Penetrating chest injuries (PCIs) are caused by an object puncturing the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy. Penetrating chest injuries can be high velocity, such as with gunshot wounds (GSWs); medium velocity, such as with pellet gunshots; or low velocity, such as with stab wounds Stab wounds Penetrating wounds caused by a pointed object. Penetrating Abdominal Injury. Penetrating chest injuries have a higher mortality Mortality All deaths reported in a given population. Measures of Health Status rate than blunt chest injuries but are less common. Performing the standardized trauma evaluation (primary and secondary surveys), as well as ordering proper imaging, is critical to determining the diagnosis and aiding in management decisions. The majority of PCIs do not require major surgery and can be managed by observation or tube thoracostomy Tube Thoracostomy Surgical procedure involving the creation of an opening (stoma) into the chest cavity for drainage; used in the treatment of pleural effusion; pneumothorax; hemothorax; and empyema. Thoracic Surgery, although surgical repair of injuries may be needed.
Last updated: Dec 5, 2022
A penetrating chest injury Chest Injury Pediatric Chest Abnormalities (PCI) can be defined as any trauma that violates the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy in an area bordered superiorly by the lower neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess and inferiorly by the lower costal margin.
Mechanism of injury categorized by object’s velocity:
Penetrating object’s ability to produce tissue damage is dependent on the following:
All trauma patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship should be checked for penetrating chest trauma. Treatment algorithms and guidelines (primary and secondary survey Secondary Survey ABCDE Assessment) direct the evaluation.
While the initial approach to stabilizing a patient with chest trauma is standardized by performing the primary and secondary surveys, further imaging and testing are dependent on the injury discovered during the initial assessment.
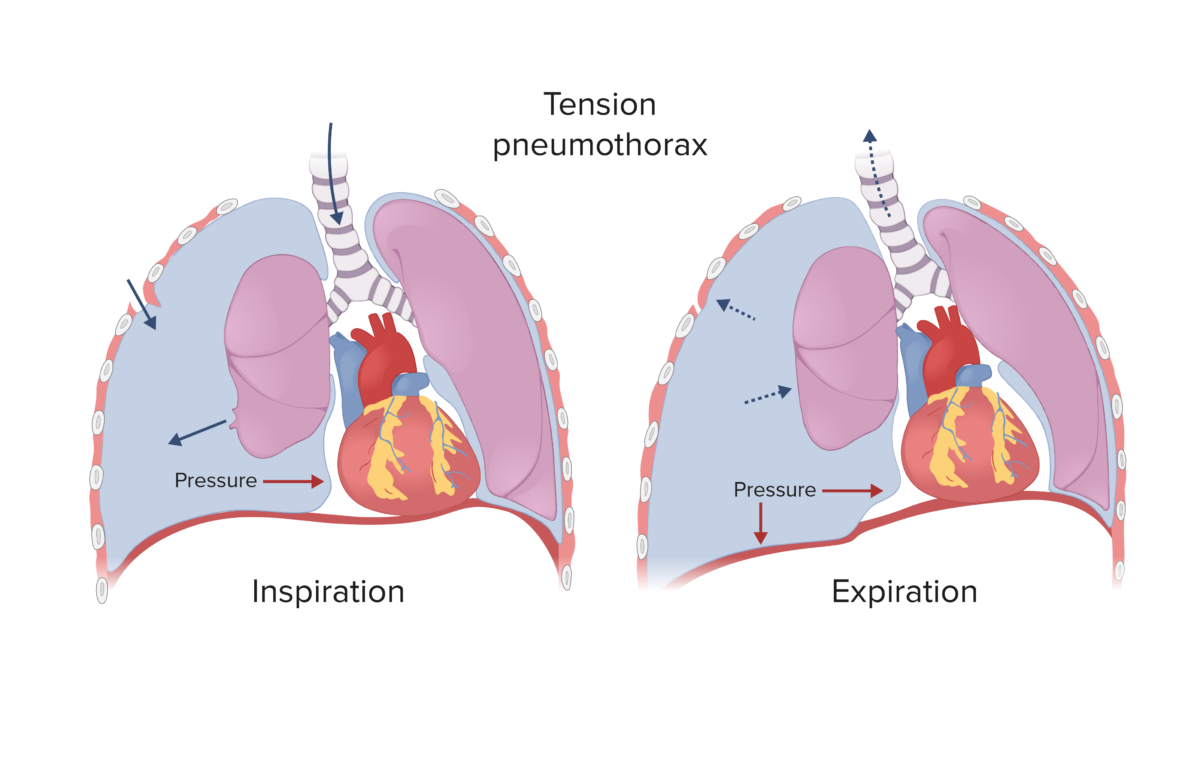
Tension pneumothorax:
Spontaneous and traumatic pneumothoraces can develop into a tension pneumothorax if the defect which allows air into the pleural space becomes a 1-way valve (air enters during inspiration, but cannot escape during expiration). This process causes rising pressure in the pleural cavity, shifting the mediastinum to the contralateral side.
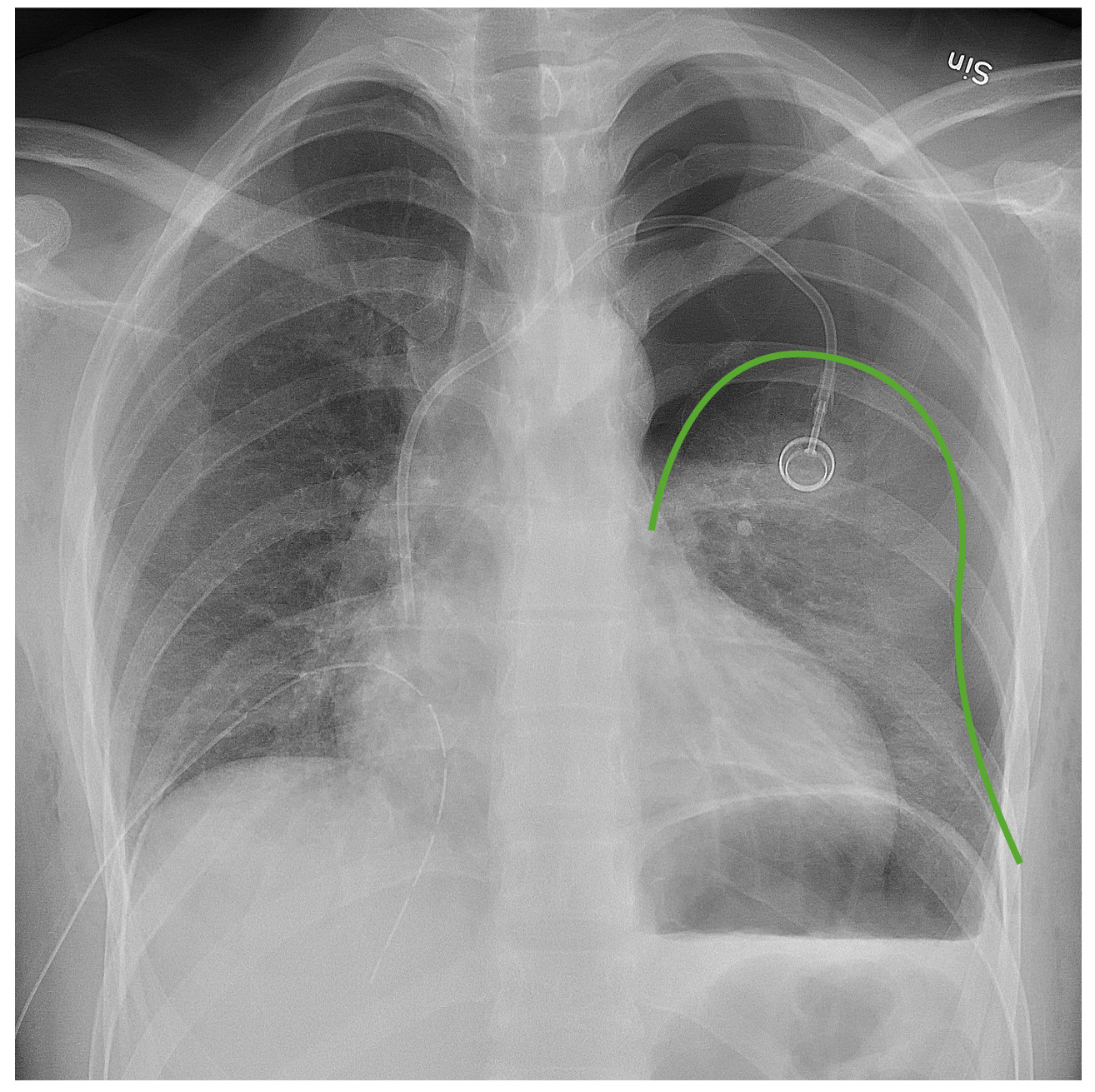
Chest radiograph demonstrating a left pneumothorax:
The green line outlines the pleural line. Notice the lack of bronchovascular markings beyond that line.

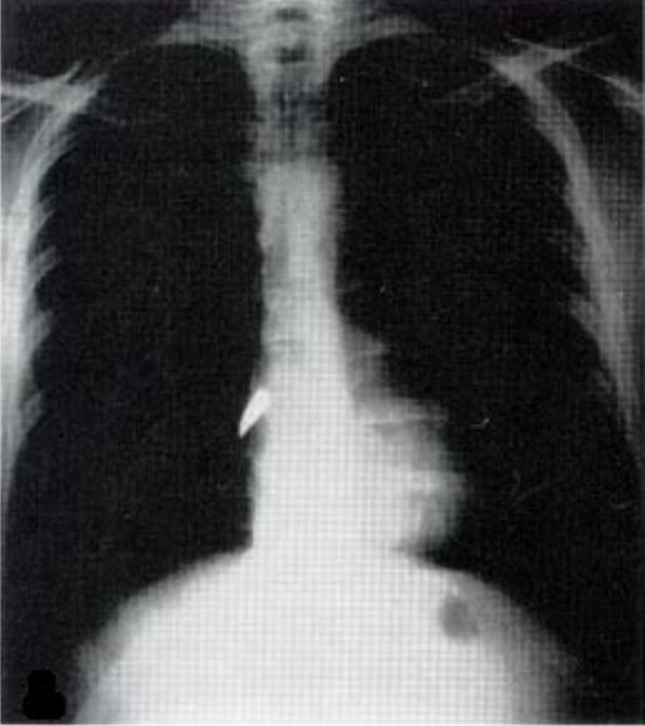
A: Anteroposterior (AP) chest X-ray revealing evidence of bilateral lung contusions and left subcutaneous emphysema. B: Chest CT confirmed both the lung contusions and the subcutaneous emphysema and demonstrated a left-sided pneumothorax not initially appearing on the AP chest X-ray.
Image: “Bilateral lung contusions” by the Department of Internal Medicine, Mercy Hospital and Medical Center, Chicago, Illinois, USA. License: CC BY 2.0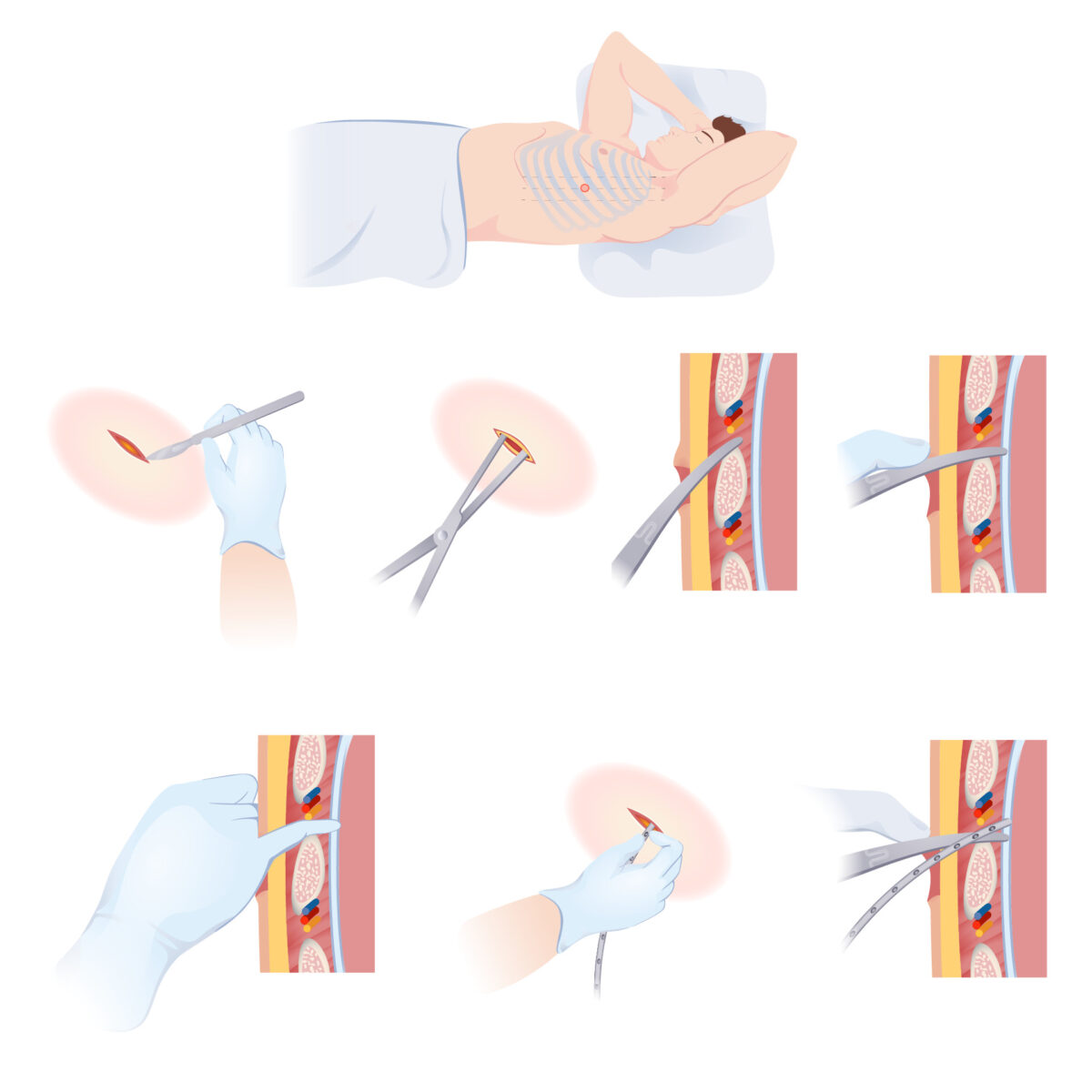
Stepwise illustration of how to insert a chest tube to drain a fluid accumulation from the pleural space
Image by Lecturio.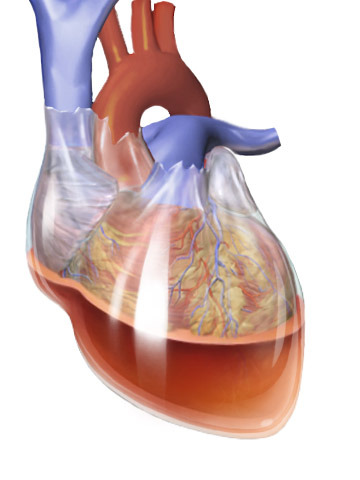
Hemopericardium:
Collection of fluid in the pericardial sac (in this case blood) can restrict the heart muscle, leading to impaired cardiac filling and cardiac output, also known as pericardial tamponade.
Chest X-ray image showing bullet in right side of heart:
The bullet has penetrated the right atrium. Laceration of the cardiac muscle is highly fatal.
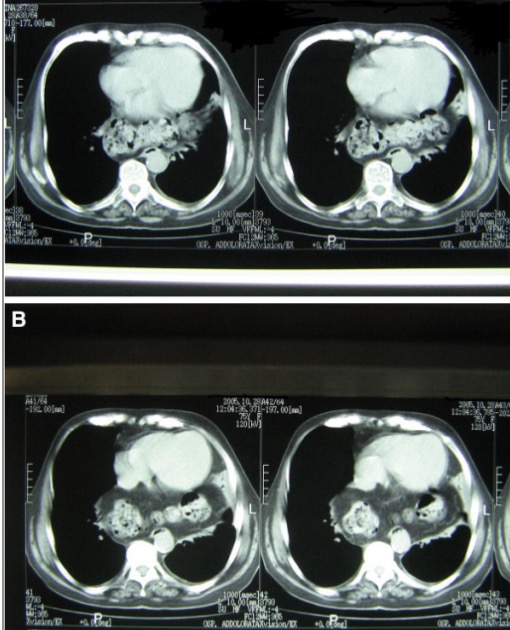
Axial CT scan of the chest:
Gas-filled large bowel loops are visible behind the heart, lying anteriorly to the spine and the aorta.