Bundle branch and fascicular blocks occur when the normal electrical activity in the His-Purkinje system is interrupted. These blocks can be due to many etiologies that may affect the structure of the heart or the conduction system directly. The blocks are classified into right bundle branch block, left bundle branch block, left anterior fascicular block, and left posterior fascicular block depending on the location of the disruption. Most individuals are asymptomatic. ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) will provide the diagnosis. Some common ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG) findings include a prolonged QRS interval, R-wave changes, axis deviation, and (in some cases) S-wave changes. No specific treatment is indicated.
Last updated: May 16, 2024
Bundle branch and fascicular blocks are classified on the basis of where the disruption occurs within the His-Purkinje system.
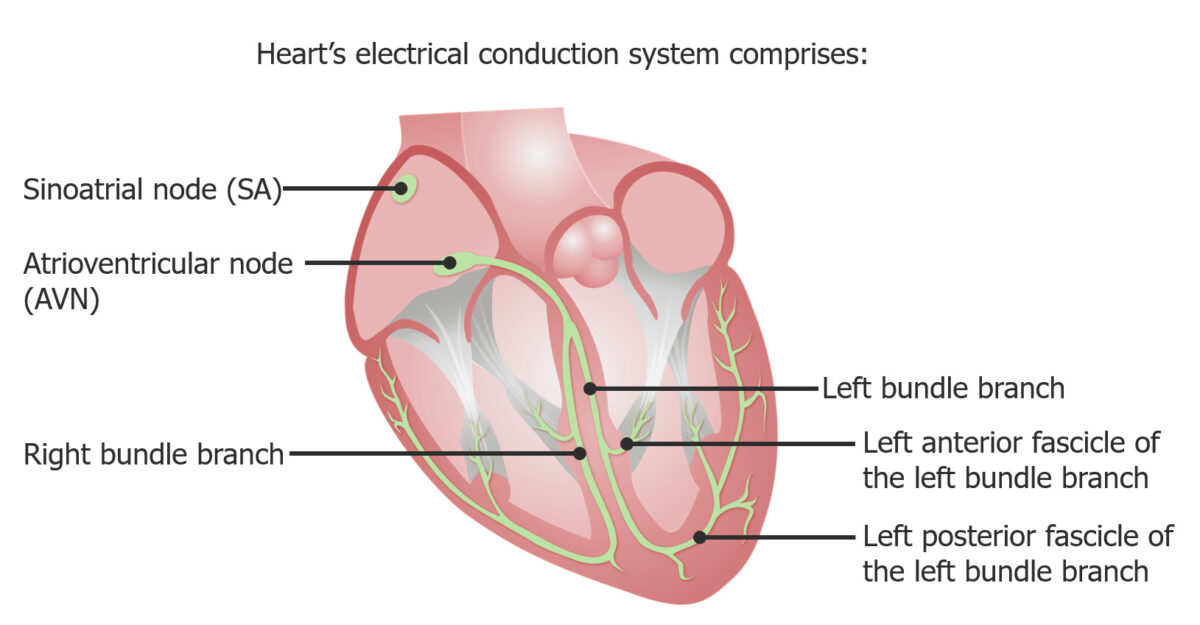
Bundle branch and fascicular blocks arise because of obstruction of electrical current through the His-Purkinje system and are named on the basis of the location of that disruption.
Image by Lecturio.These fascicular blocks can occur because of many of the same causes of RBBB or LBBB, most notably:
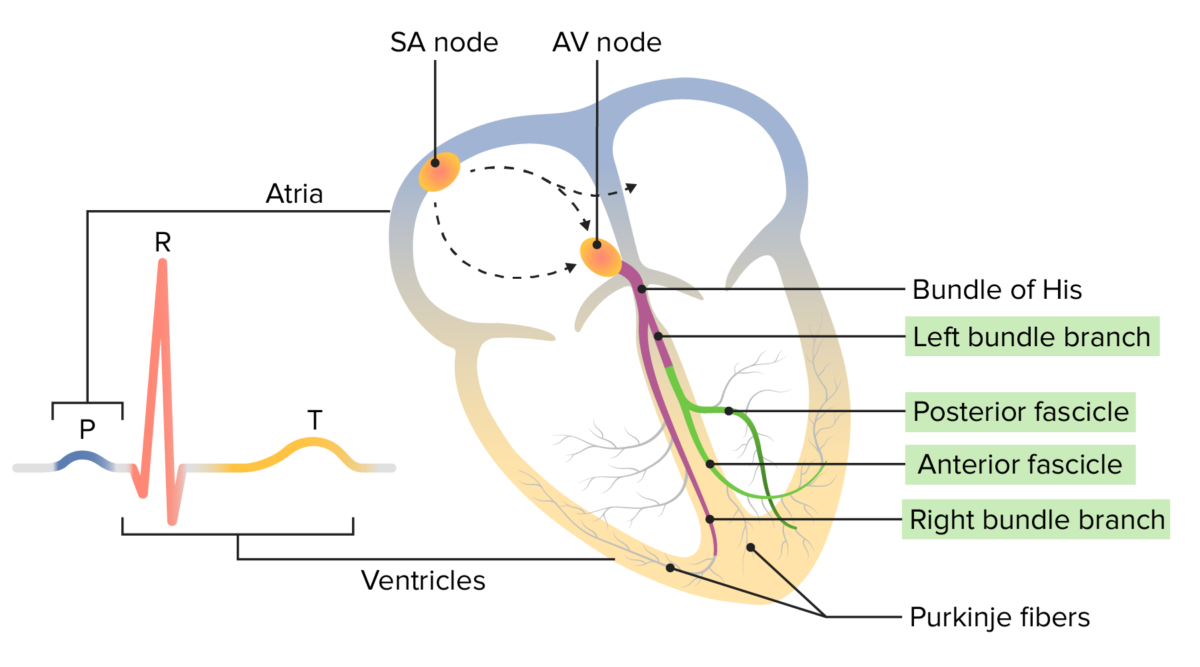
Normal electrophysiology of the heart:
The conduction impulse starts at the sinoatrial (SA) node and travels through the atrium to the atrioventricular (AV) node. From there, it moves through the bundle of His down through both bundle branches (and fascicles) to the Purkinje fibers. The movement of this electrical impulse can be recorded on an ECG.
P wave (blue): depolarization of atrial myocardium
QRS complex (orange): depolarization of ventricular myocardium
T wave (yellow): repolarization of ventricular myocardium
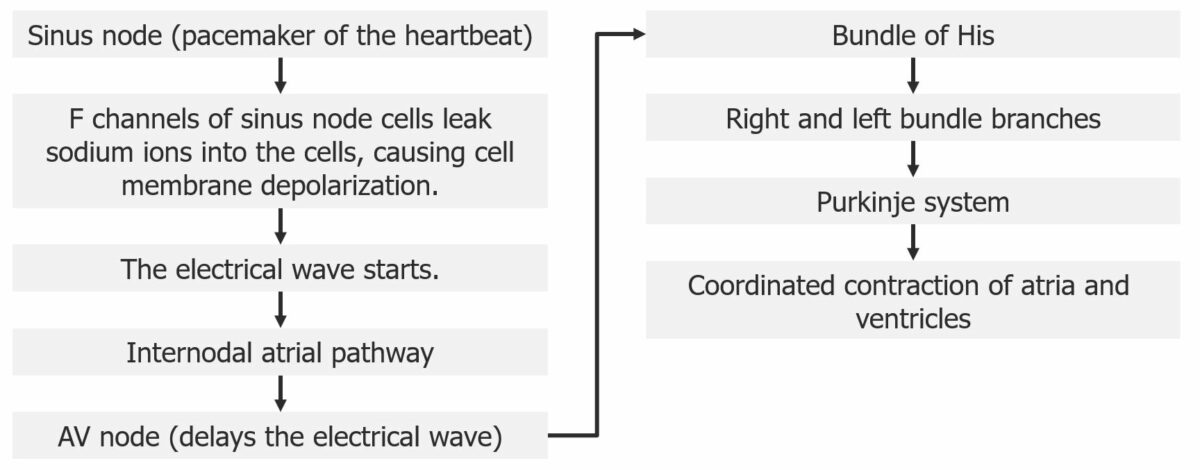
Diagram outlining the electrical pathway through the heart
Image by Lecturio.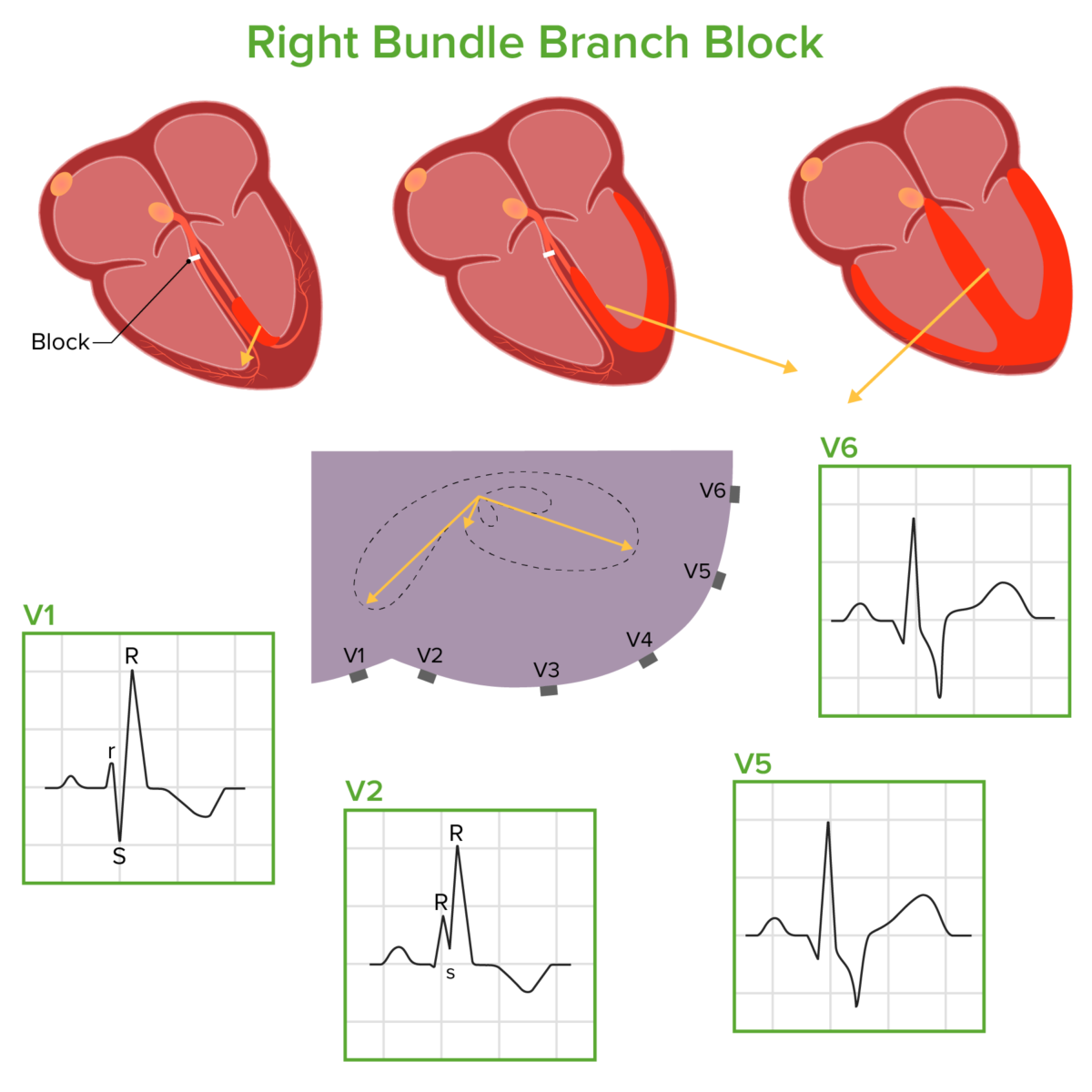
Diagram demonstrating how electrical conduction moves through the ventricles in a right bundle branch block:
The electrical impulse runs through the left bundle branch, through the septum and left ventricle, and then through the right ventricle. These phases result in the electrical conduction vectors shown above (drawn in relation to a cross section of the thorax with the precordial leads attached), which correlate with the corresponding ECG waveforms.
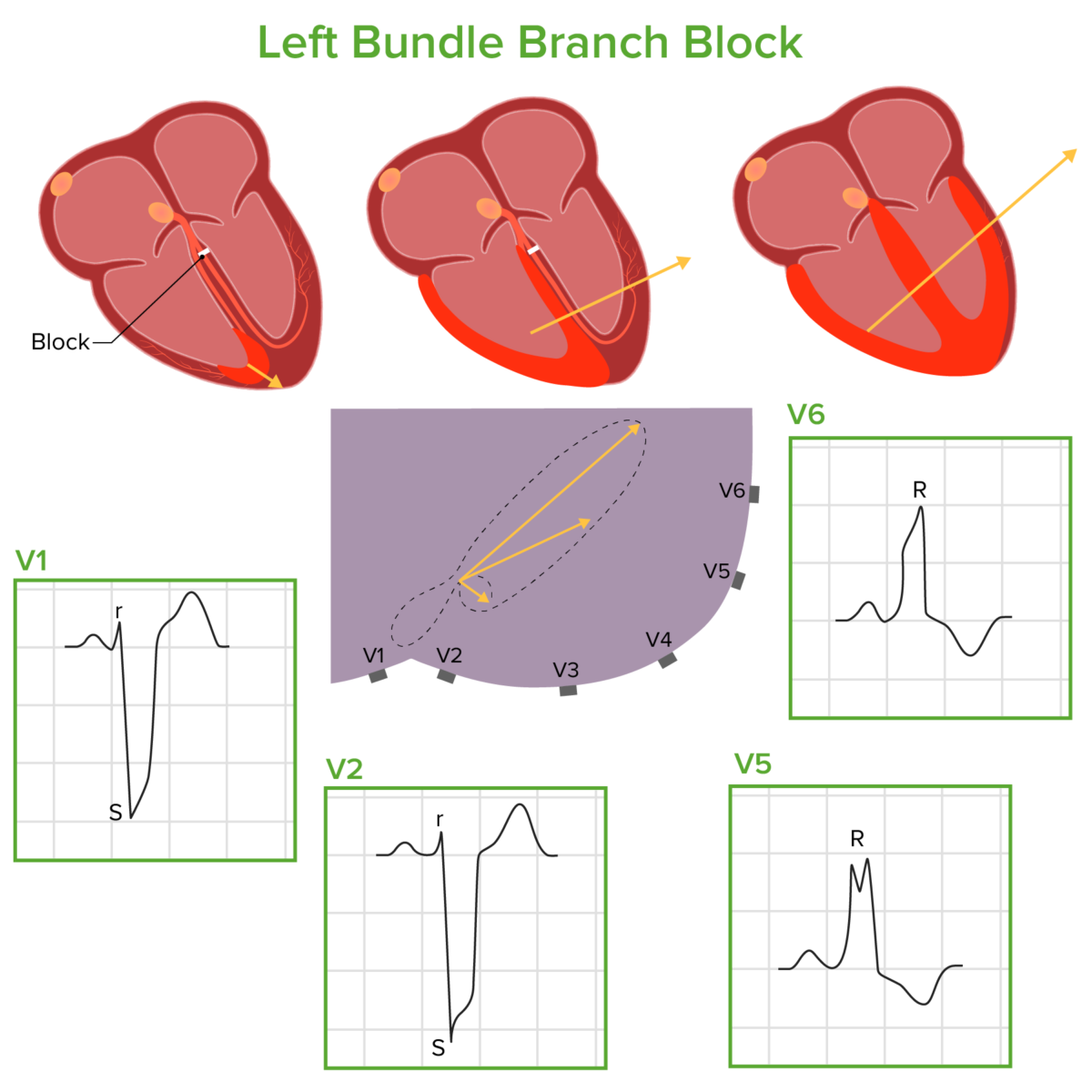
Diagram demonstrating how electrical conduction moves through the ventricles in a left bundle branch block:
The electrical impulse runs through the right bundle branch, through the septum and right ventricle, and then through the left ventricle. These phases result in the electrical conduction vectors shown above (drawn in relation to a cross section of the thorax with the precordial leads attached), which correlate with the corresponding ECG waveforms.
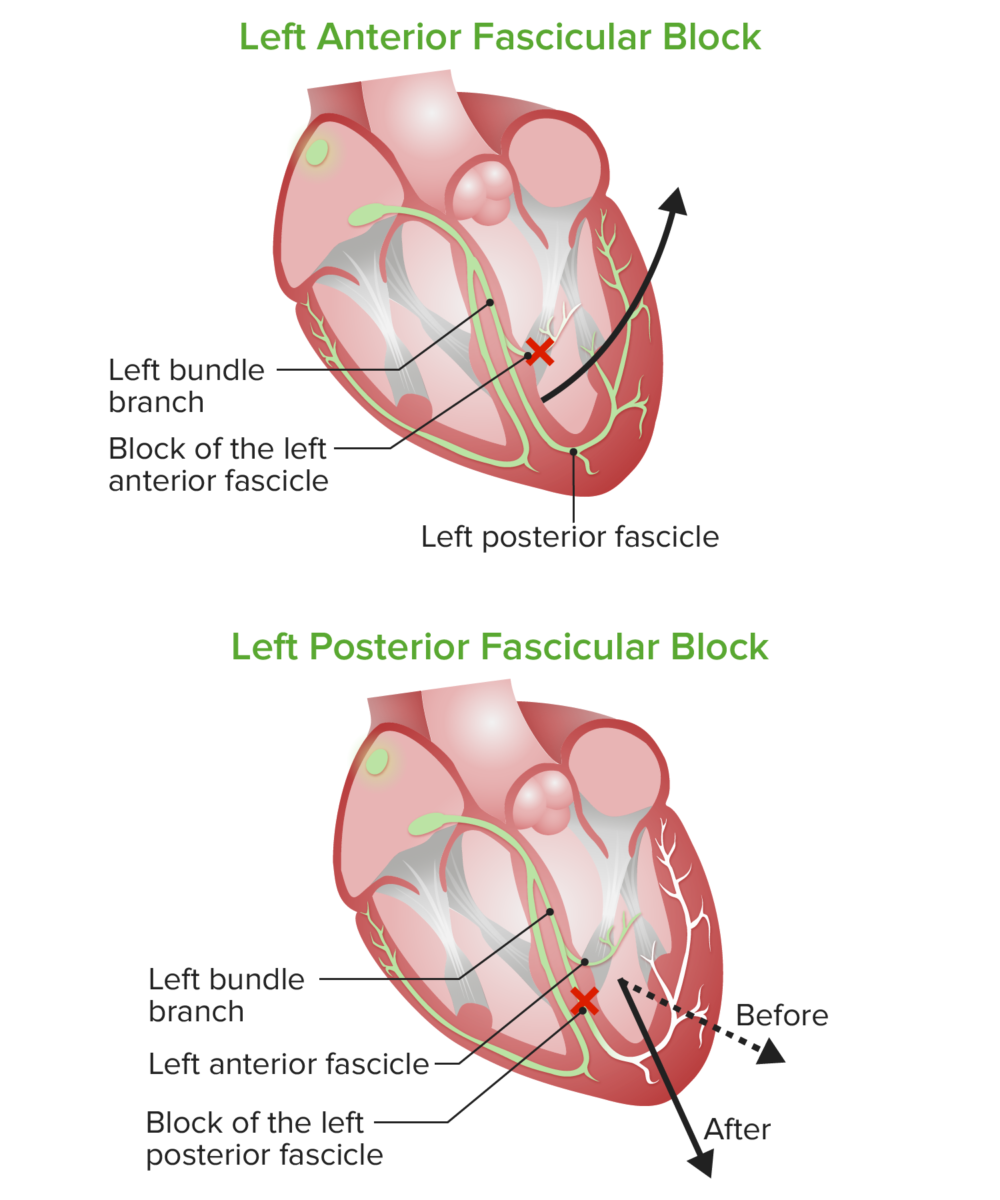
Diagram of left anterior and posterior fascicular blocks:
In left anterior fascicular block or hemiblock (LAFB), the resultant electrical vector results in significant left axis deviation. In left posterior fascicular block or hemiblock (LPFB), the electrical vector is deviated a bit rightward but is not significantly displaced from the normal QRS axis range.
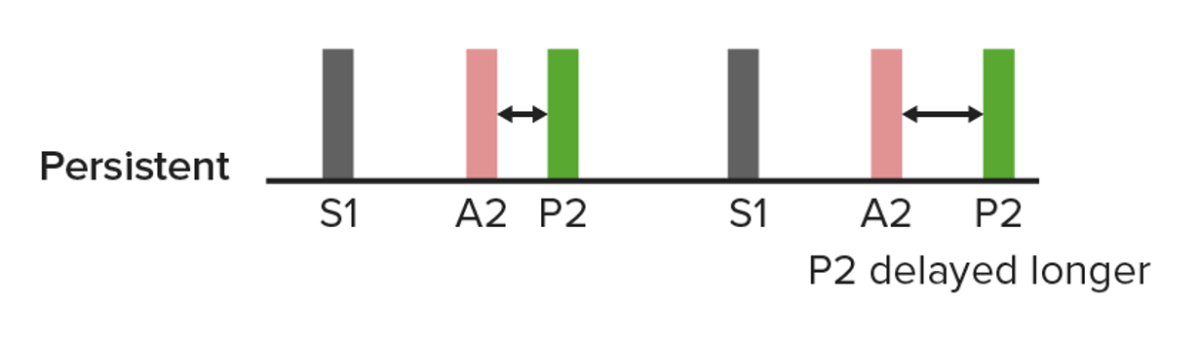
A diagram of a persistent split S2, in which closure of the pulmonic valve is delayed further by inspiration (right). This can occur in a right bundle branch block.
Image by Lecturio.Audio:
This audio clip is an example of a split S2 S2 Heart Sounds in the setting of an RBBB. The 2 sounds occurring during S2 S2 Heart Sounds result from delayed closure Delayed Closure Gastroschisis of the pulmonic valve in relation to the aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy.
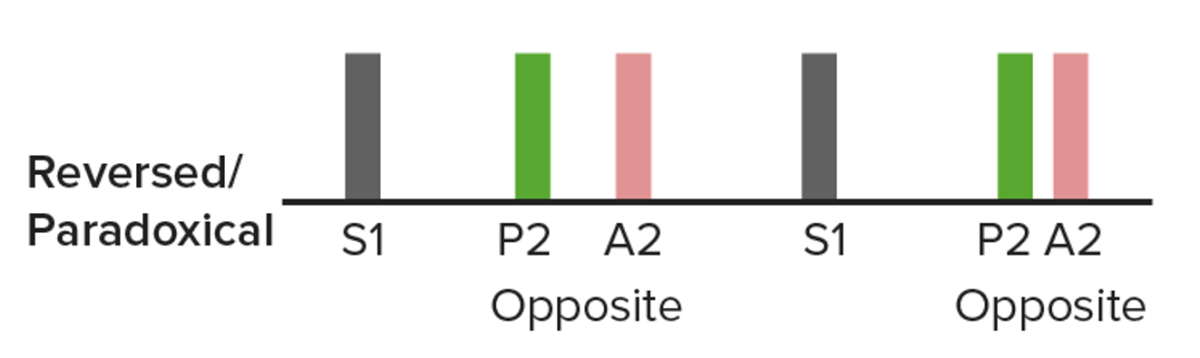
A diagram of a paradoxical split in closure of the aortic valve which is delayed:
The name “paradoxical” is due to the fact that the split narrows with inspiration (right). This can be heard in some individuals with a left bundle branch block.
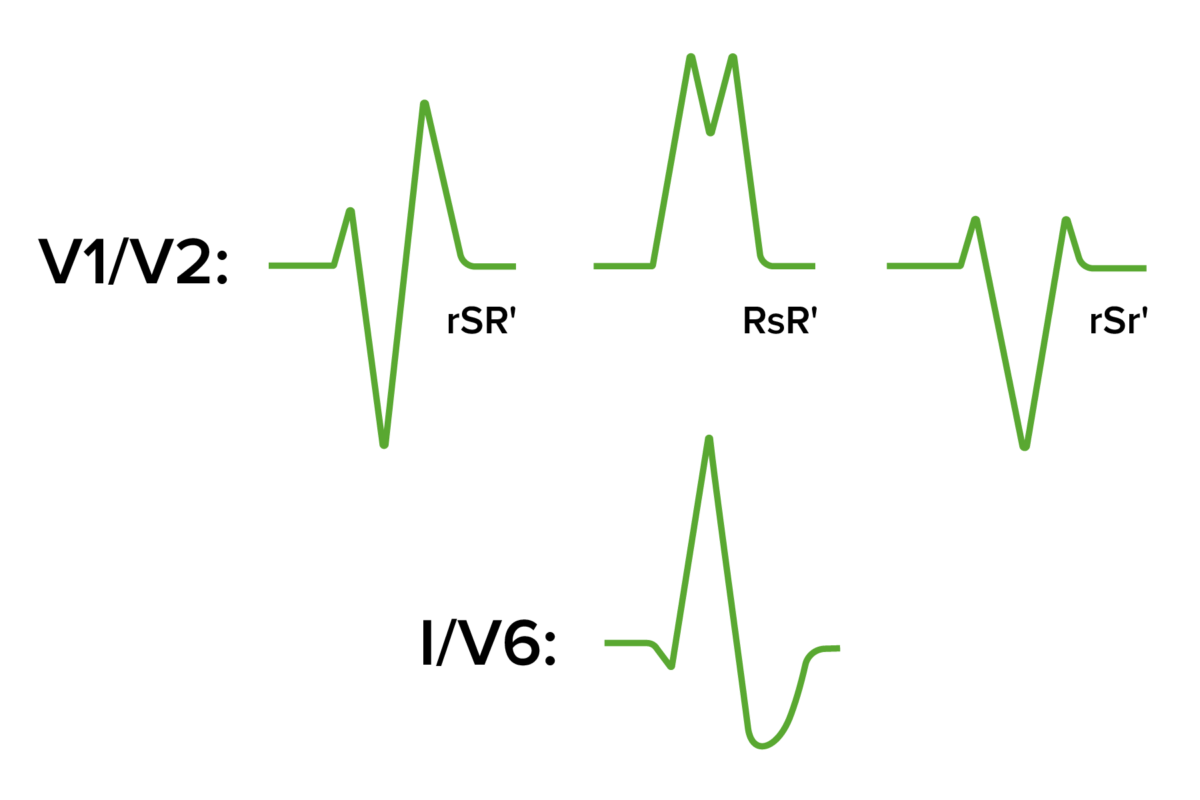
QRS morphology seen in right bundle branch block:
The RsR’ (and variations of this) give the appearance of “rabbit ears.” The S wave in leads I and V6 will appear broad, deep, and slurred.
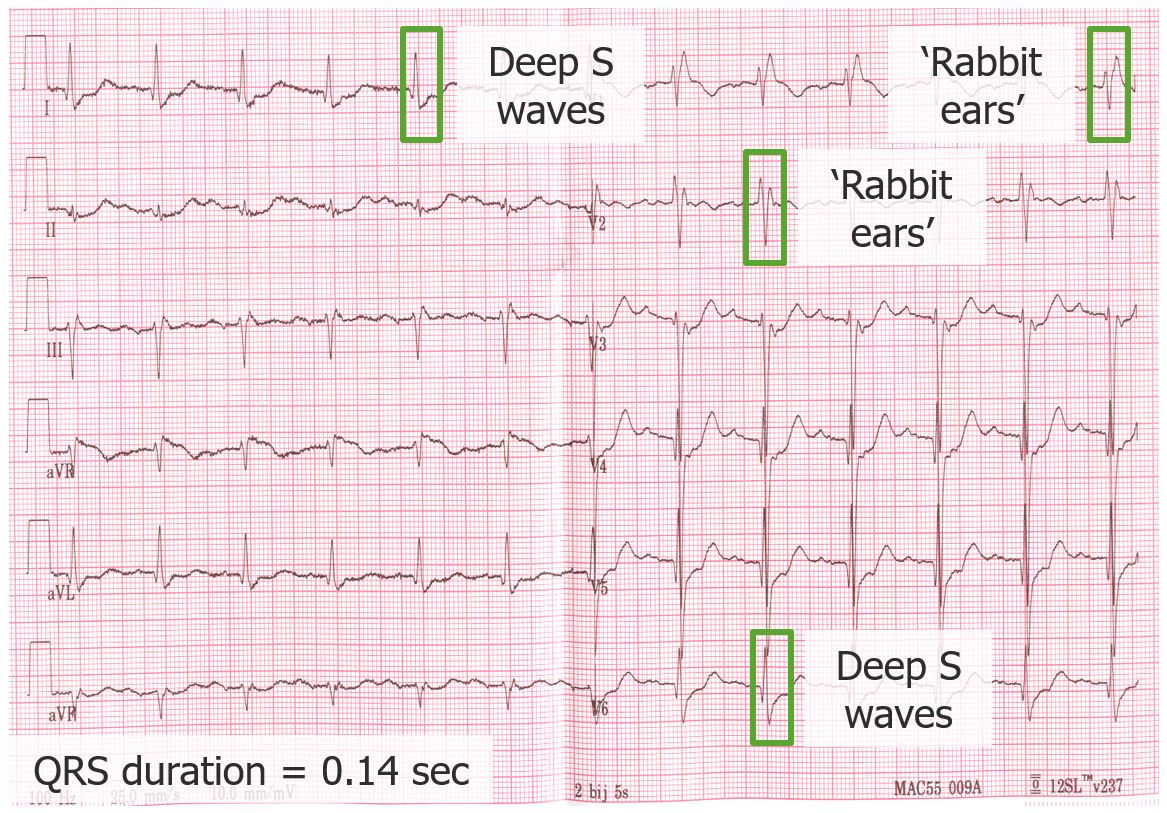
ECG demonstrating a right bundle branch block:
The QRS duration is prolonged, at 140 msec. Note the rSR’ and RSr’ in leads V1 and 2, along with the deep and broad S waves in I and V6.
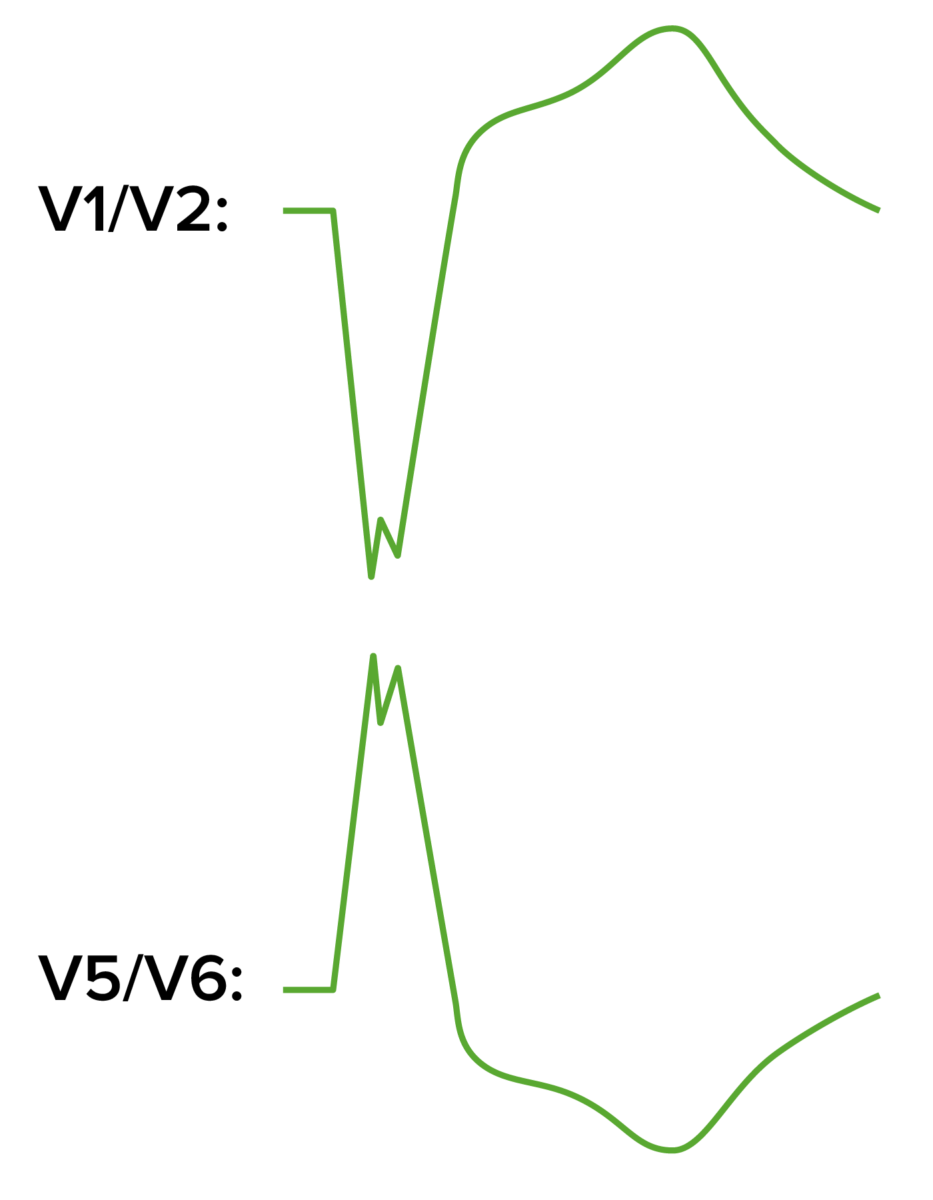
ECG patterns in left bundle branch block:
A large S wave will be seen in V1, while a large, notched R wave occurs in V5 and V6. Note that the ST-segment and T-wave directions are discordant to the QRS.
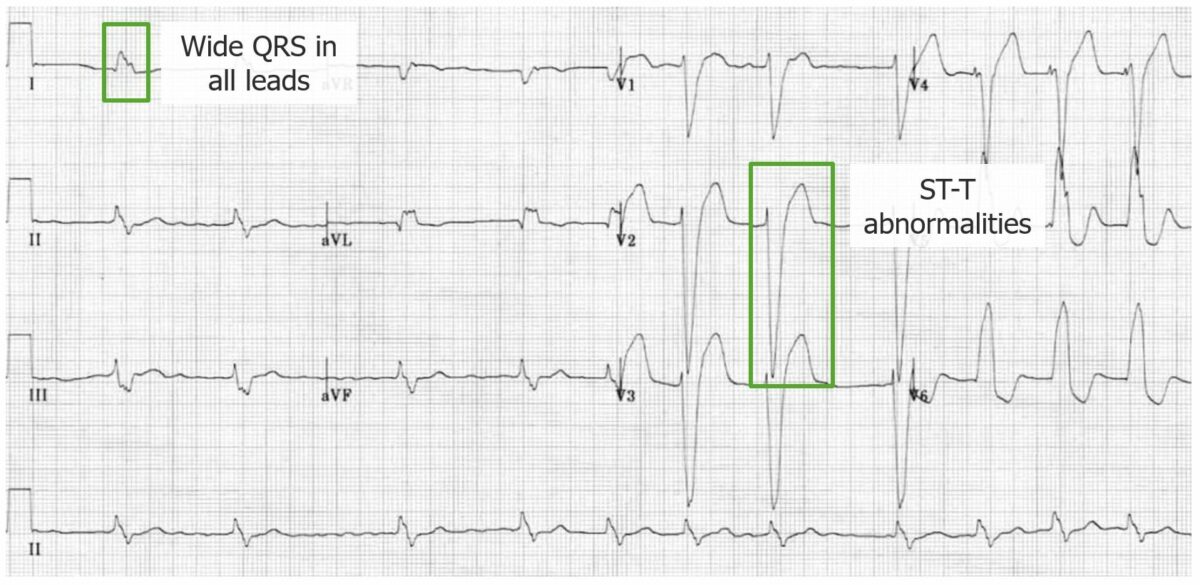
ECG demonstrating a left bundle branch block:
Note the widened QRS; the large, notched R waves in V5 and V6; and the large, broad S waves in V1 and 2. The ST segments and T waves are also generally discordant to the QRS complex.
A bundle branch block may be considered incomplete if the usual RBBB or LBBB pattern is seen but the QRS duration is 110–119 msec.
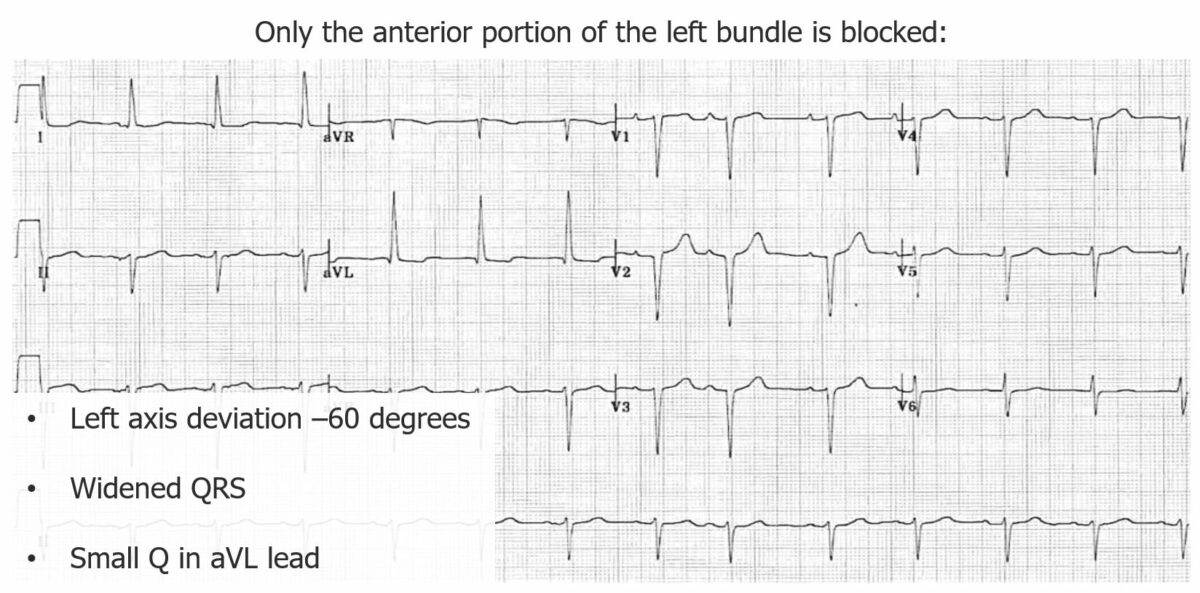
ECG demonstrating left anterior fascicular block:
Here, the axis is deviated to –60 degrees and a small Q wave is noted in aVL. The QRS is slightly prolonged, but still < 120 msec.
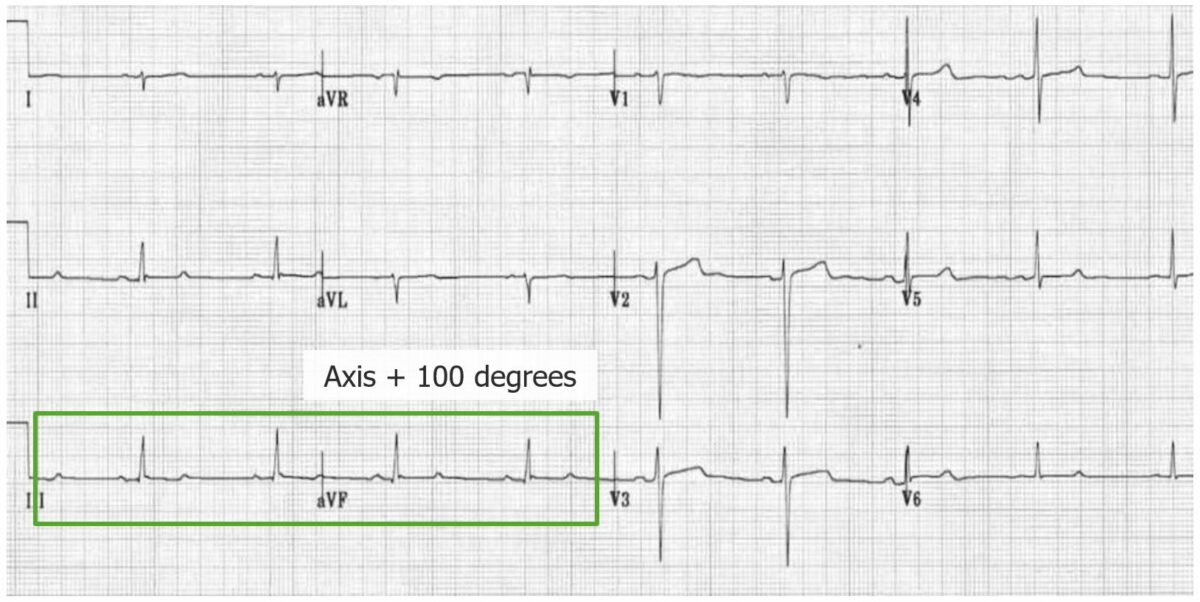
ECG demonstrating a left posterior fascicular block:
There is right axis deviation (+ 100 degrees), small Q waves in II, III, and aVF, rS complexes in I and aVL. The QRS complex duration is also < 120 msec.