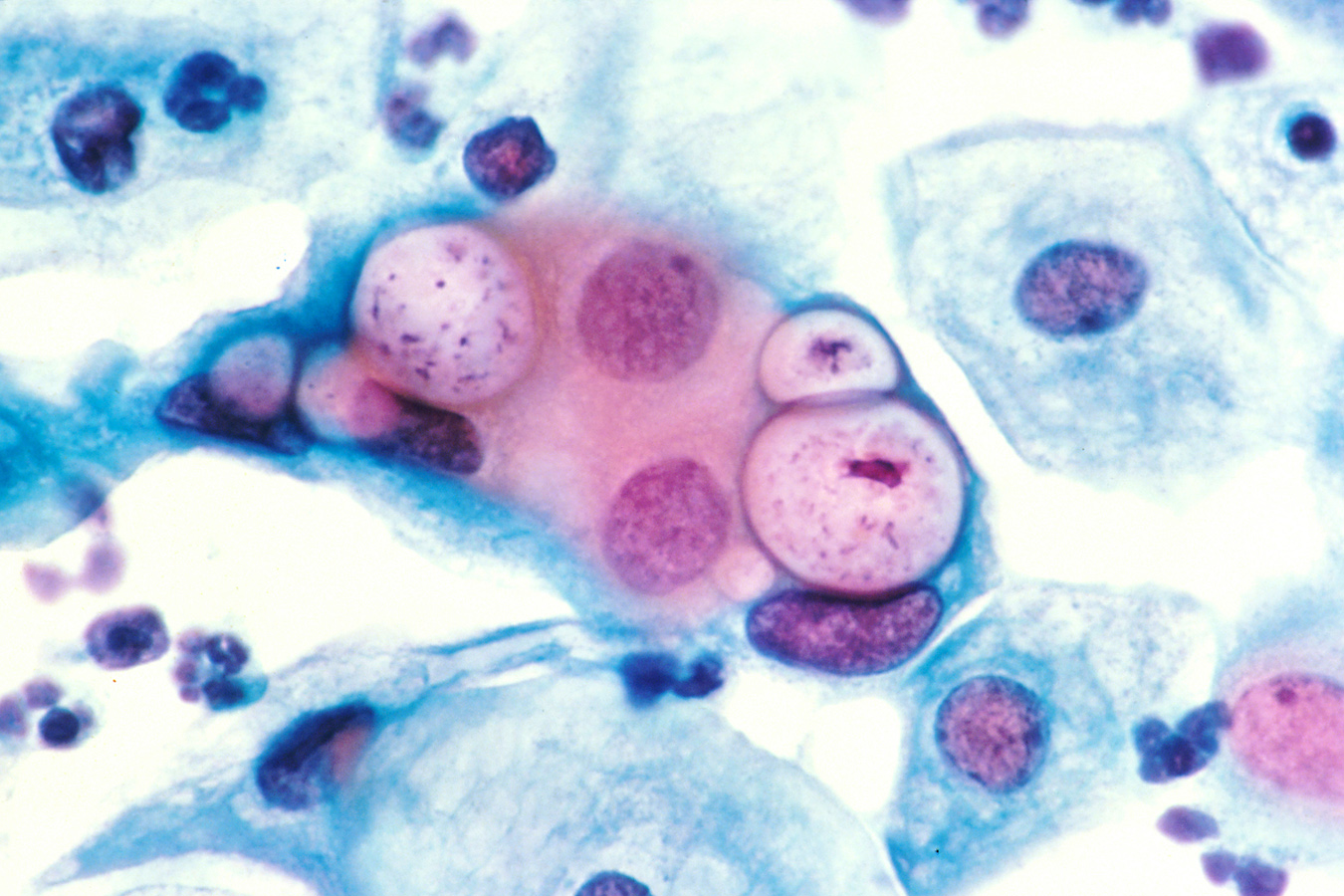
Papanicolaou stain of a cervicovaginal cytology preparation showing 3 chlamydial intranuclear inclusions within squamous epithelial cells that are next to several normal epithelial cells
Image: “Pap smear showing Chlamydia in the vacuoles 500x H&E” by Dr. Lance Liotta Laboratory. License: Public Domain
Purulent penile discharge due to urogenital gonorrhea infection
Image: “4065” by CDC. License: Public Domain
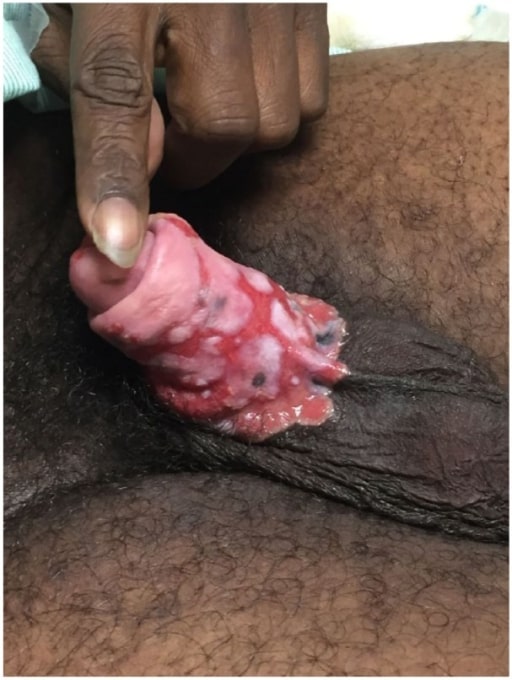
Ulcerative lesions of donovanosis:
A patient’s left inguinal region, revealing the presence of a number of ulcerative erythematous lesions, which were determined to be due to a case of donovanosis

Lymphogranuloma venereum caused by the invasive serovar L1, L2, or L3 of Chlamydia trachomatis:
This young adult experienced an acute onset of tender, enlarged lymph nodes in both groins.
Image: “Lymphogranuloma venerum: lymph nodes” by Herbert L. Fred, Hendrik A. van Dijk. License: CC BY 2.0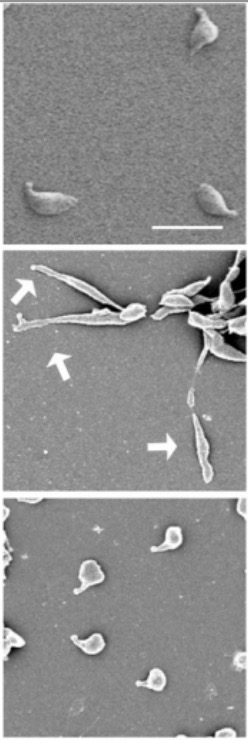
Electron micrograph of Mycloplasma genitalium:
Top and bottom images show typical flask-shaped morphology. Middle image shows filamentous morphology (arrows).

Primary, painless chancre of syphilis (Treponema pallidum infection)
Image: “Chancres on the penile shaft due to a primary syphilitic infection caused by Treponema pallidum 6803 lores” by M. Rein. License: Public Domain| Type of STI | Organism | Signs and symptoms |
|---|---|---|
| Herpes | HSV-1 or 2 | If symptomatic,
patients
Patients
Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures.
Clinician–Patient Relationship manifest:
|
| Hepatitis B Hepatitis B Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Most individuals with acute HBV infection are asymptomatic or have mild, self-limiting symptoms. Chronic infection can be asymptomatic or create hepatic inflammation, leading to liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis B Virus | Hepatitis B Hepatitis B Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Most individuals with acute HBV infection are asymptomatic or have mild, self-limiting symptoms. Chronic infection can be asymptomatic or create hepatic inflammation, leading to liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis B Virus virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology ( HBV HBV Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Hepatitis B virus is transmitted by exposure to infectious blood or body fluids. Examples of types of exposure include sexual intercourse, IV drug use, and childbirth. Hepatitis B Virus) | Acute:
|
| HIV HIV Anti-HIV Drugs | Two species of Lentivirus Lentivirus A genus of the family retroviridae consisting of non-oncogenic retroviruses that produce multi-organ diseases characterized by long incubation periods and persistent infection. Lentiviruses are unique in that they contain open reading frames (orfs) between the pol and env genes and in the 3′ env region. Five serogroups are recognized, reflecting the mammalian hosts with which they are associated. HIV-1 is the type species. Human Immunodeficiency Virus (HIV) | Different disease stages include:
|
| HPV HPV Human papillomavirus (HPV) is a nonenveloped, circular, double-stranded DNA virus belonging to the Papillomaviridae family. Humans are the only reservoir, and transmission occurs through close skin-to-skin or sexual contact. Human papillomaviruses infect basal epithelial cells and can affect cell-regulatory proteins to result in cell proliferation. Papillomavirus (HPV) | Different types (6, 11, 16, and 18) of HPV HPV Human papillomavirus (HPV) is a nonenveloped, circular, double-stranded DNA virus belonging to the Papillomaviridae family. Humans are the only reservoir, and transmission occurs through close skin-to-skin or sexual contact. Human papillomaviruses infect basal epithelial cells and can affect cell-regulatory proteins to result in cell proliferation. Papillomavirus (HPV) |
|
Penile ulcers due to chronic refractory genital herpes in a patient with AIDS
Image: “Penile ulcers” by University of Texas Medical Branch School of Medicine, Galveston, TX, USA. License: CC BY 3.0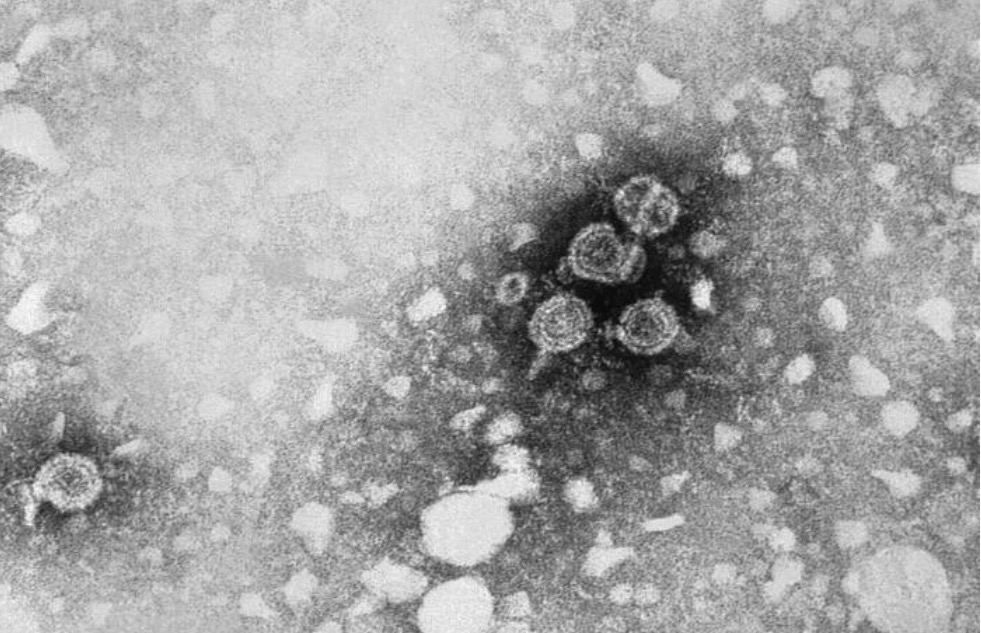
Hepatitis B:
This transmission electron microscopic (TEM) image reveals the presence of hepatitis B virus (HBV) particles. The round virions, which measure 42 nm in diameter, are known as Dane particles.

Cutaneous lesions of Kaposi’s sarcoma
Image: “Kaposi’s sarcoma” by OpenStax College. License: CC BY 3.0
Anogenital warts
Image: “Twenty molluscoid lesions” by Wolters Kluwer Health, Inc.. License: CC BY 4.0| Type of STI | Organism | Signs and symptoms |
|---|---|---|
| Trichomoniasis | Trichomonas Trichomonas A genus of parasitic flagellate eukaryotes distinguished by the presence of four anterior flagella, an undulating membrane, and a trailing flagellum. Nitroimidazoles vaginalis |
|
| Pediculosis pubis or crab louse | Pthirus pubis | Pruritus Pruritus An intense itching sensation that produces the urge to rub or scratch the skin to obtain relief. Atopic Dermatitis (Eczema) in genital and perianal area |
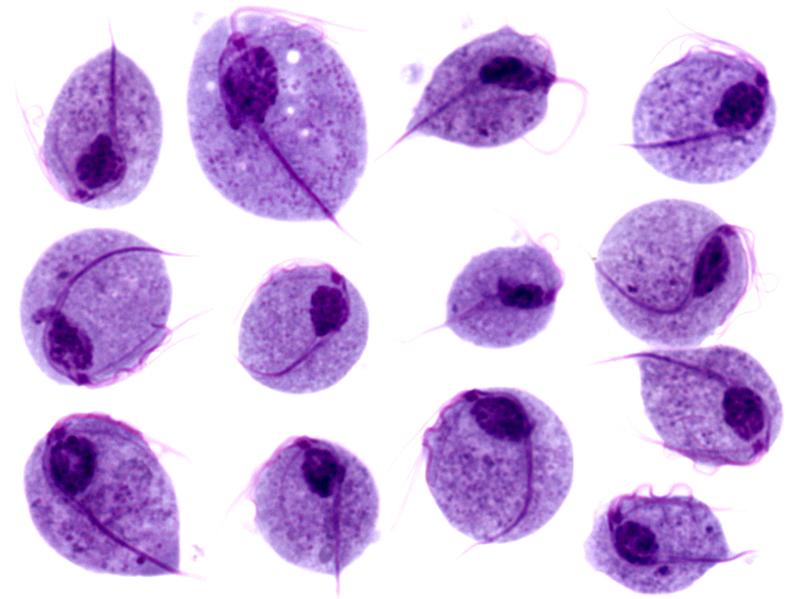
Microscopic images of Trichomonas vaginalis trophozoites
Image: “Trichomonas protozoa” by isis325. License: CC BY 2.0.
Pthirus pubis: pubic or crab louse, an ectoparasite whose only host is humans
Image: “Pthirus pubis” by Daniel J. Drew. License: Public DomainComprehensive sexual history:
Focused physical exam:
Specimen for testing is obtained from the site(s) of infection/lesion, which may include anogenital, lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy, and oral areas.
Bacterial disease:
Viral disease:
Parasitic disease:
| Type of STI | Treatment |
|---|---|
| Chancroid Chancroid Chancroid is a highly transmissible STD caused by Haemophilus ducreyi. The disease presents with painful ulcer(s) on the genital tract (termed chancroid or “soft chancre”). Up to 50% of patients will develop painful inguinal lymphadenopathy. Chancroid | Azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides or ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins |
| Chlamydia Chlamydia Chlamydiae are obligate intracellular gram-negative bacteria. They lack a peptidoglycan layer and are best visualized using Giemsa stain. The family of Chlamydiaceae comprises 3 pathogens that can infect humans: Chlamydia trachomatis, Chlamydia psittaci, and Chlamydia pneumoniae. Chlamydia | Azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides 1 g orally x 1 or doxycycline x 7 days (preferred in proctitis Proctitis Inflammation of the mucous membrane of the rectum, the distal end of the large intestine. Chronic Granulomatous Disease) |
| Gonorrhea Gonorrhea Gonorrhea is a sexually transmitted infection (STI) caused by the gram-negative bacteria Neisseria gonorrhoeae (N. gonorrhoeae). Gonorrhea may be asymptomatic but commonly manifests as cervicitis or urethritis with less common presentations such as proctitis, conjunctivitis, or pharyngitis. Gonorrhea | Ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins 500 mg (with doxycycline if chlamydia Chlamydia Chlamydiae are obligate intracellular gram-negative bacteria. They lack a peptidoglycan layer and are best visualized using Giemsa stain. The family of Chlamydiaceae comprises 3 pathogens that can infect humans: Chlamydia trachomatis, Chlamydia psittaci, and Chlamydia pneumoniae. Chlamydia has not been ruled out) |
| Granuloma inguinale Granuloma inguinale Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis or donovanosis Donovanosis Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. Donovanosis |
|
| Lymphogranuloma venereum Lymphogranuloma venereum Subacute inflammation of the inguinal lymph glands caused by certain immunotypes of Chlamydia trachomatis. It is a sexually transmitted disease in the U.S. But is more widespread in developing countries. It is distinguished from granuloma venereum, which is caused by calymmatobacterium granulomatis. Chlamydial Infections ( LGV LGV Subacute inflammation of the inguinal lymph glands caused by certain immunotypes of Chlamydia trachomatis. It is a sexually transmitted disease in the U.S. But is more widespread in developing countries. It is distinguished from granuloma venereum, which is caused by calymmatobacterium granulomatis. Chlamydial Infections) | Doxycycline |
| Mycoplasma genitalium Mycoplasma genitalium A species of gram-negative bacteria originally isolated from urethral specimens of patients with non-gonococcal urethritis. In primates it exists in parasitic association with ciliated epithelial cells in the genital and respiratory tracts. Mycoplasma infection | Azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides |
| Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis | Penicillin Penicillin Rheumatic Fever G (parenteral) |
| Type of STI | Treatment |
|---|---|
| Herpes | Antivirals:
|
| HPV HPV Human papillomavirus (HPV) is a nonenveloped, circular, double-stranded DNA virus belonging to the Papillomaviridae family. Humans are the only reservoir, and transmission occurs through close skin-to-skin or sexual contact. Human papillomaviruses infect basal epithelial cells and can affect cell-regulatory proteins to result in cell proliferation. Papillomavirus (HPV) | Cytodestructive therapy:
|
| HIV HIV Anti-HIV Drugs | Combination
antiretroviral therapy
Antiretroviral therapy
Antiretroviral therapy (ART) targets the replication cycle of the human immunodeficiency virus (HIV) and is classified based on the viral enzyme or mechanism that is inhibited. The goal of therapy is to suppress viral replication to reach the outcome of undetected viral load.
Anti-HIV Drugs with the following:
|
| Hepatitis B Hepatitis B Hepatitis B virus (HBV) is a partially double-stranded DNA virus, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Most individuals with acute HBV infection are asymptomatic or have mild, self-limiting symptoms. Chronic infection can be asymptomatic or create hepatic inflammation, leading to liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis B Virus |
|
| Type of STI | Treatment |
|---|---|
| Trichomoniasis |
|
| Pediculosis pubis | Topical permethrin Permethrin A pyrethroid insecticide commonly used in the treatment of lice infestations and scabies. Scabies or topical pyrethrins with piperonyl butoxide |