Lentigo maligna is melanoma Melanoma Melanoma is a malignant tumor arising from melanocytes, the melanin-producing cells of the epidermis. These tumors are most common in fair-skinned individuals with a history of excessive sun exposure and sunburns. Melanoma in situ, a precancerous Precancerous Pathological conditions that tend eventually to become malignant. Barrett Esophagus lesion that may progress to an invasive melanoma Melanoma Melanoma is a malignant tumor arising from melanocytes, the melanin-producing cells of the epidermis. These tumors are most common in fair-skinned individuals with a history of excessive sun exposure and sunburns. Melanoma (specifically lentigo maligna melanoma Melanoma Melanoma is a malignant tumor arising from melanocytes, the melanin-producing cells of the epidermis. These tumors are most common in fair-skinned individuals with a history of excessive sun exposure and sunburns. Melanoma subtype). This condition typically occurs in sun-damaged areas (e.g., face and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess) of elderly patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Lentigo maligna presents as a brown macule Macule Nonpalpable lesion < 1 cm in diameter Generalized and Localized Rashes with color variegation and asymmetrical borders that grow slowly. The lesion should be biopsied to confirm a diagnosis and surgical excision with a safety margin is the 1st-line treatment.
Last updated: Mar 28, 2025
Lentigo maligna (also known as Hutchinson melanotic freckle) is melanoma Melanoma Melanoma is a malignant tumor arising from melanocytes, the melanin-producing cells of the epidermis. These tumors are most common in fair-skinned individuals with a history of excessive sun exposure and sunburns. Melanoma in situ. This type of precancerous Precancerous Pathological conditions that tend eventually to become malignant. Barrett Esophagus lesion may progress to lentigo maligna melanoma Melanoma Melanoma is a malignant tumor arising from melanocytes, the melanin-producing cells of the epidermis. These tumors are most common in fair-skinned individuals with a history of excessive sun exposure and sunburns. Melanoma.

Lentigo maligna: an asymmetric brown macule with color variegation present on the left cheek
Image: “Lentigo maligna” by kilbad. License: CC BY 3.0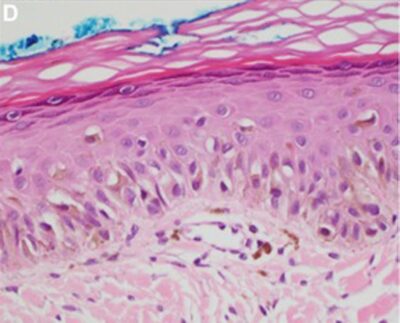
Lentigo maligna:
A nest of atypical melanocytes can be noted. The basement membrane is intact. Therefore, this lesion is lentigo maligna (in situ).
Surgical excision:
Nonsurgical:
Patient education: