Multitrauma occurs when 2 or more traumatic injuries occur in at least 2 areas of the body. A systematic management approach is necessary for individuals who have undergone trauma to maximize outcomes and reduce the risk of undiscovered injuries. Assessment of multitrauma starts with a primary survey Primary Survey Thoracic Trauma in Children followed by the A-B-C-D-E scheme, involving securing of the airway Airway ABCDE Assessment (A), and evaluating breathing (B), circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment (C), recognition of neurologic deficits Neurologic Deficits High-Risk Headaches or disability Disability Determination of the degree of a physical, mental, or emotional handicap. The diagnosis is applied to legal qualification for benefits and income under disability insurance and to eligibility for social security and workman's compensation benefits. ABCDE Assessment (D), and exposure to environmental control (E). Once the primary survey Primary Survey Thoracic Trauma in Children is completed, a secondary survey Secondary Survey ABCDE Assessment is performed to obtain pertinent history and nature of the trauma based on a thorough examination and diagnostic studies. The A-B-C-D-E approach is crucial for the overall stabilization, treatment, and identification Identification Defense Mechanisms of any missed injuries.
Last updated: Jan 24, 2023
Multitrauma or polytrauma is defined as 2 or more severe injuries in at least 2 areas of the body (with at least 1 life-threatening injury).
Trauma is a leading cause of mortality Mortality All deaths reported in a given population. Measures of Health Status and morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status globally.
Hemorrhage is the most common preventable cause of mortality Mortality All deaths reported in a given population. Measures of Health Status in trauma.
Factors associated with poor outcomes in trauma:
Primary survey Primary Survey Thoracic Trauma in Children is the initial evaluation used to identify and manage life-threatening injuries in an individual with trauma. The survey consists of 5 assessments performed in a stepwise manner: airway, breathing, circulation, disability, and exposure.

Application of the backboard and C-collar by emergency medical services (EMS) in the field:
If the affected individual arrives in a personal vehicle, the C-collar is applied during the airway (A) portion of the primary survey.
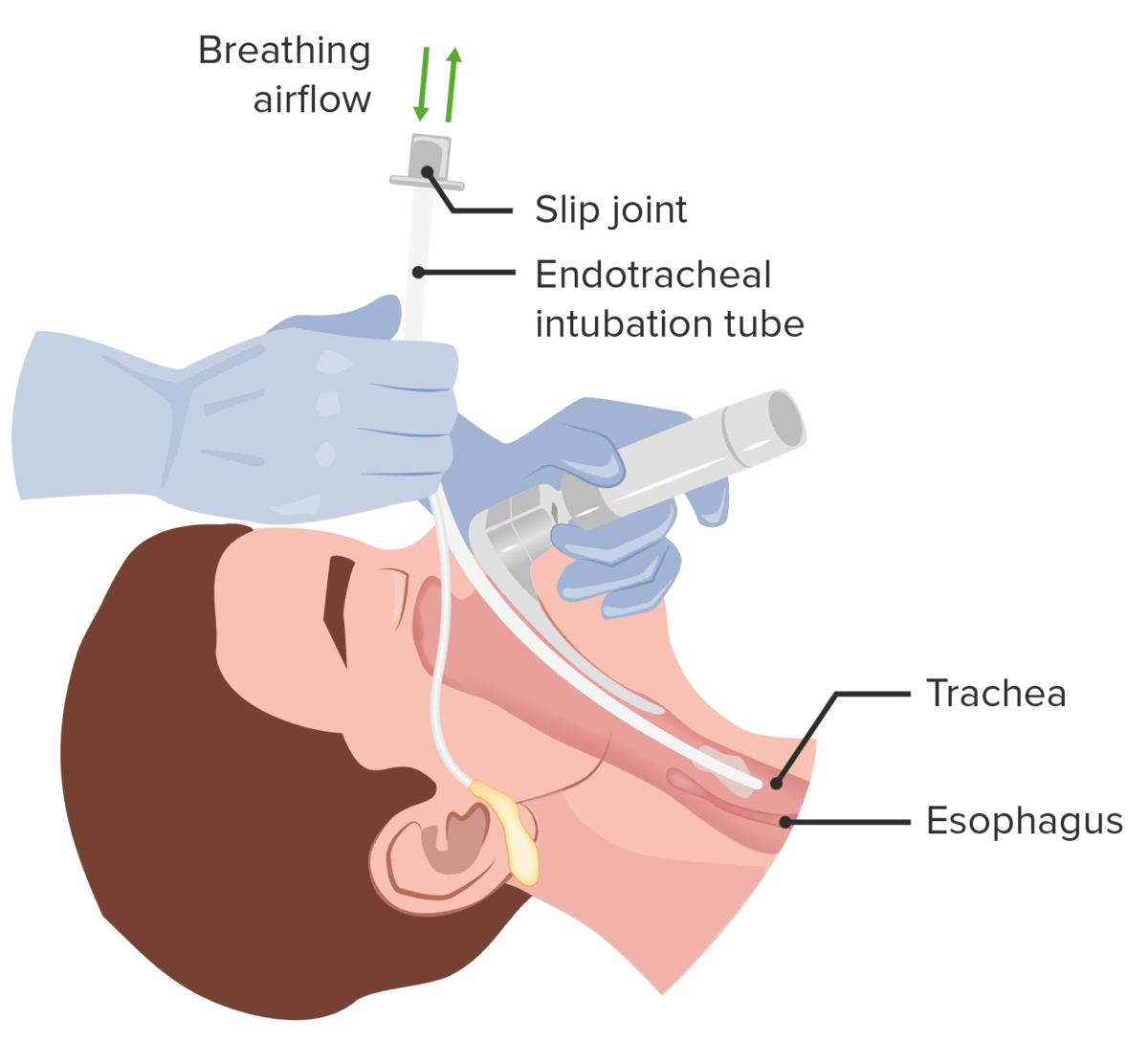
Airway management: establishing a definite airway via insertion of an endotracheal tube
Image by Lecturio.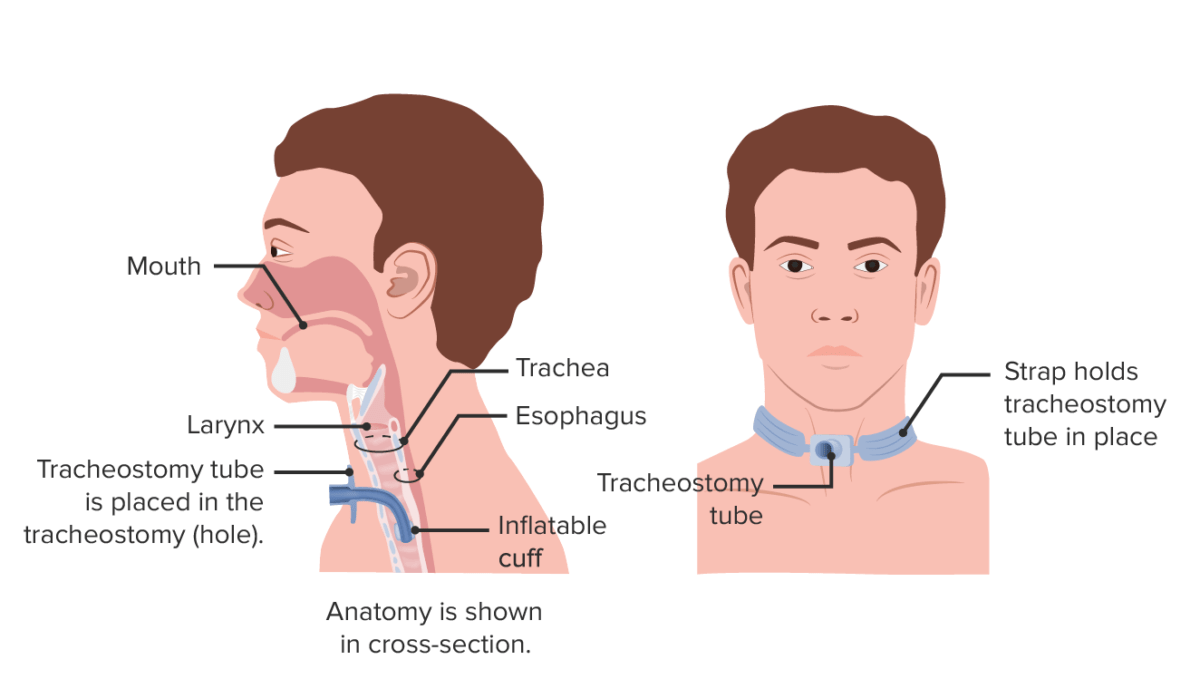
Tracheostomy:
Figure A shows a side view of the neck and the correct placement of a tracheostomy tube in the trachea or windpipe. Figure B shows an external view of an individual with a tracheostomy tube.
Disability Disability Determination of the degree of a physical, mental, or emotional handicap. The diagnosis is applied to legal qualification for benefits and income under disability insurance and to eligibility for social security and workman’s compensation benefits. ABCDE Assessment assessment:
| Feature | Response | Score |
|---|---|---|
| Eye opening | Open spontaneously | 4 |
| Open to verbal commands | 3 | |
| Open to pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 2 | |
| No eye opening | 1 | |
| Verbal response | Oriented and appropriate | 5 |
| Disoriented but conversant | 4 | |
| Nonsensical words | 3 | |
| Moaning | 2 | |
| Silent | 1 | |
| Motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology response | Follows commands | 6 |
| Localizes pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 5 | |
| Withdraws from pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | 4 | |
| Flexor posturing | 3 | |
| Extensor posturing Extensor posturing A condition characterized by abnormal posturing of the limbs that is associated with injury to the brainstem. This may occur as a clinical manifestation or induced experimentally in animals. The extensor reflexes are exaggerated leading to rigid extension of the limbs accompanied by hyperreflexia and opisthotonus. This condition is usually caused by lesions which occur in the region of the brainstem that lies between the red nuclei and the vestibular nuclei. In contrast, decorticate rigidity is characterized by flexion of the elbows and wrists with extension of the legs and feet. The causative lesion for this condition is located above the red nuclei and usually consists of diffuse cerebral damage. Increased Intracranial Pressure (ICP) | 2 | |
| Flaccid | 1 |
The goal of this step is to evaluate and manage negative environmental effects:
The goal of the secondary survey Secondary Survey ABCDE Assessment is to rapidly and thoroughly examine the affected individual from head to toe and identify all potentially significant injuries.
For focused history, recall the mnemonic “AMPLE”:
Pertinent history, thorough physical examination, and appropriate diagnostic studies help avoid missed injuries such as:
The tables below summarize the different mechanisms of trauma and their associated specific injuries.
| Mechanism of injury | Potential associated injuries |
|---|---|
| Head-on collision |
|
| Rear-end collision |
|
| Ejected from vehicle | Spinal injuries |
| Windshield damage |
|
| Steering wheel damage | Thoracic injuries |
| Dashboard involvement/damage |
|
| Mechanism of injury | Potential associated injuries |
|---|---|
| Low speed (braking automobile) |
|
| High speed | Waddle’s triad (in pediatric pedestrians):
|
| Mechanism of injury | Potential associated injuries |
|---|---|
| Automobile related |
|
| Nonautomobile-related |
|
| Mechanism of injury | Potential associated injuries |
|---|---|
| Vertical impact |
|
| Horizontal impact |
|