Heart failure (HF) is the complex condition resulting from a structural and/or functional inability of the heart to supply the normal cardiac output to meet metabolic needs. In HF, impaired ventricular filling or ejection of blood leads to fatigue, dyspnea, and fluid retention or edema. Echocardiography can confirm the diagnosis, providing information about the ejection fraction (EF) and the adequacy of ventricular filling and relaxation. Treatment is directed at the removal of excess fluid and decreasing oxygen demand of the heart. Prognosis depends on the underlying cause, compliance with medical therapy, and presence of comorbidities.
Last updated: May 16, 2024
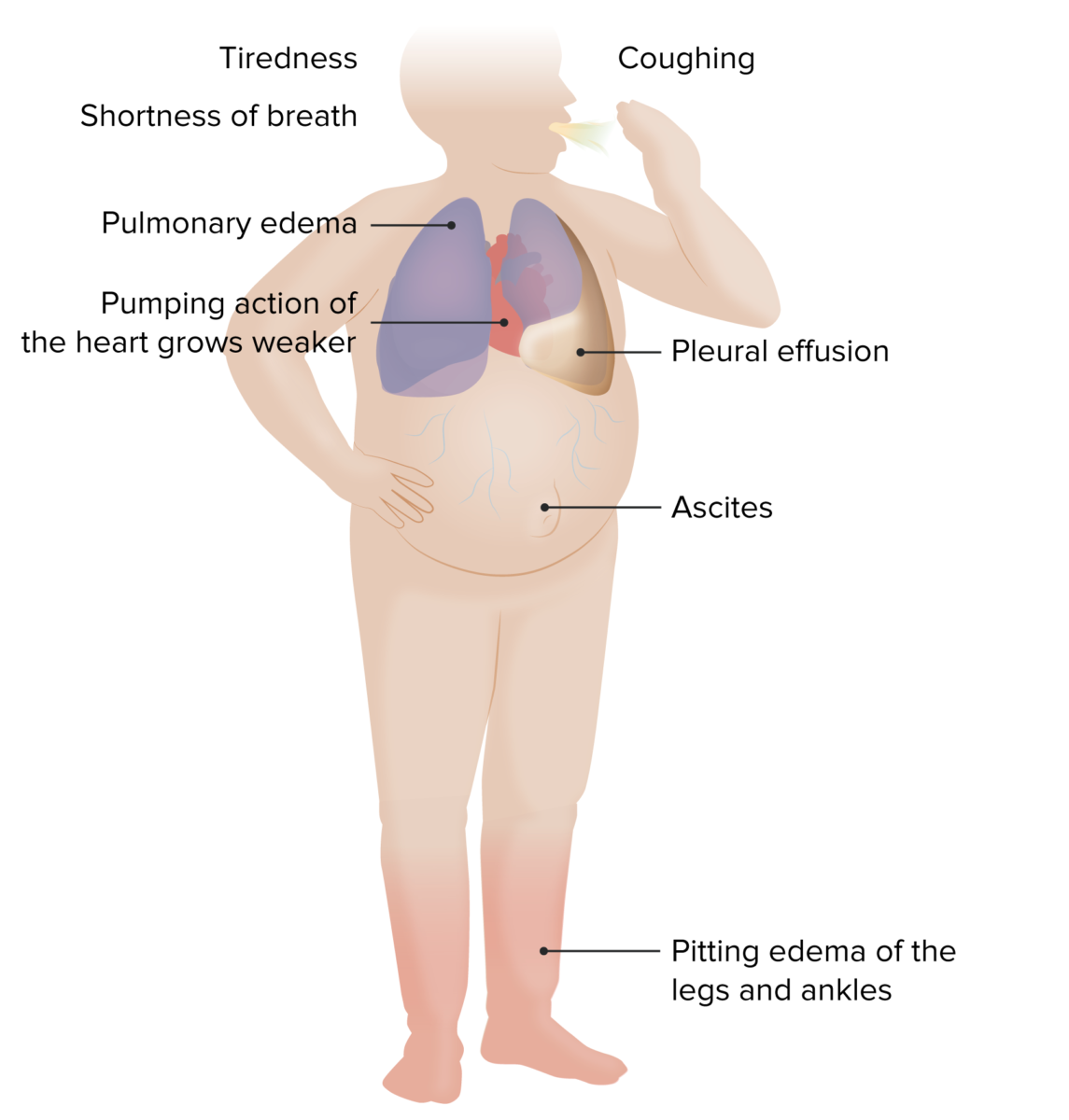
Symptoms/signs of HF
Image by Lecturio.| Test | Findings |
|---|---|
| BNP BNP A peptide that is secreted by the brain and the heart atria, stored mainly in cardiac ventricular myocardium. It can cause natriuresis; diuresis; vasodilation; and inhibits secretion of renin and aldosterone. It improves heart function. It contains 32 amino acids. Renal Sodium and Water Regulation/pro-BNP |
|
| Chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests |
|
| ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) |
|
| Echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA) |
|
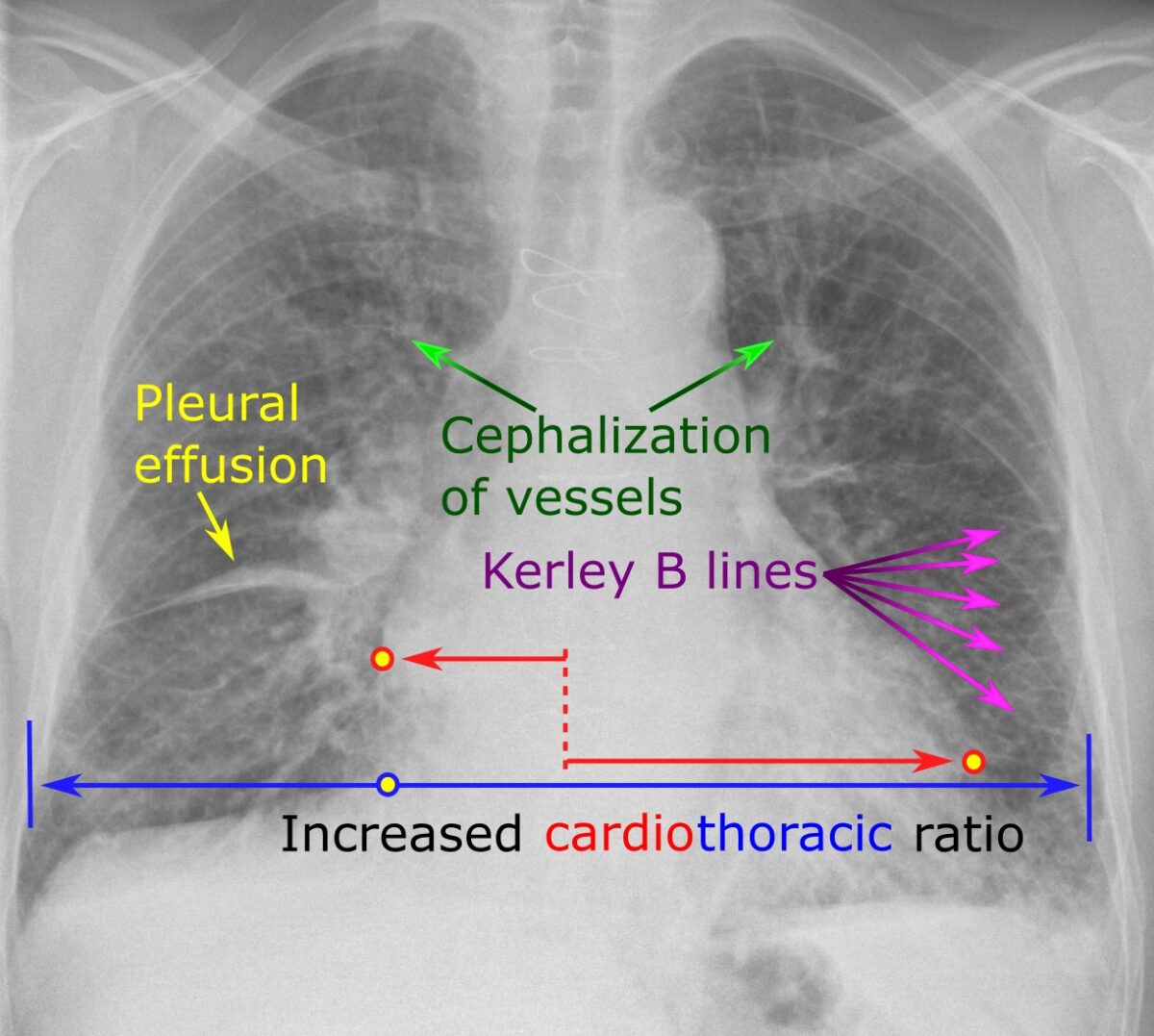
Chest radiograph showing characteristic findings of HF
Image: “Chest radiograph with signs of congestive heart failure – annotated” by Mikael Häggström – Own work. License: CC0 1.0A good mnemonic to remember these findings on CXR CXR X-ray visualization of the chest and organs of the thoracic cavity. It is not restricted to visualization of the lungs. Pulmonary Function Tests is ABCDE:
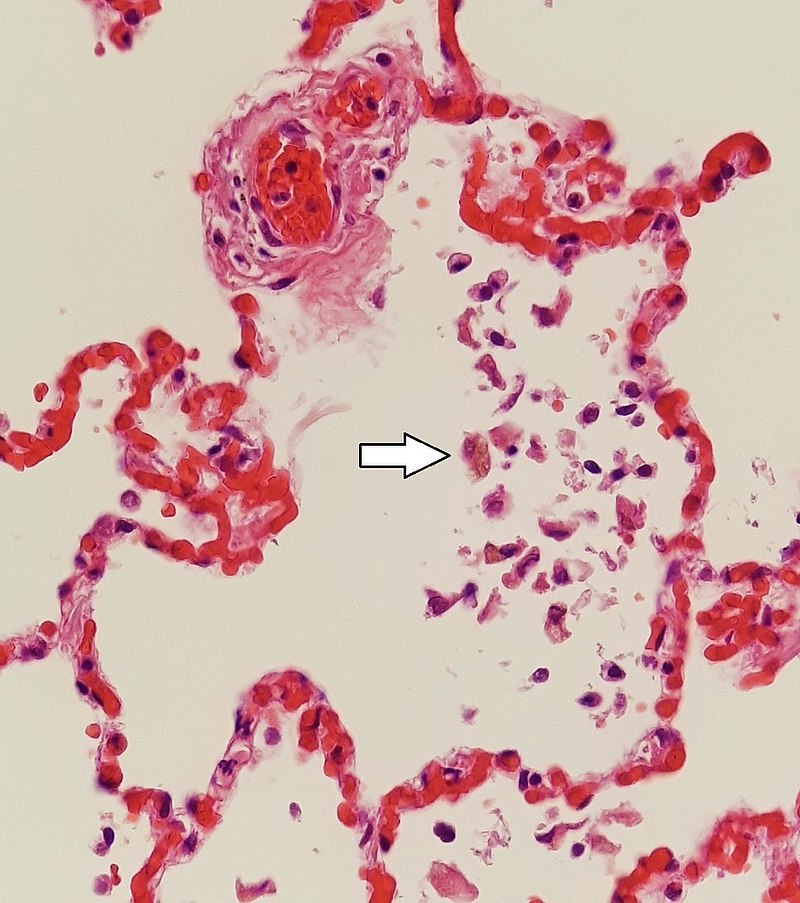
Small, congested capillaries may burst, leading to intra-alveolar hemorrhage that is marked by hemosiderin-laden macrophages (white arrow). Also known as “heart failure cells,” these cells indicate heart failure.
Image: “Siderophages (one indicated by white arrow) and pulmonary congestion, indicating left congestive heart failure” by Mikael Häggström, M.D. – Own work. License: CC0 1.0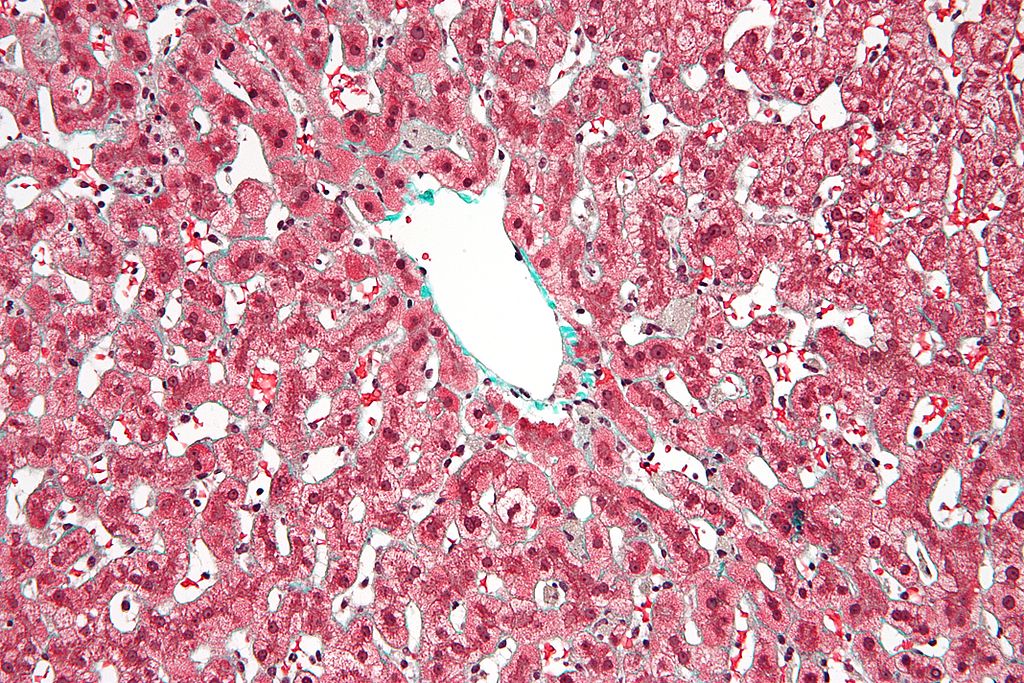
Micrograph of congestive hepatopathy or nutmeg liver due to venous congestion, usually due to heart failure. This may lead to cardiac cirrhosis.
Image: “Congestive hepatopathy high mag” by Nephron – Own work. License: CC BY-SA 3.0Acute decompensated HF causes respiratory distress, generally due to accumulation of fluid in the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy ( pulmonary edema Pulmonary edema Pulmonary edema is a condition caused by excess fluid within the lung parenchyma and alveoli as a consequence of a disease process. Based on etiology, pulmonary edema is classified as cardiogenic or noncardiogenic. Patients may present with progressive dyspnea, orthopnea, cough, or respiratory failure. Pulmonary Edema).
Initial treatment measures
To recall the management of acute heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) or exacerbation of HF, remember LMNOP:
Lifestyle modifications decrease morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status and mortality Mortality All deaths reported in a given population. Measures of Health Status in heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR).
Overview:
Drug classes in detail:
| Classification | Stage A | Stage B | Stage C | Stage D |
|---|---|---|---|---|
| At risk for HF | Structural heart disease, no symptoms | Structural heart disease, with symptoms | Advanced HF | |
| N/A | NYHA class I | NYHA class I–IV | NYHA IV | |
| General measures |
|
|||
| Initial drug therapy | As indicated by other risk factors |
|
|
|
| Secondary drug therapy (add-on) | N/A | N/A | In class II-IV, add:
|
|
Aside from cardiovascular complications such as arrhythmias and valvular dysfunction, long-term complications may include:
The following conditions are risk factors and/or causes of heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR):
References