Testicular torsion is the sudden rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays of the testicle, specifically the spermatic cord Spermatic Cord Either of a pair of tubular structures formed by ductus deferens; arteries; veins; lymphatic vessels; and nerves. The spermatic cord extends from the deep inguinal ring through the inguinal canal to the testis in the scrotum. Testicles: Anatomy, around its axis in the inguinal canal Inguinal canal The tunnel in the lower anterior abdominal wall through which the spermatic cord, in the male; round ligament, in the female; nerves; and vessels pass. Its internal end is at the deep inguinal ring and its external end is at the superficial inguinal ring. Inguinal Canal: Anatomy and Hernias or below. The acute rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays results in compromised blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure to and from the testicle, which puts the testicle at risk for necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage. Quick diagnosis and intervention is key to saving the affected testicle. Emergent surgical exploration with subsequent orchidopexy is required. Ultrasound or manual detorsion should not delay definitive care.
Last updated: Dec 1, 2024
Testicular torsion:
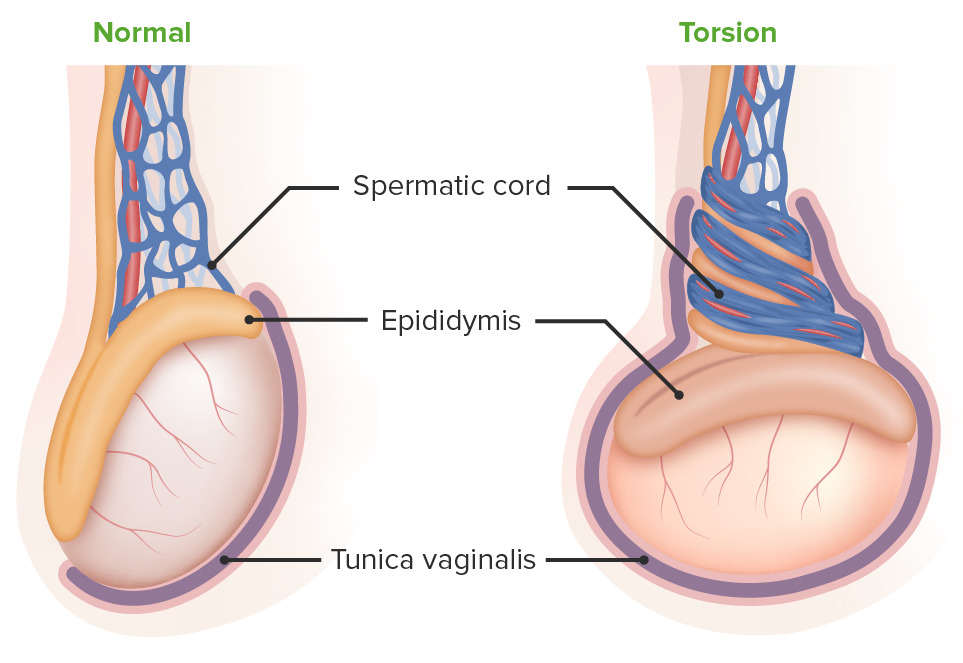
The left image depicts a normal testicle. Testicular torsion is seen on the right: The testicle lies horizontally, creating an increased risk of torsion of the spermatic vessels.
| Clinical feature | Points |
|---|---|
| Testicular swelling Swelling Inflammation | 2 |
| Hard testicle | 2 |
| Absent cremasteric reflex Cremasteric Reflex Male Genitourinary Examination | 1 |
| High-riding testicle | 1 |
| Nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics/ vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia | 1 |

Intraoperative scrotal exploration for testicular torsion:
A: blue discolored testicle devoid of blood supply and twisted spermatic cord
B: prior orchiopexy sutures denoting recurrent testicular torsion
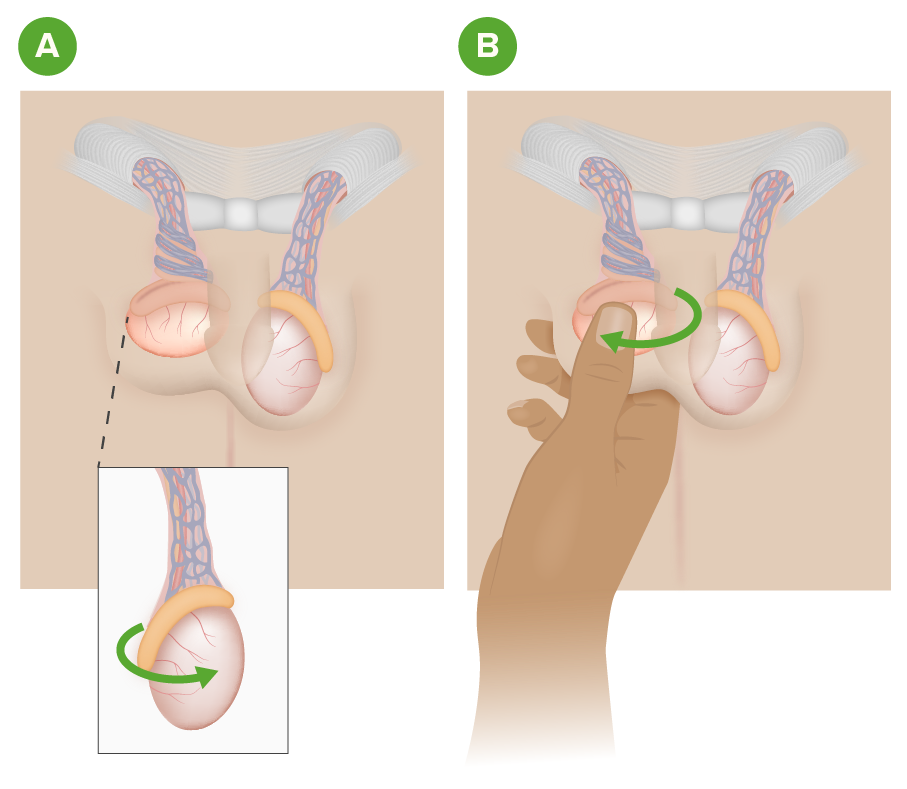
Manual testicular detorsion:
Image A depicts a right testicular torsion.
Image B illustrates the manual detorsion method of grasping and rotating the affected testicle with the “open book technique” from the medial to lateral position.