Donovanosis (also known as granuloma inguinale) is an STD caused by Klebsiella granulomatis and is mainly seen in tropical regions. The condition is characterized by chronic, progressive, ulcerating disease mostly affecting the genital region. The patient presents with painless nodular lesions that ulcerate, commonly with a "beefy-red" base. There is no associated inguinal lymphadenopathy Inguinal Lymphadenopathy Lymphadenopathy. Diagnosis is via history, clinical findings, and tissue smear or biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma showing Donovan bodies, which are intracellular inclusion bodies inside macrophages Macrophages The relatively long-lived phagocytic cell of mammalian tissues that are derived from blood monocytes. Main types are peritoneal macrophages; alveolar macrophages; histiocytes; kupffer cells of the liver; and osteoclasts. They may further differentiate within chronic inflammatory lesions to epithelioid cells or may fuse to form foreign body giant cells or langhans giant cells. Innate Immunity: Phagocytes and Antigen Presentation. Treatment is with a prolonged course of antibiotics until lesions are healed, with monitoring for recurrence.
Last updated: May 16, 2024
Donovanosis, or granuloma inguinale, is an STD characterized by chronic progressive ulcers affecting the genital region.

Ulcerative lesions of Donovanosis: a patient’s left inguinal region, revealing the presence of a number of ulcerative erythematous lesions, which were determined to be due to a case of donovanosis
Image: “5365” by CDC/Dr. Tabua, Chief Medical Officer from Port Moresby, Papua, New Guinea. License: Public Domain
An ulcerogranulomatous lesion due to donovanosis:
Note the beefy-red base at the frenulum of the penis.
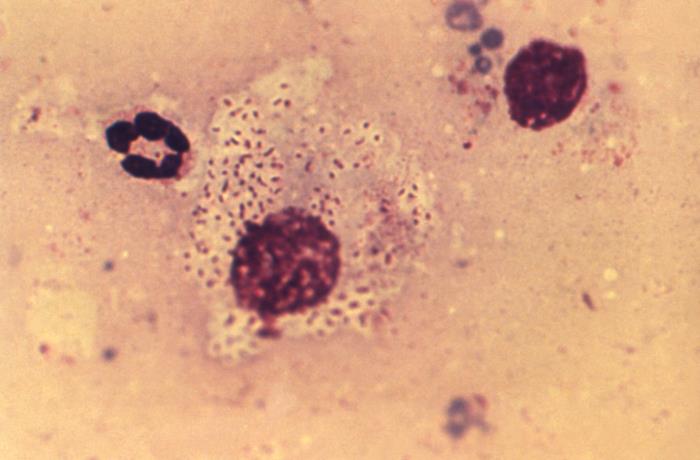
Tissue sample from an ulcer: a WBC that contained the pathognomonic finding of Donovan bodies, which were encapsulated, gram-negative rods, representing the responsible bacterium Klebsiella granulomatis
Image: “18899” by CDC/Susan Lindsley. License: Public Domain