Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles ( myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy) and impaired systolic and/or diastolic function in the absence of other heart disorders ( coronary artery Coronary Artery Truncus Arteriosus disease, hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, valvular disease, and congenital Congenital Chorioretinitis heart disease). The list of causes is extensive, ranging from familial disorders to underlying diseases and infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship often present with chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, palpitations Palpitations Ebstein’s Anomaly, and/or syncope Syncope Syncope is a short-term loss of consciousness and loss of postural stability followed by spontaneous return of consciousness to the previous neurologic baseline without the need for resuscitation. The condition is caused by transient interruption of cerebral blood flow that may be benign or related to a underlying life-threatening condition. Syncope. Some patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may be completely asymptomatic, while others may present with sudden cardiac death Sudden cardiac death Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest as the first sign of an underlying condition. Diagnosis is made through the use of ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) and cardiac imaging such as echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA) and cardiac MRI Cardiac MRI Imaging of the Heart and Great Vessels. Management involves medications typically used to treat heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), as well as implantable devices. In severe cases, heart transplantation Heart Transplantation The transference of a heart from one human or animal to another. Organ Transplantation may be necessary.
Last updated: May 16, 2024
Cardiomyopathies are diseases that affect the structure and function of the heart muscle ( myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy) in the absence of secondary causes (e.g., coronary artery Coronary Artery Truncus Arteriosus disease, hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, valvular disease, and congenital Congenital Chorioretinitis heart disease).
Causes vary:
Approximately ⅓ of cases have a genetic cause.
By morphology:
By etiology:
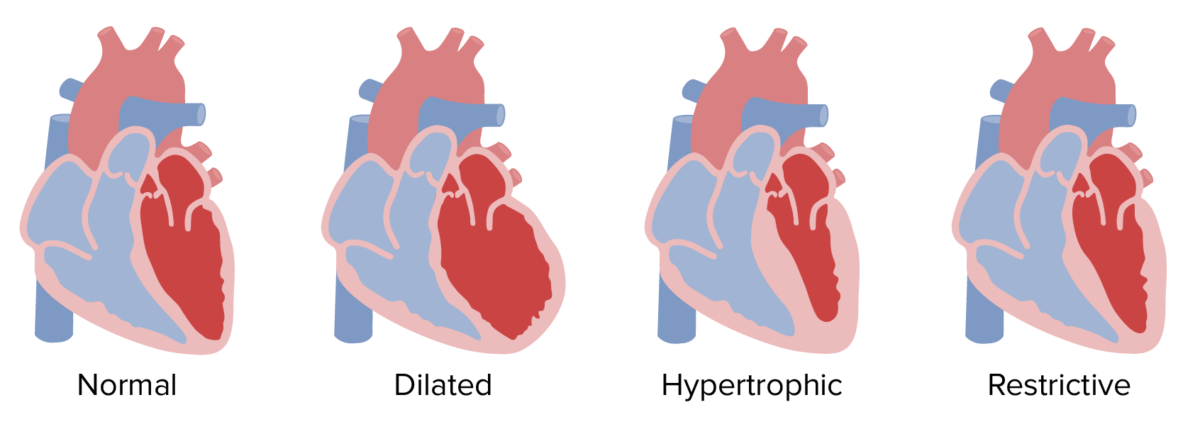
Morphological classification of cardiomyopathies
Image by Lecturio.Diagnostic approach varies based on the type of cardiomyopathy. Physicians Physicians Individuals licensed to practice medicine. Clinician–Patient Relationship must have a high index of suspicion for disorders of the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR).
Goals:
In cases refractory to treatment, heart transplantation Heart Transplantation The transference of a heart from one human or animal to another. Organ Transplantation may be indicated.
Complications:
| Dilated | Restrictive | Hypertrophic | Arrhythmogenic right ventricular CM | |
|---|---|---|---|---|
| Etiology |
|
|
|
|
| Clinical presentation |
|
|
|
|
| Physical exam findings |
|
|
|
|
| Ejection fraction Ejection fraction Cardiac Cycle | ↓ | ↓ or normal | ↑ or normal | ↓ |
| L ventricular diastolic dimension | ↑ | ↑ | ↓ | Normal |
| Left ventricular wall thickness | ↓ | Normal or ↑ | ↑↑ | Normal |
| Atrial size | ↑ | ↑ | ↑ | Normal |
| Diagnosis |
|
|
|
|