Gastroschisis is a congenital abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen defect characterized by the complete lack of closure of the abdominal musculature. A portion of intestine does not return to the abdominal cavity, thereby remaining in its early embryonic herniated state but with no coverings. Diagnosis is made by prenatal ultrasonography. Findings include a paraumbilical wall defect with uncovered herniated intestines. Fetal surveillance Surveillance Developmental Milestones and Normal Growth and bowel monitoring are done to measure fetal growth and amniotic fluid Amniotic fluid A clear, yellowish liquid that envelopes the fetus inside the sac of amnion. In the first trimester, it is likely a transudate of maternal or fetal plasma. In the second trimester, amniotic fluid derives primarily from fetal lung and kidney. Cells or substances in this fluid can be removed for prenatal diagnostic tests (amniocentesis). Placenta, Umbilical Cord, and Amniotic Cavity volume, as well as observe any bowel changes. The mode and timing of delivery depend on these factors. Neonatal care includes protection of the exposed bowel, fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome, and airway Airway ABCDE Assessment maintenance. Primary closure can be performed within hours of birth. The presence of a large gastroschisis or thickened and dilated bowel warrants delayed closure, with the use a bowel covering or “silo,” and serial bowel reduction.
Last updated: Jan 7, 2025
Gastroschisis is a full-thickness defect of the anterior abdominal wall Abdominal wall The outer margins of the abdomen, extending from the osteocartilaginous thoracic cage to the pelvis. Though its major part is muscular, the abdominal wall consists of at least seven layers: the skin, subcutaneous fat, deep fascia; abdominal muscles, transversalis fascia, extraperitoneal fat, and the parietal peritoneum. Surgical Anatomy of the Abdomen through which the intestine and/or other abdominal viscera freely protrude.
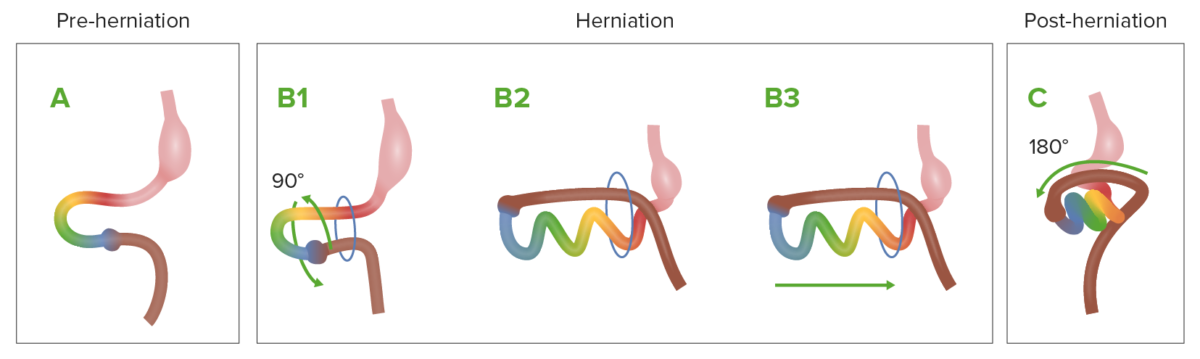
Diagram showing the normal process of intestinal rotation and herniation during embryologic development
A: the midgut (multi-colored loop) before herniation.
B1-B3: as it grows rapidly, the midgut herniates through the umbilical ring, and starts rotation.
C: The midgut returns to the abdominal cavity.
Embryologic hypotheses leading to herniation Herniation Omphalocele of the bowel:

Illustration of an abdominal wall defect with herniated bowel not covered by a sac or a membrane (gastroschisis)
Image by Lecturio.
Gastroschisis in a newborn. Note the eviscerated bowel to the right of the umbilical insertion.
Image: “Gastroschis with concomitant jejuno-ileala tresia type III b” by Clinic of Pediatric Surgery, University Clinical Center Sarajevo, Sarajevo, Bosnia and Herzegovina. License: CC BY 3.0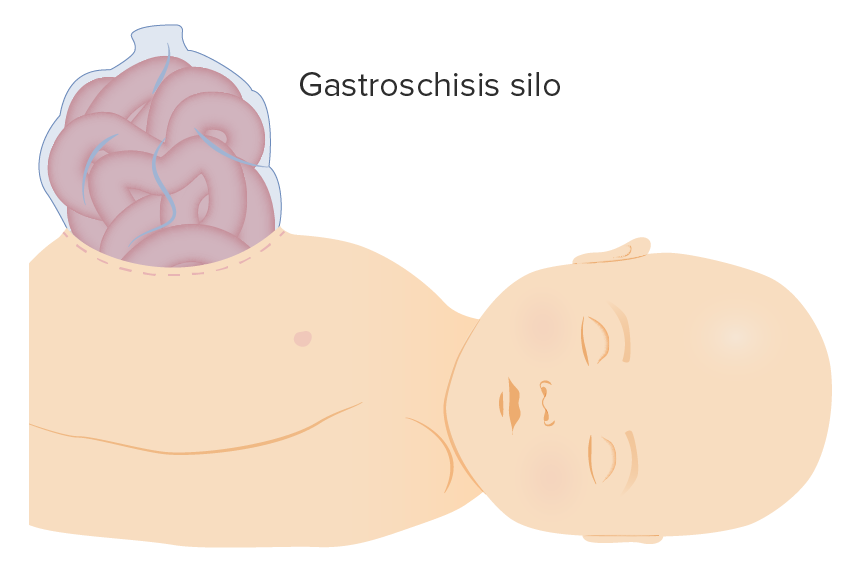
Gastroschisis silo
Image by Lecturio.