Epididymitis and orchitis are characterized by acute inflammation Acute Inflammation Inflammation of the epididymis Epididymis The convoluted cordlike structure attached to the posterior of the testis. Epididymis consists of the head (caput), the body (corpus), and the tail (cauda). A network of ducts leaving the testis joins into a common epididymal tubule proper which provides the transport, storage, and maturation of spermatozoa. Testicles: Anatomy and the testicle, respectively, due to viral or bacterial infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with gradually worsening testicular pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and scrotal swelling Swelling Inflammation along with systemic symptoms such as fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, depending on severity. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with concomitant sexually transmitted diseases (STDs) may present with lower urinary tract Urinary tract The urinary tract is located in the abdomen and pelvis and consists of the kidneys, ureters, urinary bladder, and urethra. The structures permit the excretion of urine from the body. Urine flows from the kidneys through the ureters to the urinary bladder and out through the urethra. Urinary Tract: Anatomy symptoms. Diagnosis is based on clinical findings and urinalysis Urinalysis Examination of urine by chemical, physical, or microscopic means. Routine urinalysis usually includes performing chemical screening tests, determining specific gravity, observing any unusual color or odor, screening for bacteriuria, and examining the sediment microscopically. Urinary Tract Infections (UTIs) in Children with culture. Scrotal ultrasound may show increased blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure to the affected epididymis Epididymis The convoluted cordlike structure attached to the posterior of the testis. Epididymis consists of the head (caput), the body (corpus), and the tail (cauda). A network of ducts leaving the testis joins into a common epididymal tubule proper which provides the transport, storage, and maturation of spermatozoa. Testicles: Anatomy or testicle. Treatment is with empiric gram-negative coverage antibiotics and culture-directed therapy. Supportive care includes scrotal support and non-steroidal anti-inflammatory drugs.
Last updated: Mar 24, 2023
Epididymitis and orchitis are the most common causes of scrotal pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways in adults (> 600,000 cases per year in the United States).
Causes:

Epididymo-orchitis: presenting with swollen and tender right testicle, which appears larger compared to the normal left testicle
Image: “Painless mass” by Division of Pediatric Surgery, Oita Prefectural Hospital, 476 Bunyou Oita, Japan. License: CC BY 2.0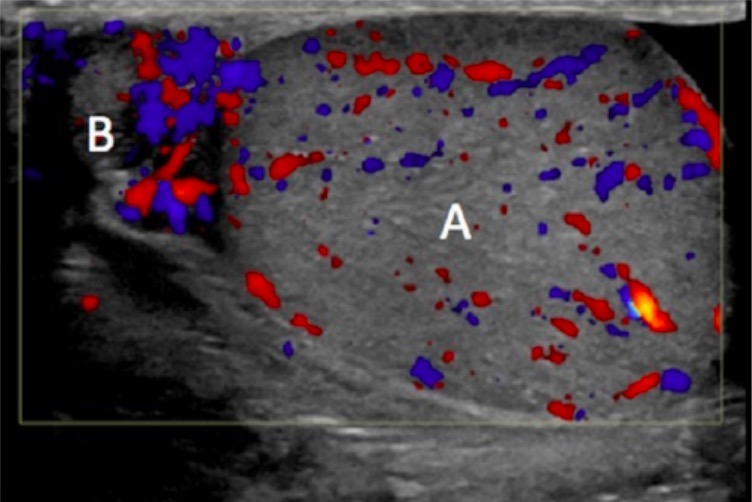
Testicular ultrasound depicting the inflamed epididymis (B) with increased blood flow; testicle (A) with normal blood flow
Image: “Right scrotal ultrasound with color Doppler” by University of Pittsburgh, Graduate School of Medicine, 401 Scaife Hall, 3550 Terrace Street, Pittsburgh, PA 15261, USA. License: CC BY 3.0