Cryptorchidism is one of the most common congenital anomalies in young boys. Typically, this asymptomatic condition presents during a routine well-child examination where 1 or both testicles Testicles The testicles, also known as the testes or the male gonads, are a pair of egg-shaped glands suspended within the scrotum. The testicles have multiple layers: an outer tunica vaginalis, an intermediate tunica albuginea, and an innermost tunica vasculosa. The testicles are composed of testicular lobules and seminiferous tubules. Testicles: Anatomy are not palpable in the scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy. Diagnosis depends on physical exam and ultrasound is performed only when other disorders are suspected. Treatment is dependent on patient age and testis position. In boys with persistent undescended testis by age 6 months, the condition is unlikely to spontaneously resolve. If the testis is palpable but not in the dependent intrascrotal location, an orchiopexy (bringing the testicle to the scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy) is preferred. If the testis is non-palpable, a diagnostic laparoscopy Diagnostic Laparoscopy Laparotomy and Laparoscopy is needed to inspect for an intra-abdominal testis, which requires a staged Fowler-Stephen’s orchiopexy.
Last updated: Nov 18, 2024
Cryptorchidism is the absence of 1 or both testicles Testicles The testicles, also known as the testes or the male gonads, are a pair of egg-shaped glands suspended within the scrotum. The testicles have multiple layers: an outer tunica vaginalis, an intermediate tunica albuginea, and an innermost tunica vasculosa. The testicles are composed of testicular lobules and seminiferous tubules. Testicles: Anatomy in the scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy. Cryptorchid testis (“hidden testis”) may be undescended or absent (atrophied).
Pathogenesis overall is not well understood but is affected by hormonal and anatomical embryologic factors.
Normal mechanical descent:
Defective mechanisms in the different phases of descent:
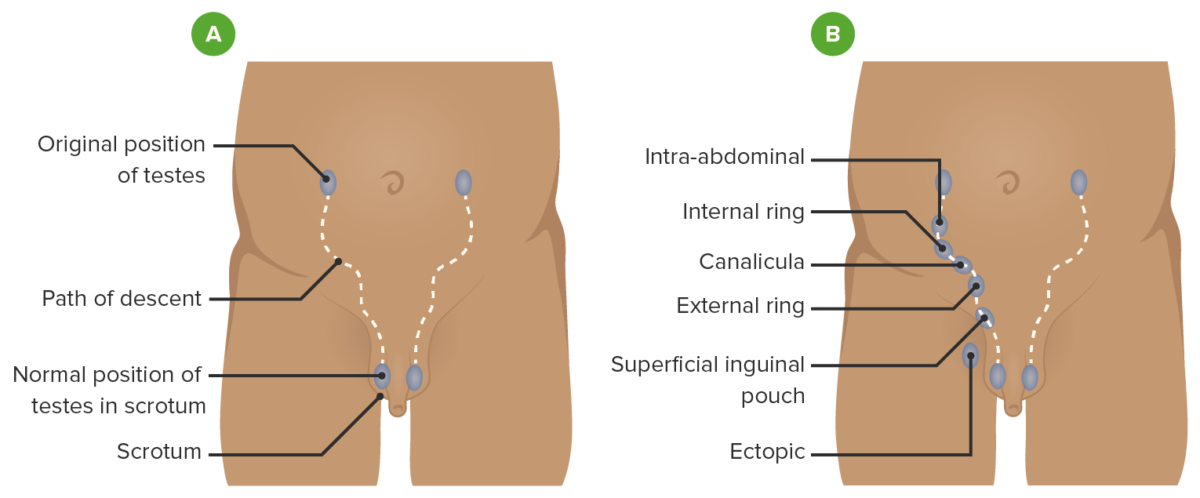
Path of descent of the testis
A: normal path the testis follows as it descends into the scrotum
B: possible locations where an undescended testis can be found

Undescended testis: a nonpalpable left testicle and a palpable right testicle in the scrotal position
Image: “Case 2” by Department of Endocrinology, Mohammed VI Hospital, Medical School, Mohammed the First University, 60 000 Oujda, Morocco. License: CC BY 3.0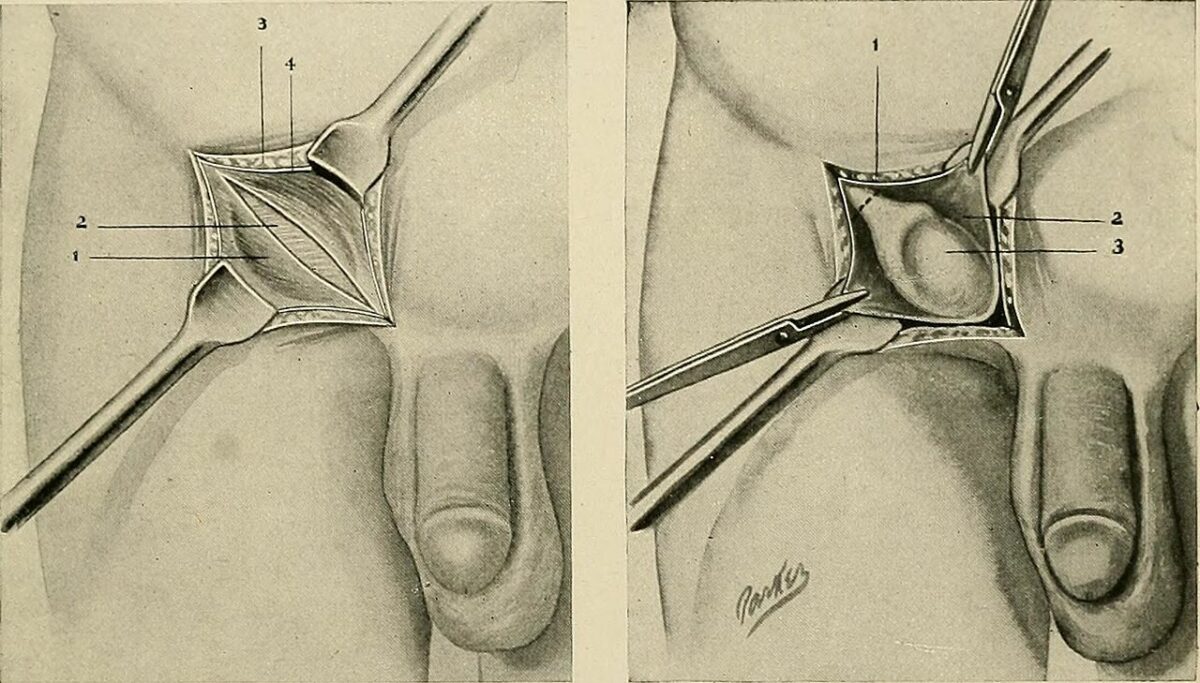
Surgical correction of undescended testis
Left: inguinal region dissection
Right: inguinal approach to orchiopexy with testicle exposed in inguinal canal