Chagas disease is an infection caused by the American trypanosome Trypanosoma cruzi. This parasitic protozoan is transmitted in the feces of reduviid bugs in South and Central America. Acute infection may present with inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation at the inoculation site Inoculation site Yellow Fever Virus (chagoma), fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, and lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy. Untreated, chronic infection can progress to severe complications, including megacolon Megacolon Megacolon is a severe, abnormal dilatation of the colon, and is classified as acute or chronic. There are many etiologies of megacolon, including neuropathic and dysmotility conditions, severe infections, ischemia, and inflammatory bowel disease. Megacolon, megaesophagus, and cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types. The diagnosis can be confirmed with identification Identification Defense Mechanisms of organisms on blood smear Blood smear Myeloperoxidase Deficiency, serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus, or PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR). Treatment with benznidazole or nifurtimox is effective only in the acute phase Acute phase Short Bowel Syndrome.
Last updated: Sep 19, 2022

Photomicrograph of a blood smear showing 5 parasitic, flagellated Trypanosoma cruzi trypomastigotes
Image: “Photomicrograph of a blood smear showing five parasitic, flagellated, Trypanosoma cruzi trypomastigotes” by CDC. License: Public Domain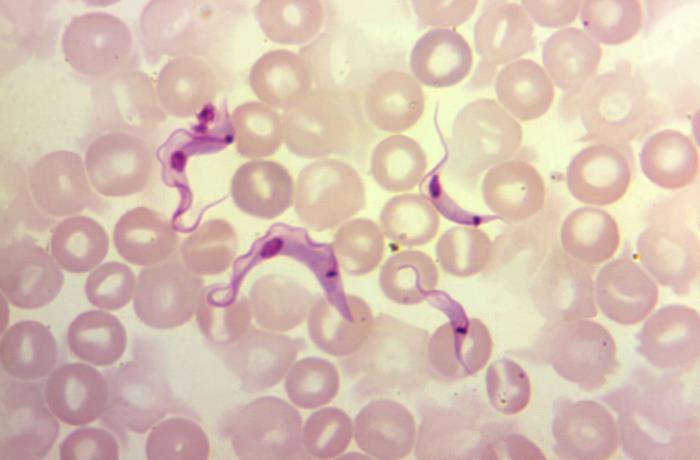
Photomicrograph of a blood sample specimen showing 4 flagellated Trypanosoma cruzi parasites, referred to as trypomastigotes
Image: “Under a magnification of 1200X, this photomicrograph of a blood sample specimen, revealed the presence of four flagellated, Trypanosoma cruzi parasites” by CDC. License: Public DomainAmerican trypanosomiasis is called Chagas disease.

A species of Triatoma, or kissing bug:
The kissing bug serves as a vector to transmit the protozoan pathogen Trypanosoma cruzi, which causes Chagas disease.
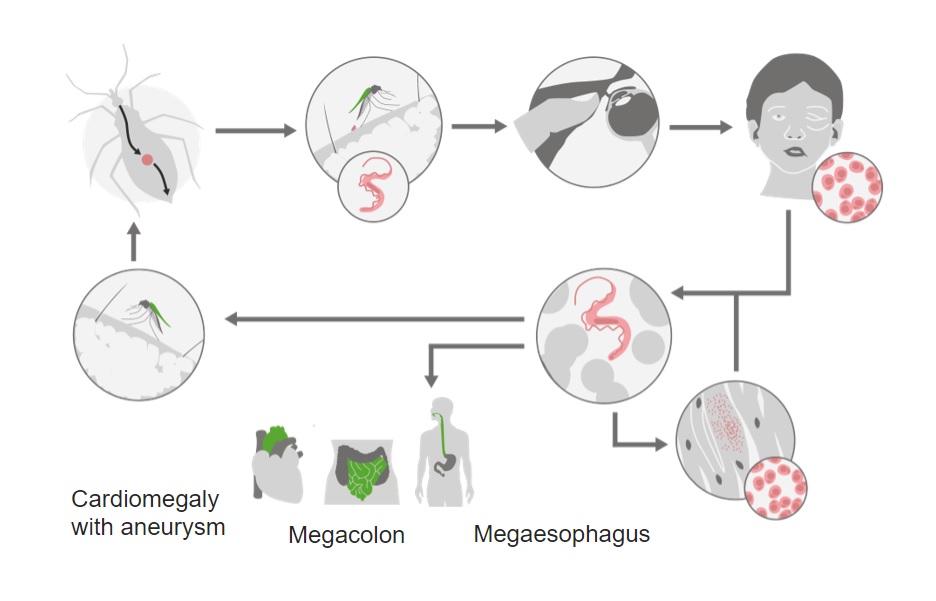
Life cycle of the American trypanosome Trypanosoma cruzi:
During a blood meal, the reduviid bug will defecate. Scratching the area allows entry of parasites through the bite wound or conjunctiva.
Once inside the body, replication and dissemination occurs. There is particular preference for myocardium and myenteric plexus.
With chronic infection, tissue damage can lead to cardiomyopathy, megacolon, and megaesophagus.
The incubation Incubation The amount time between exposure to an infectious agent and becoming symptomatic. Rabies Virus period is approximately 1–2 weeks, and the infection lasts 8–12 weeks.

Photograph of a patient with acute Chagas disease infection with swelling of the right eye (Romaña’s sign).
Image: “An acute Chagas disease infection with swelling of the right eye (Romaña’s sign)” by CDC. License: Public DomainA minority of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship develop chronic infection, which presents 10–20 years after the initial inoculation period.
Congenital Congenital Chorioretinitis disease occurs in a minority of infants born to infected mothers.
Confirmatory tests:
Supporting evaluation:
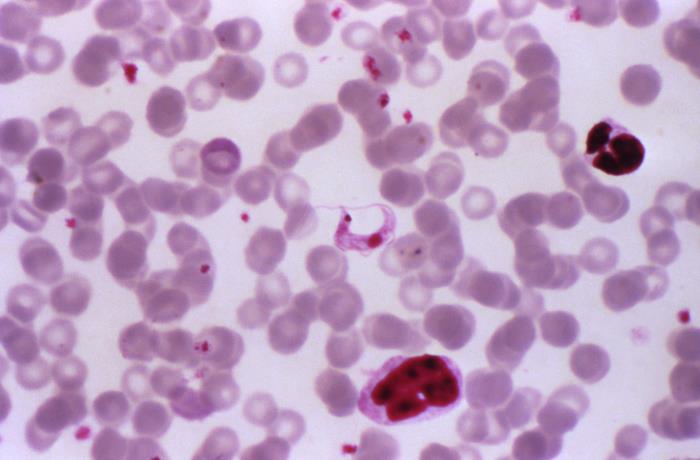
Photomicrograph of a Giemsa-stained blood smear specimen revealing the presence of a Trypanosoma cruzi trypomastigote
Image: “Under a magnification of 1000X, this photomicrograph of a Giemsa stained blood smear specimen revealed the presence of a parasitic Trypanosoma cruzi protozoan” by CDC. License: Public Domain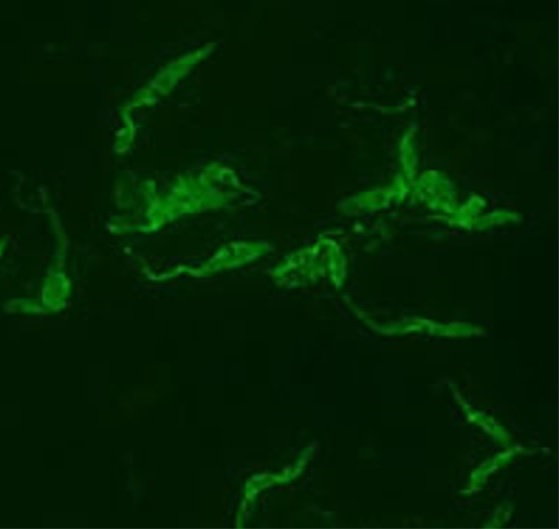
Indirect fluorescent antibody testing of a blood smear in a patient infected with Trypanosoma cruzi.
Image by Lecturio. License: CC BY-NC-SA 4.0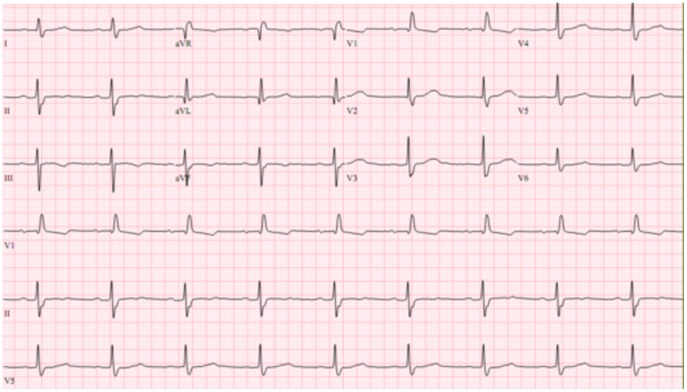
ECG showing a right bundle branch block with left anterior fascicular block in a patient with Chagas disease.
Image: “ECG showing a right bundle branch block with left anterior fascicular block” by de Alencar MC et al. License: CC BY 4.0
Chest X-ray image showing cardiac enlargement due to chronic Chagas cardiomyopathy
Image: “Heart radiology Chagas disease” by CDC. License: Public Domain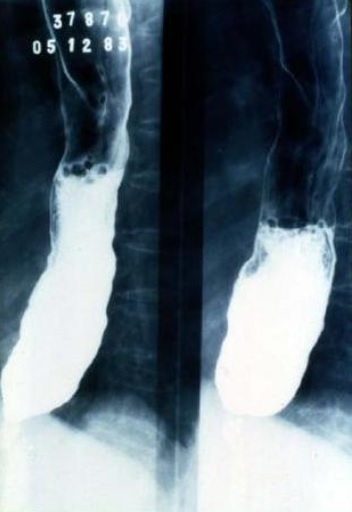
Barium esophagram demonstrating megaesophagus in a patient with Chagas disease
Image: “Chagas megaseophagus” by CDC. License: Public DomainAcute infection:
Chronic disease:
| Giardia Giardia A genus of flagellate intestinal eukaryotes parasitic in various vertebrates, including humans. Characteristics include the presence of four pairs of flagella arising from a complicated system of axonemes and cysts that are ellipsoidal to ovoidal in shape. Nitroimidazoles | Leishmania Leishmania Leishmania species are obligate intracellular parasites that are transmitted by an infected sandfly. The disease is endemic to Asia, the Middle East, Africa, the Mediterranean, and South and Central America. Clinical presentation varies, dependent on the pathogenicity of the species and the host’s immune response. Leishmania/Leishmaniasis | Trypanosoma | Trichomonas Trichomonas A genus of parasitic flagellate eukaryotes distinguished by the presence of four anterior flagella, an undulating membrane, and a trailing flagellum. Nitroimidazoles | |
|---|---|---|---|---|
| Characteristics |
|
|
|
|
| Forms |
|
|
|
|
| Transmission |
|
|
|
Sexually transmitted |
| Clinical | Giardiasis Giardiasis An infection of the small intestine caused by the flagellated protozoan giardia. It is spread via contaminated food and water and by direct person-to-person contact. Giardia/Giardiasis | Leishmaniasis Leishmaniasis Leishmania species are obligate intracellular parasites that are transmitted by an infected sandfly. The mildest form is cutaneous leishmaniasis (CL), characterized by painless skin ulcers. The mucocutaneous type involves more tissue destruction, causing deformities. Visceral leishmaniasis (VL), the most severe form, presents with hepatosplenomegaly, anemia, thrombocytopenia, and fever. Leishmania/Leishmaniasis |
|
Trichomoniasis |
| Diagnosis |
|
|
|
|
| Treatment |
|
Depends on the clinical syndrome:
|
Depends on the clinical disease:
|
|
| Prevention |
|
|
|
|
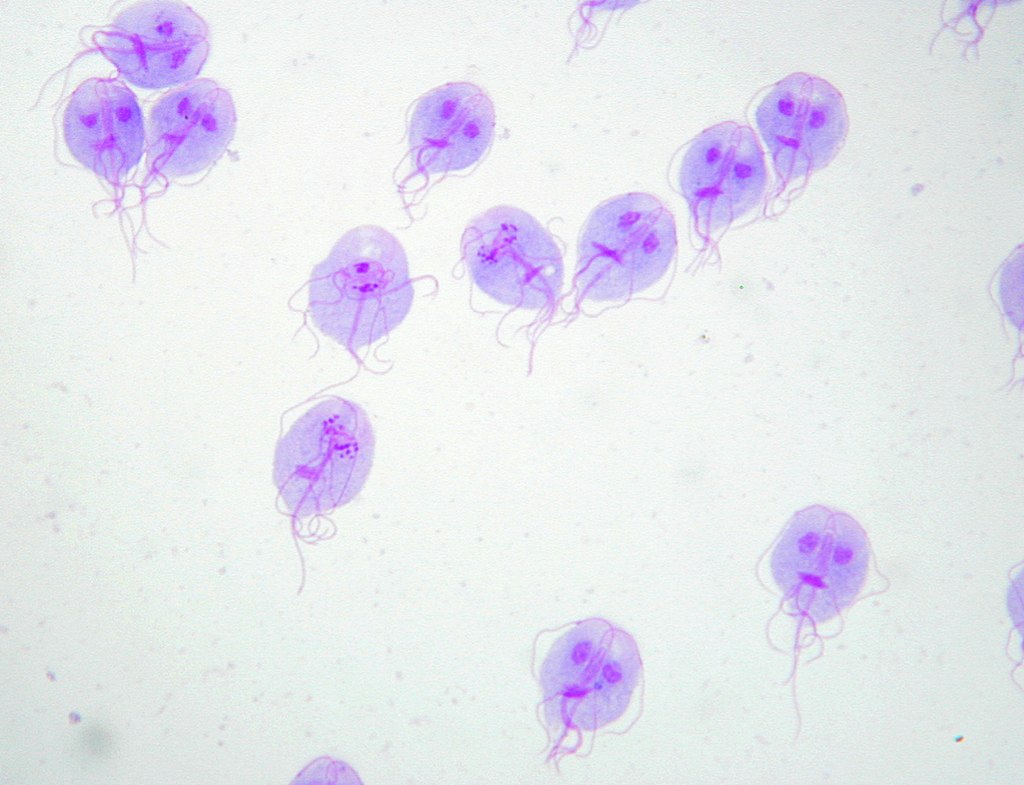
Giemsa stain of Giardia lamblia trophozoites
Image: “Trophozoites of Giardia lamblia” by Eva Nohýnková, Department of Tropical Medicine, 1st Faculty of Medicine, Charles University in Prague and Hospital Bulovka, Czech Republic. License: CC BY 4.0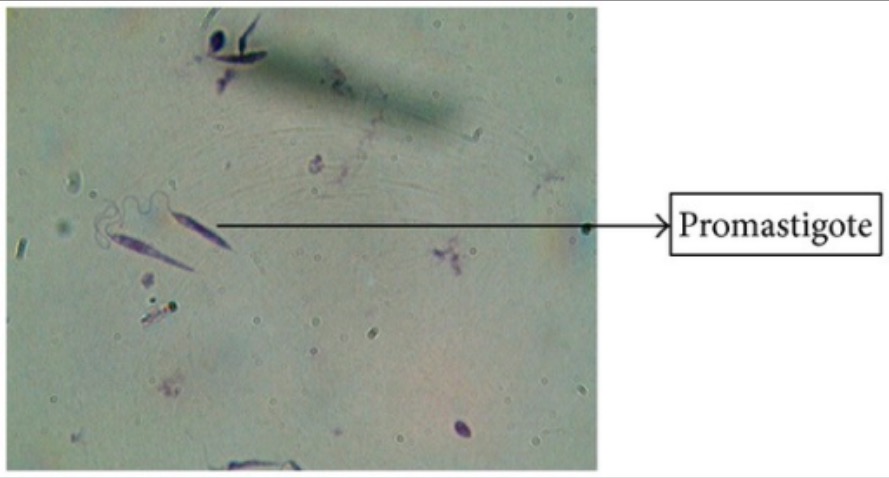
Giemsa stain of Leishmania promastigotes
Image: “Giemsa stain” by Arriyadh Community College, King Saud University, P.O. Box 28095, Riyadh 11437, Saudi Arabia. License: CC BY 3.0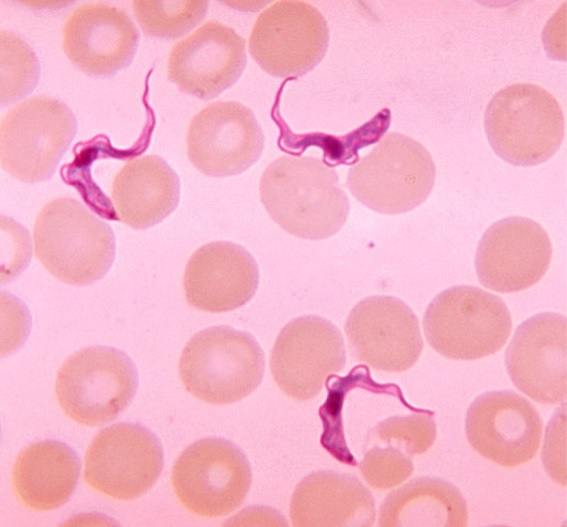
Blood smear demonstrating Trypanosoma trypomastigotes
Image by Lecturio. License: CC BY-NC-SA 4.0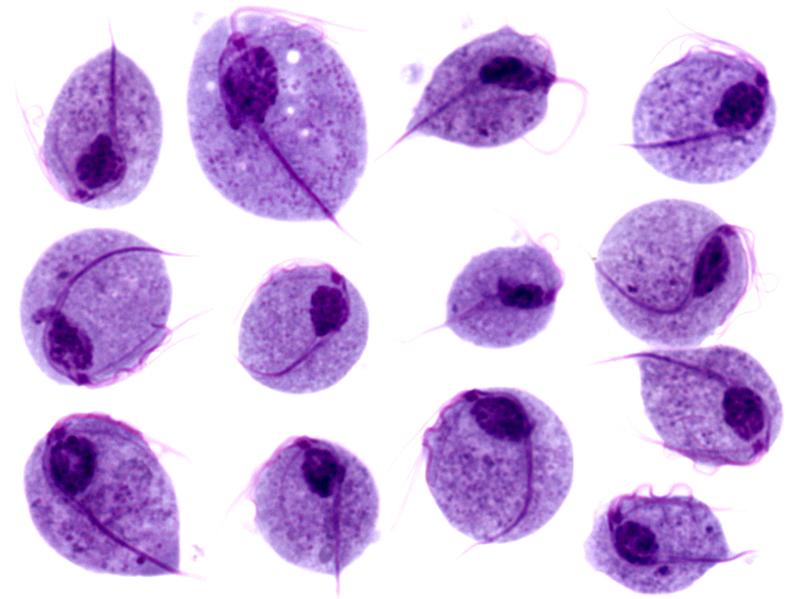
Microscopic images of Trichomonas vaginalis trophozoites
Image: “Trichomonas protozoa” by isis325. License: CC BY 2.0.