A volvulus is the twisting or axial Axial Computed Tomography (CT) rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays of a portion of the bowel around its mesentery Mesentery A layer of the peritoneum which attaches the abdominal viscera to the abdominal wall and conveys their blood vessels and nerves. Peritoneum: Anatomy. The most common site of volvulus in adults is the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy; most frequently the sigmoid volvulus. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with symptoms of bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis such as abdominal pain Abdominal Pain Acute Abdomen, distension, vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, and constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation/ obstipation Obstipation Large Bowel Obstruction. In severe cases, signs of bowel ischemia Bowel ischemia Mesenteric ischemia is a rare, life-threatening condition caused by inadequate blood flow through the mesenteric vessels, which results in ischemia and necrosis of the intestinal wall. Mesenteric ischemia can be either acute or chronic. Mesenteric Ischemia and gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction ( tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, hematochezia Hematochezia Gastrointestinal Bleeding, and peritonitis Peritonitis Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Penetrating Abdominal Injury) may also be present. Clinical suspicion prompts imaging to confirm the diagnosis and surgery is the definitive treatment. For stable patients Stable Patients Blunt Chest Trauma with sigmoid volvulus, surgery may be preceded by endoscopic detorsion. However, immediate surgery is required for colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis or ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage.
Last updated: Jun 15, 2025
A volvulus is the twisting of a segment of bowel on its mesentery Mesentery A layer of the peritoneum which attaches the abdominal viscera to the abdominal wall and conveys their blood vessels and nerves. Peritoneum: Anatomy, which results in bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis.
Sigmoid volvulus:
Cecal volvulus:

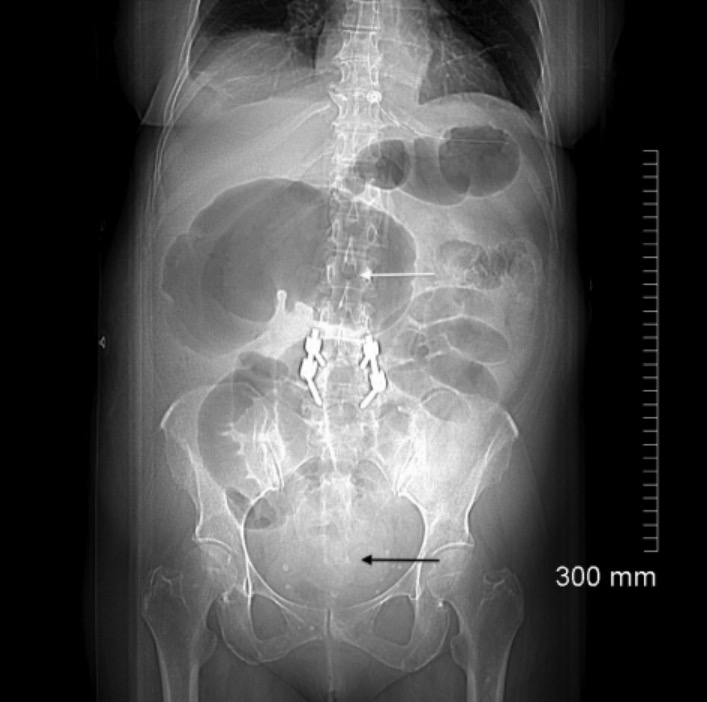
Abdominal radiography showing a sigmoid volvulus with its characteristic coffee bean appearance
Image: “Sigmoidvolvulus” by Mont4nha. License: CC0
Cecal volvulus:
Computed tomography (CT) shows a whirl sign (arrow) and distended cecum (arrowhead) in the upper left abdominal cavity and small bowel
Computed tomography (CT) scout image of cecal volvulus:
In the right upper quadrant, an image of a dilated cecum producing the classic kidney bean sign (white arrow). Centrally present within the abdomen, multiple dilated loops of small bowel and, in the distal colon, a paucity of gas (black arrow) are suggestive of a complete intestinal obstruction.
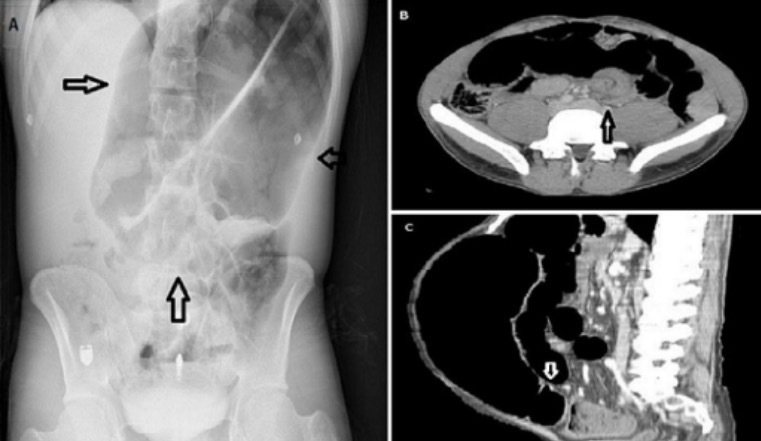
Coffee bean sign (A), whirl sign (B) and bird’s beak sign (C) in the diagnosis of sigmoid volvulus
Image: “Diagnosis of sigmoid volvulus” by Bezmialem Vakif University, Department of Emergency Medicine, Istanbul, Turkey. License: CC BY 2.0Sigmoidoscopy Sigmoidoscopy Endoscopic examination, therapy or surgery of the sigmoid flexure. Colorectal Cancer Screening with detorsion:
Surgery:

Sigmoid volvulus (intraoperative view)
Image: “Sigmoid volvulus during surgery” by General Surgery Department, Aga Khan University Hospital, Stadium Road, Karachi 74800, Pakistan. License: CC BY 2.0Overall mortality Mortality All deaths reported in a given population. Measures of Health Status:
Predictors of mortality Mortality All deaths reported in a given population. Measures of Health Status: