Advertisement
Advertisement
Advertisement
Advertisement
Arrhythmogenic right ventricular cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types (ARVC) is an inherited disorder of the heart muscle that affects the right ventricle (RV); it can cause rhythm disturbances and sudden cardiac death Sudden cardiac death Cardiac arrest is the sudden, complete cessation of cardiac output with hemodynamic collapse. Patients present as pulseless, unresponsive, and apneic. Rhythms associated with cardiac arrest are ventricular fibrillation/tachycardia, asystole, or pulseless electrical activity. Cardiac Arrest ( SCD SCD Sickle cell disease (SCD) is a group of genetic disorders in which an abnormal Hb molecule (HbS) transforms RBCs into sickle-shaped cells, resulting in chronic anemia, vasoocclusive episodes, pain, and organ damage. Sickle Cell Disease). The disorder results from mutations in the genes Genes A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. DNA Types and Structure that encode desmosomal proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis involved in cell-to-cell adhesion Adhesion The process whereby platelets adhere to something other than platelets, e.g., collagen; basement membrane; microfibrils; or other 'foreign' surfaces. Coagulation Studies. Symptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship develop palpitations Palpitations Ebstein’s Anomaly, arrhythmias leading to syncope Syncope Syncope is a short-term loss of consciousness and loss of postural stability followed by spontaneous return of consciousness to the previous neurologic baseline without the need for resuscitation. The condition is caused by transient interruption of cerebral blood flow that may be benign or related to a underlying life-threatening condition. Syncope, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, or chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. Diagnosis is based on clinical presentation, ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG), echocardiographic, and imaging findings. Management aims to prevent SCD SCD Sickle cell disease (SCD) is a group of genetic disorders in which an abnormal Hb molecule (HbS) transforms RBCs into sickle-shaped cells, resulting in chronic anemia, vasoocclusive episodes, pain, and organ damage. Sickle Cell Disease and symptom-causing arrhythmias. Treatment includes implantable cardioverter-defibrillator (ICD) placement, radiofrequency ablation Radiofrequency ablation Removal of tissue using heat generated from electrodes delivering an alternating electrical current in the frequency of radio waves. Hepatocellular Carcinoma (HCC) and Liver Metastases to correct arrhythmias, and antiarrhythmic medications. Prevention of disease progression with lifestyle changes is important, and cardiac transplantation may be necessary after 15 years.
Last updated: May 16, 2024
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Arrhythmogenic right ventricular cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types (ARVC) is a genetic disease of the heart muscle characterized by the fibrofatty replacement of the right ventricular myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy.
The clinical presentation of arrhythmogenic right ventricular cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types is variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables and may remain silent for decades, making it difficult to recognize.
The details of the 2017 Report of the American College of Cardiology/ American Heart Association American Heart Association A voluntary organization concerned with the prevention and treatment of heart and vascular diseases. Heart Failure Task Force and the Heart Rhythm Society (ACC/AHA/ HRS HRS Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of hrs is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome) are beyond the scope here. The report defines global or regional dysfunction and structural alterations with detailed echocardiographic measurements of the RV outflow tract.
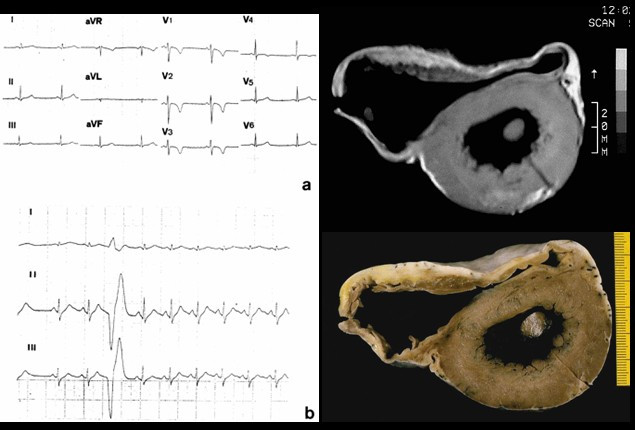
Left: 12-lead ECG shows (a) inverted T waves in V1–V4 and (b) ventricular ectopic beats.
Right: cross-section of the heart with the right ventricular dilatation, anterior and posterior aneurysms
The main goals in the management of arrhythmogenic right ventricular cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types are to prevent life-threatening arrhythmias and to slow the progression of the disease.