Neural tube Neural tube A tube of ectodermal tissue in an embryo that will give rise to the central nervous system, including the spinal cord and the brain. Lumen within the neural tube is called neural canal which gives rise to the central canal of the spinal cord and the ventricles of the brain. Gastrulation and Neurulation defects (NTDs) are the 2nd-most common type of congenital birth defects. Neural tube Neural tube A tube of ectodermal tissue in an embryo that will give rise to the central nervous system, including the spinal cord and the brain. Lumen within the neural tube is called neural canal which gives rise to the central canal of the spinal cord and the ventricles of the brain. Gastrulation and Neurulation defects can range from asymptomatic (closed NTD) to very severe malformations of the spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy or brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification (open NTD). Neural tube Neural tube A tube of ectodermal tissue in an embryo that will give rise to the central nervous system, including the spinal cord and the brain. Lumen within the neural tube is called neural canal which gives rise to the central canal of the spinal cord and the ventricles of the brain. Gastrulation and Neurulation defects are caused by the failure of the neural tube Neural tube A tube of ectodermal tissue in an embryo that will give rise to the central nervous system, including the spinal cord and the brain. Lumen within the neural tube is called neural canal which gives rise to the central canal of the spinal cord and the ventricles of the brain. Gastrulation and Neurulation to close properly during the 3rd and 4th week of embryological development. The most common type of open NTD is meningomyelocele, which involves both the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy and neural tissue. The etiologies of NTD are multifactorial, ranging from maternal nutrition to genetic determinants. Prenatal diagnosis by ultrasound and maternal α-fetoprotein level is common. Management of open NTDs is mainly surgical.
Last updated: Feb 7, 2025
A neural tube Neural tube A tube of ectodermal tissue in an embryo that will give rise to the central nervous system, including the spinal cord and the brain. Lumen within the neural tube is called neural canal which gives rise to the central canal of the spinal cord and the ventricles of the brain. Gastrulation and Neurulation defect (NTD; spinal dysraphism Dysraphism Teratogenic Birth Defects) is a congenital defect in the covering of the central nervous system Central nervous system The main information-processing organs of the nervous system, consisting of the brain, spinal cord, and meninges. Nervous System: Anatomy, Structure, and Classification, resulting from a failure of the neural tube Neural tube A tube of ectodermal tissue in an embryo that will give rise to the central nervous system, including the spinal cord and the brain. Lumen within the neural tube is called neural canal which gives rise to the central canal of the spinal cord and the ventricles of the brain. Gastrulation and Neurulation to close spontaneously during the 3rd or 4th week of embryonic development.
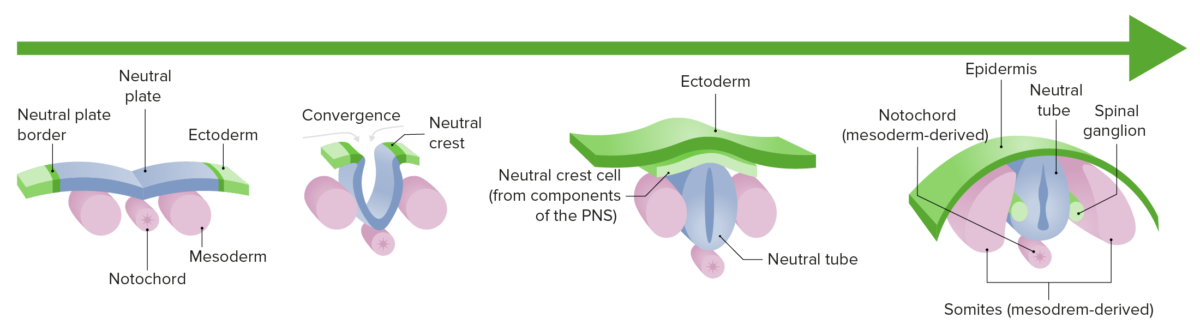
Neurulation: the differentiation and growth of the neural plate into the neural tube during the first trimester of gestation.
PNS: Peripheral nervous system
Most NTDs are discovered during prenatal screening Screening Preoperative Care. Open NTDs are evident at birth, but closed NTDs may have more subtle presentations.
| Name | Description | Clinical features |
|---|---|---|
| Myelomeningocele | Spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy and meningeal herniation Herniation Omphalocele | The higher the lesion in the
spine
Spine
The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum.
Vertebral Column: Anatomy, the more severe the symptoms:
|
| Meningocele | Meningeal herniation Herniation Omphalocele without spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy involvement |
|
| Encephalocele | Meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy ± brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification tissue protruding from cranial defect |
|
| Anencephaly | Major component of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy is absent. |
|
| Spina bifida occulta | Midline vertebral body Vertebral body Main portion of the vertebra which bears majority of the weight. Vertebral Column: Anatomy fusion defect without protruding dura or neural tissue |
|
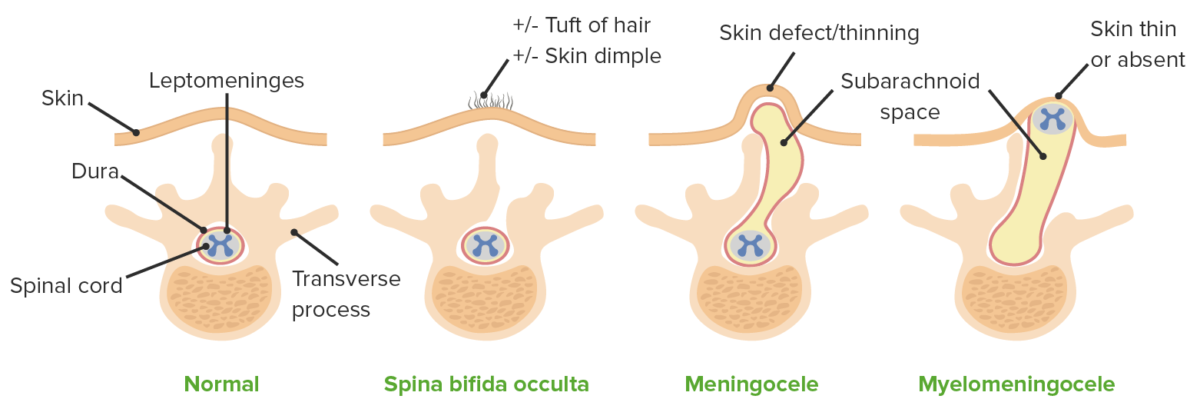
Types of NTD and their respective defect
Image by Lecturio.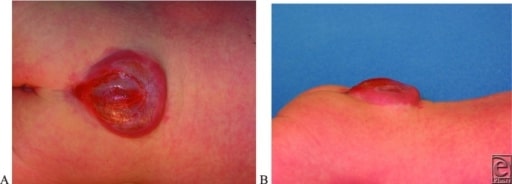
A and B: Posterior and lateral photographs demonstrating a lumbosacral myelomeningocele
Image: “Lumbosacral Myelomeningocele” by US National Library of Medicine. License: CC BY 2.0
Tuft of hair over the lower back in a patient with spina bifida
Image: “Hypertrichiosis” by Department of Pediatric Surgery, Maulana Azad Medical College, New Delhi. License: CC BY 3.0