Borrelia are gram-negative microaerophilic Microaerophilic Helicobacter spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema. Owing to their small size, they are not easily seen on Gram stain Gram stain Klebsiella but can be visualized using dark-field microscopy Dark-field microscopy Treponema, Giemsa, or Wright stain. Spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema are motile and move in a characteristic spinning fashion due to axial Axial Computed Tomography (CT) filaments in the periplasmic space. The ability of Borrelia to express different repertoires of surface proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis allows for bacterial transmission and evasion of the host immune system Immune system The body's defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs. Borrelia utilizes Ixodes ticks Ticks Blood-sucking acarid parasites of the order ixodida comprising two families: the softbacked ticks (argasidae) and hardbacked ticks (ixodidae). Ticks are larger than their relatives, the mites. They penetrate the skin of their host by means of highly specialized, hooked mouth parts and feed on its blood. Ticks attack all groups of terrestrial vertebrates. In humans they are responsible for many tick-borne diseases, including the transmission of rocky mountain spotted fever; tularemia; babesiosis; african swine fever; and relapsing fever. Coxiella/Q Fever, Ornithodoros ticks Ticks Blood-sucking acarid parasites of the order ixodida comprising two families: the softbacked ticks (argasidae) and hardbacked ticks (ixodidae). Ticks are larger than their relatives, the mites. They penetrate the skin of their host by means of highly specialized, hooked mouth parts and feed on its blood. Ticks attack all groups of terrestrial vertebrates. In humans they are responsible for many tick-borne diseases, including the transmission of rocky mountain spotted fever; tularemia; babesiosis; african swine fever; and relapsing fever. Coxiella/Q Fever, and the human body louse Human Body Louse Epidemic Typhus as vectors, and the resulting diseases include Lyme disease Lyme disease Lyme disease is a tick-borne infection caused by the gram-negative spirochete Borrelia burgdorferi. Lyme disease is transmitted by the black-legged Ixodes tick (known as a deer tick), which is only found in specific geographic regions. Patient presentation can vary depending on the stage of the disease and may include a characteristic erythema migrans rash. Lyme Disease and relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever.
Last updated: Mar 27, 2025

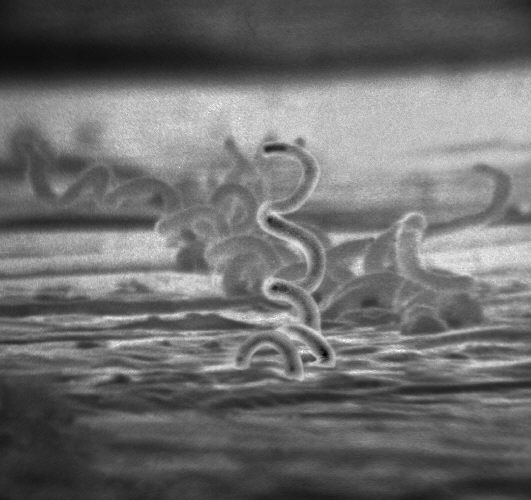
Dark-field microscopy of Borrelia burgdorferi
Image: “Borrelia burgdorferi (CDC-PHIL-6631) lores” by CDC. License: Public Domain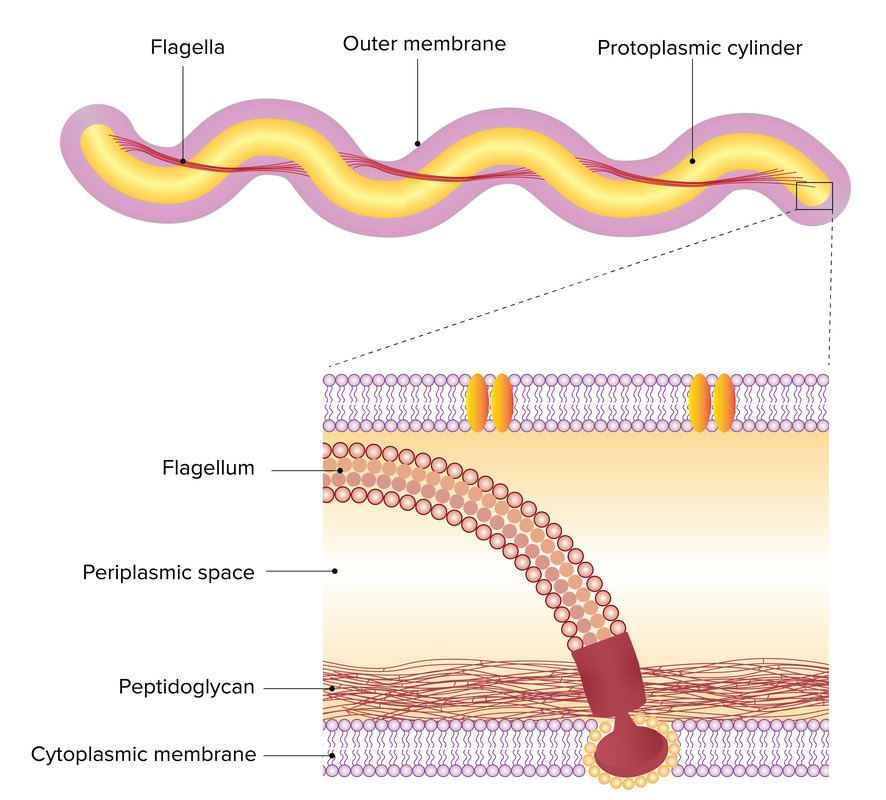
Axial filaments of Borrelia:
Axial filaments are made up of multiple periplasmic flagella (bottom picture). This allows the spirochete (top picture) to move in a spinning fashion.
The following diseases are caused by Borrelia:
| Disease | Lyme disease Lyme disease Lyme disease is a tick-borne infection caused by the gram-negative spirochete Borrelia burgdorferi. Lyme disease is transmitted by the black-legged Ixodes tick (known as a deer tick), which is only found in specific geographic regions. Patient presentation can vary depending on the stage of the disease and may include a characteristic erythema migrans rash. Lyme Disease | Relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever |
|---|---|---|
| Associated species |
|
|
| Clinical manifestations |
|
|
| Complications |
|
|
| Diagnosis | Clinical, supported using ELISA ELISA An immunoassay utilizing an antibody labeled with an enzyme marker such as horseradish peroxidase. While either the enzyme or the antibody is bound to an immunosorbent substrate, they both retain their biologic activity; the change in enzyme activity as a result of the enzyme-antibody-antigen reaction is proportional to the concentration of the antigen and can be measured spectrophotometrically or with the naked eye. Many variations of the method have been developed. St. Louis Encephalitis Virus and Western blot | Clinical, dark-field microscopy Dark-field microscopy Treponema, Giemsa stain, or Wright stain of blood smear Blood smear Myeloperoxidase Deficiency |
| Management |
|
|
| Prevention |
|
|
TBRF: tick-borne relapsing fever
LBRF: louse-borne relapsing fever
AV: atrioventricular
ARDS: acute respiratory distress syndrome
ELISA: enzyme-linked immunosorbent assay
PEP: post-exposure prophylaxis
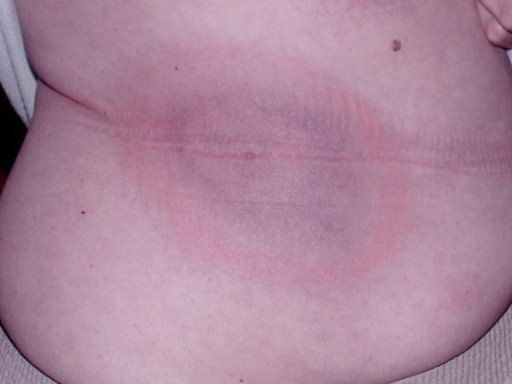
Classic erythema migrans rash of Borrelia burgdorferi
Image: “Diagnostic challenges of early Lyme disease: lessons from a community case series” by Aucott J, Morrison C, Munoz B, Rowe PC, Schwarzwalder A, West SK. License: CC BY 2.0Spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema are gram-negative, spiral-shaped, and motile. The following table briefly compares some clinically relevant spirochetes Spirochetes An order of slender, flexuous, helically coiled bacteria, with one or more complete turns in the helix. Treponema:
| Organism | Treponema pallidum Treponema pallidum The causative agent of venereal and non-venereal syphilis as well as yaws. Treponema pallidum | Other T. pallidum subspecies | Treponema carateum Treponema carateum Treponema | Borrelia burgdorfi | Borrelia recurrentis | Leptospira interrogans Leptospira interrogans A genus of question mark-shaped bacteria spirochetes which is found in freshwater that is contaminated by animal urine. It causes leptospirosis. Leptospira/Leptospirosis |
|---|---|---|---|---|---|---|
| Micro |
|
|
|
|
|
|
| Virulence Virulence The degree of pathogenicity within a group or species of microorganisms or viruses as indicated by case fatality rates and/or the ability of the organism to invade the tissues of the host. The pathogenic capacity of an organism is determined by its virulence factors. Proteus |
|
|
|
|
Antigenic variation |
|
| Reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli | Humans | Humans | Humans |
|
Humans |
|
| Transmission | Sexual contact | P2P contact | P2P contact | Ixodes tick | Louse | Direct contact with animal tissue or fluids |
| Clinical | Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis |
|
Pinta Pinta An infectious disease of the skin caused by treponema carateum that occurs only in the Western hemisphere. Age of onset is between 10 and 20 years of age. This condition is characterized by marked changes in the skin color and is believed to be transmitted by direct person-to-person contact. Yaws, Bejel, and Pinta | Lyme disease Lyme disease Lyme disease is a tick-borne infection caused by the gram-negative spirochete Borrelia burgdorferi. Lyme disease is transmitted by the black-legged Ixodes tick (known as a deer tick), which is only found in specific geographic regions. Patient presentation can vary depending on the stage of the disease and may include a characteristic erythema migrans rash. Lyme Disease | Relapsing fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever |
|
| Diagnosis |
|
Blood-smear analysis |
|
|||
| Management |
|
|
|
|
|
|
Osp: outer surface protein
LPS: lipopolysaccharide
P2P: person-to-person
Microaero: microaerophilic
VDRL: Venereal Disease Research Laboratory test
FTA-ABS: fluorescent treponemal antibody absorption
ELISA: enzyme-linked immunosorbent assay
PCR: polymerase chain reaction
Visual comparison of spirochetes on electron micrograph: thick spirals of Treponema
Image: “Treponema pallidum” by Dr. David Cox. License: Public Domain
Visual comparison of spirochetes on electron micrograph: Borrelia, which are larger than Treponema
Image: “Lyme disease parasite, Borrelia burgdorferi” by Claudia Molins. License: Public Domain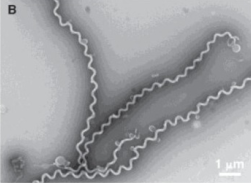
Visual comparison of spirochetes on electron micrograph: hooked ends of Leptospira
Image: “A filtration-based technique for simultaneous SEM and TEM sample preparation for the rapid detection of pathogens” by Beniac DR, Siemens CG, Wright CJ, Booth TF. License: CC BY 3.0, edited by Lecturio.