Blunt chest trauma is a non-penetrating traumatic injury to the thoracic cavity. Thoracic traumatic injuries are classified according to the mechanism of injury as blunt or penetrating injuries Penetrating injuries Wounds caused by objects penetrating the skin. Genitourinary Trauma. Different structures can be injured including the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy ( ribs Ribs A set of twelve curved bones which connect to the vertebral column posteriorly, and terminate anteriorly as costal cartilage. Together, they form a protective cage around the internal thoracic organs. Chest Wall: Anatomy, sternum Sternum A long, narrow, and flat bone commonly known as breastbone occurring in the midsection of the anterior thoracic segment or chest region, which stabilizes the rib cage and serves as the point of origin for several muscles that move the arms, head, and neck. Chest Wall: Anatomy), lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy, heart, major blood vessels, and the esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy. The extent and specific type of thoracic traumatic injury can be identified by a proper history and physical examination supported by adequate imaging studies. Management depends on the specific type of injury.
Last updated: Jul 26, 2023
Blunt chest trauma is injury and consequential pathology arising from application of significant kinetic forces to the chest that do not cause penetration Penetration X-rays of the thoracic cavity.
The chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy is composed of:
The chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy‘s function is to absorb trauma and protect underlying vulnerable structures from damage:
The suspected mechanism of injury should prompt suspicion for blunt chest trauma. Treatment algorithms and guidelines direct evaluation:
While the initial approach to stabilizing a patient with chest trauma is standardized, further imaging and testing is dependent on the injury discovered during the initial assessment.
Choosing the best imaging studies depends on the patient’s hemodynamic stability:
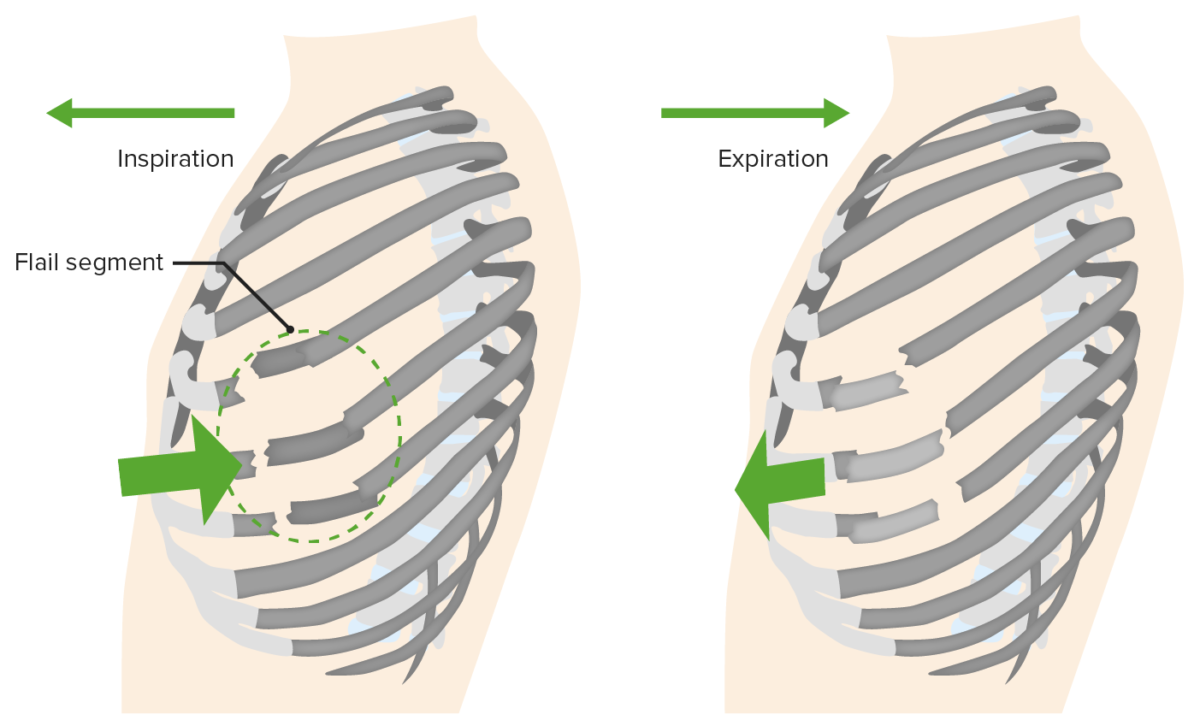
Flail chest: fractured ribs that move paradoxically in comparison to the chest wall
Image by Lecturio.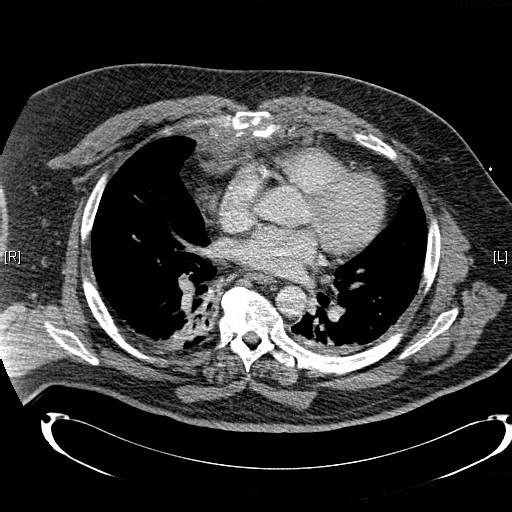
Chest CT showing comminuted sternal fracture:
Fractures of the sternum can occur during high-energy chest traumas and can be simple (meaning a single fracture) or comminuted (where the bone breaks into multiple fragments). Usually, fractures of the sternum are associated with underlying injury of the lungs or heart.
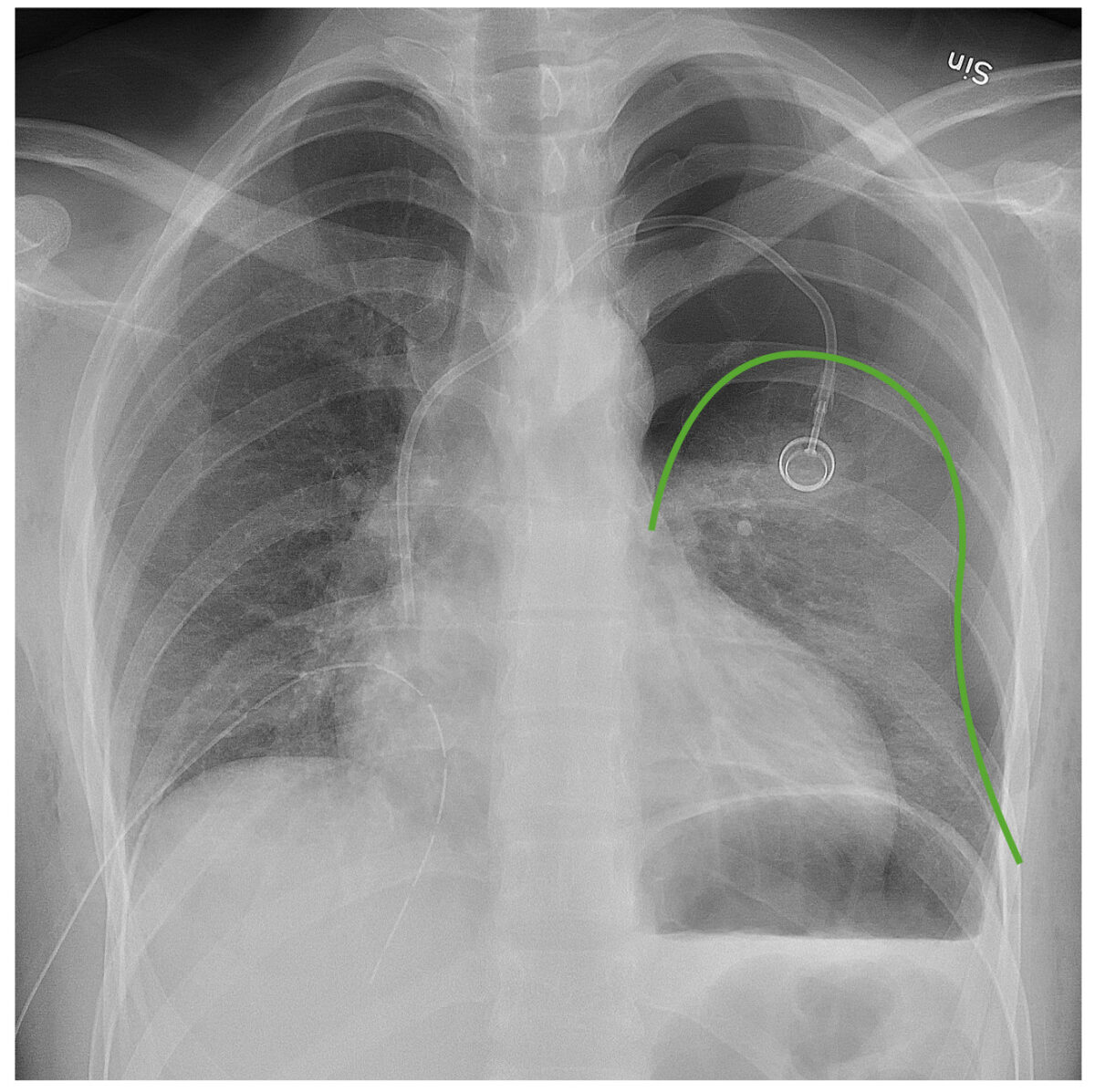
Chest radiograph demonstrating a left pneumothorax:
The green line outlines the pleural line. Notice the lack of bronchovascular markings beyond that line.

AP chest X-ray revealing evidence of bilateral lung contusions and left subcutaneous emphysema (Panel A): Chest CT confirmed both the lung contusions and the subcutaneous emphysema and demonstrated a left sided pneumothorax not initially appearing on the anteroposterior chest X-ray (Panel B).
Image: “Bilateral lung contusions” by Departement of Internal Medicine, Mercy Hospital and Medical Center, Chicago, Illinois, USA. License: CC BY 2.0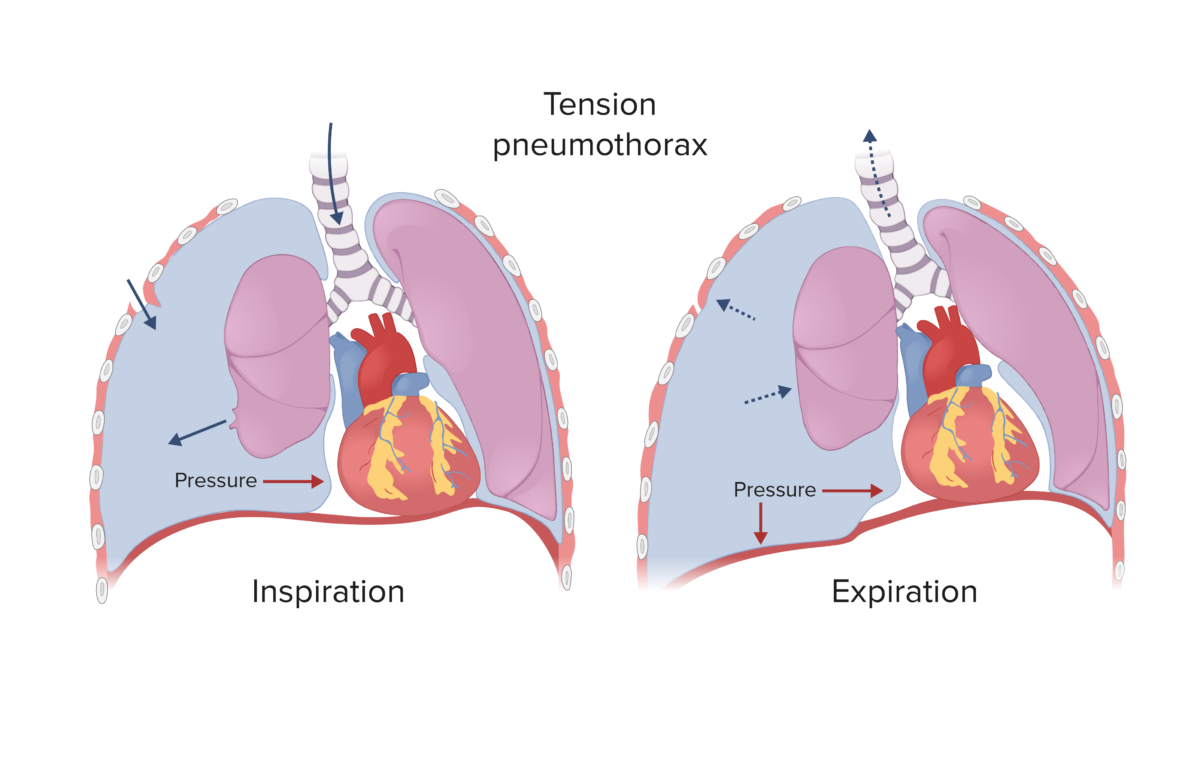
Tension pneumothorax:
Spontaneous and traumatic pneumothoraces can develop into a tension pneumothorax if the defect that allows air into the pleural space becomes a 1-way valve (air enters during inspiration, but cannot escape during expiration), which causes rising pressure in the pleural cavity, shifting the mediastinum to the contralateral side.
Tracheobronchial tear
Injury to the trachea or the bronchi is often seen with high energy chest trauma.
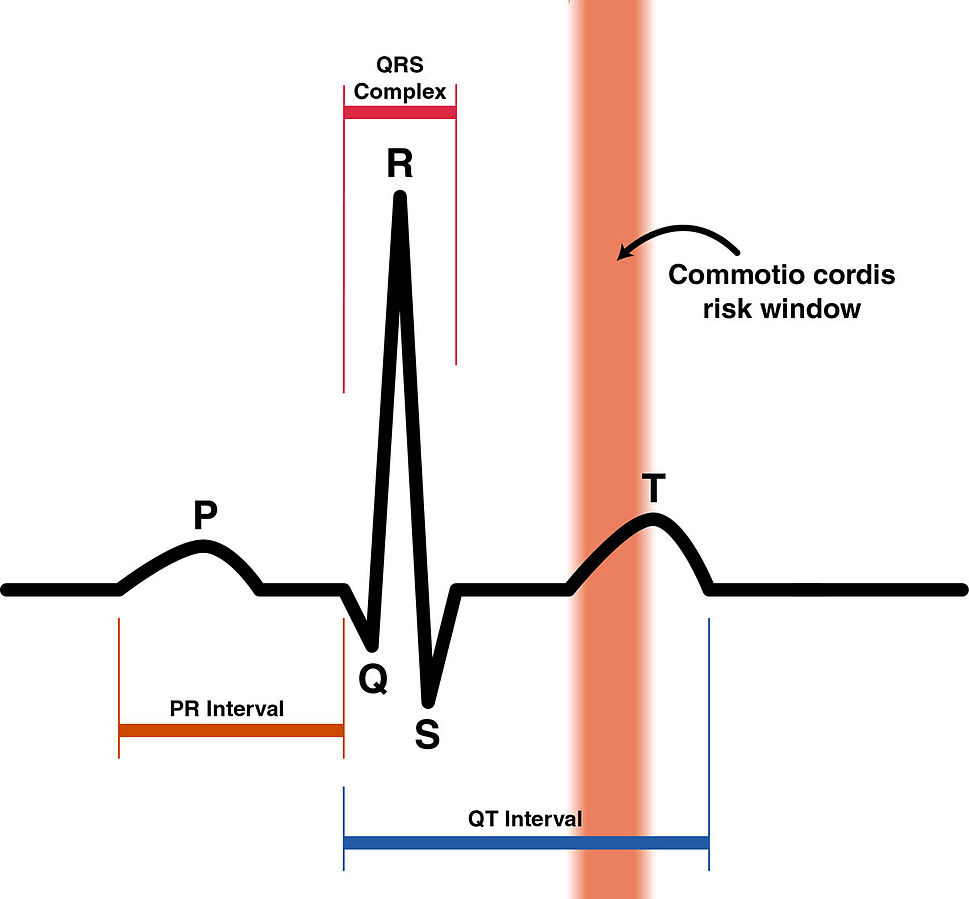
Commotio cordis risk window:
Commotio cordis is a cardiac arrest that occurs when the chest over the heart is struck during the portion of the cardiac cycle corresponding with the upstroke of the T wave on ECG.
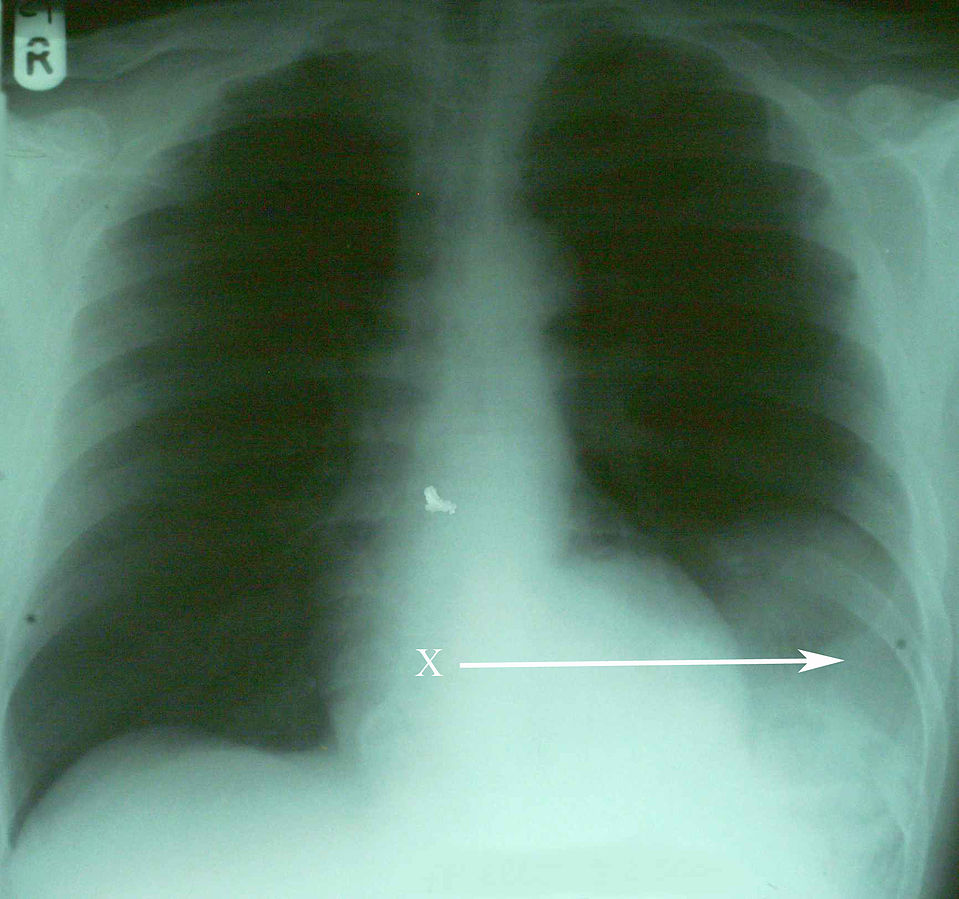
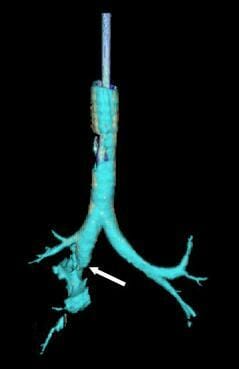
Diaphragmatic rupture:
Rupture of the diaphragm secondary to chest trauma seen on chest X-ray as bowel contents in the thoracic cavity. Arrow labeled X points to portion of the spleen herniating into the chest cavity through a diaphragmatic rupture.