Sudden infant death syndrome (SIDS) describes the sudden death of an otherwise healthy infant (< 1 year of age) with no identifiable cause. Sudden infant death syndrome is the leading cause of death in children between 1 and 12 months of age in the United States. Sudden infant death syndrome is a diagnosis of exclusion and can only be confirmed after other causes of death have been ruled out with a thorough medical history and autopsy. Providing parents with preventative education is key to reducing the risk of SIDS. Preventative measures include having infants sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep supine, on firm surfaces, with no clutter in their crib.
Last updated: Dec 8, 2024
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of a child in infancy (< 1 year of age) with no identifiable cause after examination, clinical case review, and autopsy.
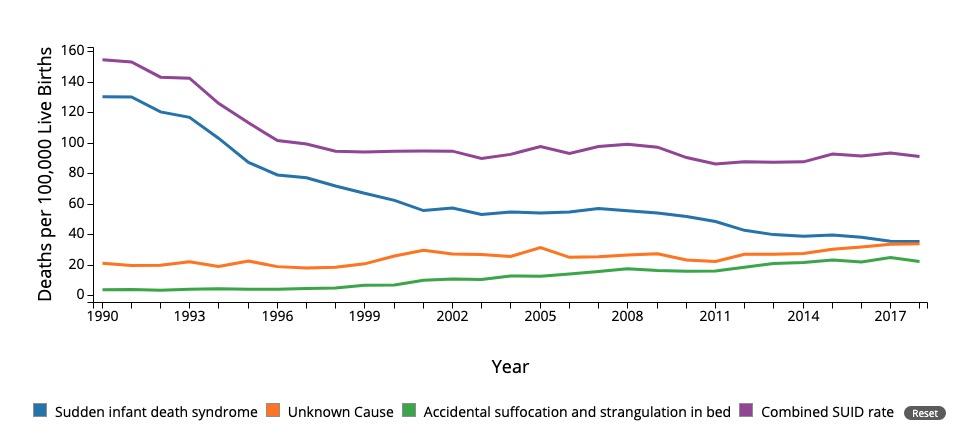
Mortality due to sudden infant death syndrome (SIDS) and other causes. Notice the decrease since 1994 due to public interventions including the “back to sleep” campaign.
SUID: Sudden unexpected infact death
The most likely cause of SIDS involves a multifactorial genesis in particularly vulnerable babies, in which internal and external factors work together.
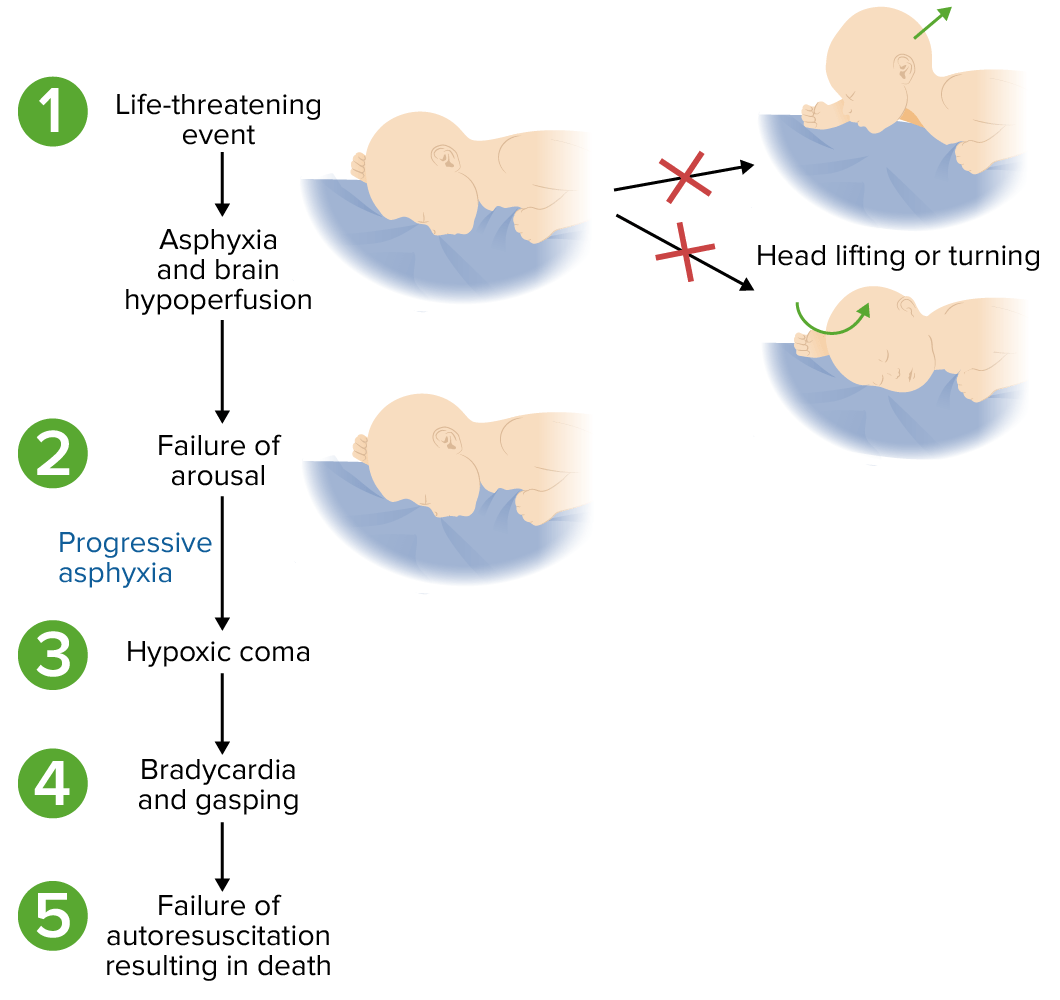
Possible pathophysiology of sudden infant death syndrome (SIDS):
In some vulnerable infants, an event may lead to hypoxia and/or hypercapnia. The inability to detect or respond leads to progressive physiologic consequences and death.
| Category | Mechanisms | Example effects on infant |
|---|---|---|
| Central nervous system Central nervous system The main information-processing organs of the nervous system, consisting of the brain, spinal cord, and meninges. Nervous System: Anatomy, Structure, and Classification | Reduced detection and response to rising CO2 and falling O2, increasing vulnerability to apnea and hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage | |
| Genetic & autonomic | Diminished ability to initiate protective breathing efforts or adjust heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology in response to low oxygen | |
| Cardiac anomalies | Predisposition to fatal heart rhythm disturbances, especially under stress or hypoxic conditions | |
| Metabolic factors | Difficulty maintaining adequate energy supplies, exacerbating the impact of respiratory or cardiac stress | |
| Infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease & immune response | Heightened risk of respiratory failure Respiratory failure Respiratory failure is a syndrome that develops when the respiratory system is unable to maintain oxygenation and/or ventilation. Respiratory failure may be acute or chronic and is classified as hypoxemic, hypercapnic, or a combination of the two. Respiratory Failure and inability to recover from hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage due to excessive or dysregulated inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation |
SIDS is a diagnosis of exclusion that can be assigned only after:
The primary focus of management is providing an accurate post-mortem diagnosis as well as emotional and psychological support to the parents. Parents and family members should also be:
Parental education is key to preventing SIDS. As noted above, many of the risk factors are modifiable and can be prevented. Parental education includes:
The following conditions are natural causes of death to be distinguished from SIDS: