Yaws, bejel, and pinta are endemic, nonvenereal treponematoses. The causative organisms are Treponema pallidum Treponema pallidum The causative agent of venereal and non-venereal syphilis as well as yaws. Treponema subspecies pertenue (yaws), T. pallidum subspecies endemicum (bejel), and T. carateum T. carateum Treponema (pinta). These treponematoses are generally transmitted by direct skin-to-skin contact with infected skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions. Yaws and bejel affect skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and bones, resulting in cutaneous plaques and nodules and destructive bone lesions Bone Lesions Multiple Myeloma. Pinta involves only the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions. Diagnosis is made with a combination of serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus, clinical features, demographics, and geographic distribution. Management includes intramuscular benzathine penicillin Penicillin Rheumatic Fever G or oral azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides.
Last updated: Feb 25, 2025
Yaws (most common):
Bejel:
Pinta:
Humans are the only reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli.
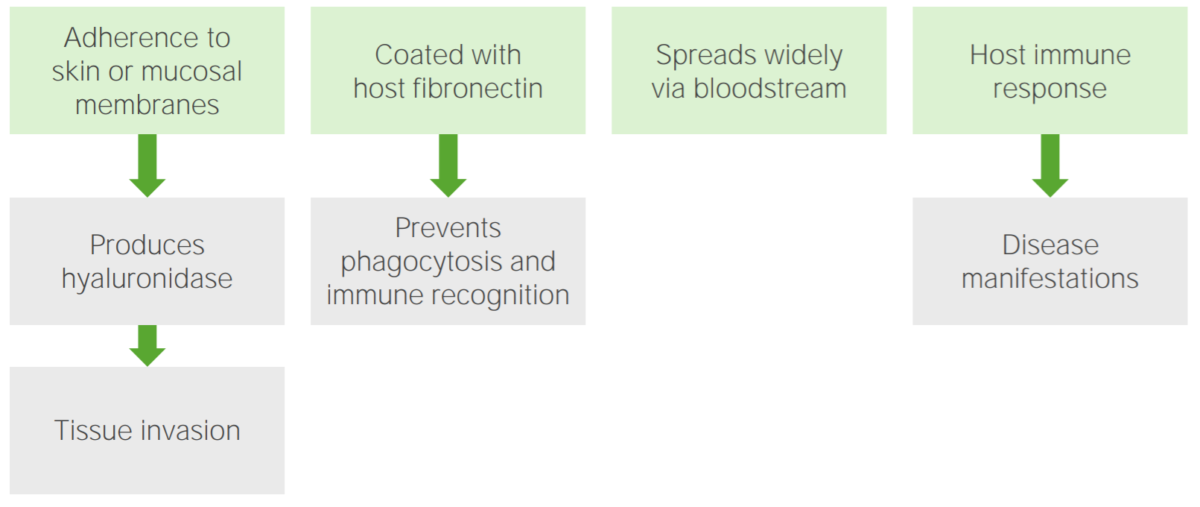
Pathogenesis of Treponema infections:
The pathogen adheres to the skin or mucosal membranes, leading to the production of hyaluronidase, which allows for tissue invasion. The pathogen coats itself in the host’s fibronectin, which prevents its phagocytosis and recognition by the immune system. Consequently, the pathogen disseminates through the bloodstream. A host immune response ultimately occurs, which causes disease manifestations.
Primary phase:
Secondary phase:
Tertiary phase:
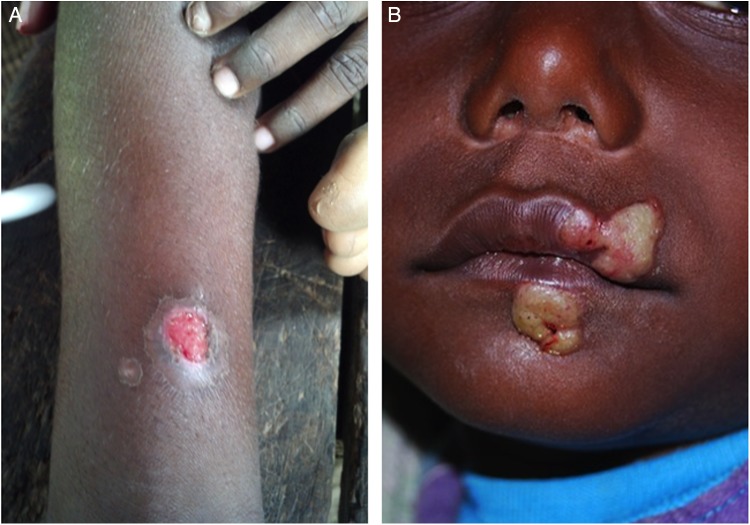
Cutaneous lesions of primary yaws:
A: typical ulcer of primary yaws
B: papilloma of primary yaws

Skin lesions of secondary yaws:
A: crusted maculopapular lesion of secondary yaws
B: multiple ulcers of secondary yaws

Cutaneous manifestation of yaws:
Juxta-articular skin lesions and nodules on the elbow resulting from a Treponema pallidum pertenue infection
Primary phase:
Secondary stage:
Tertiary phase:
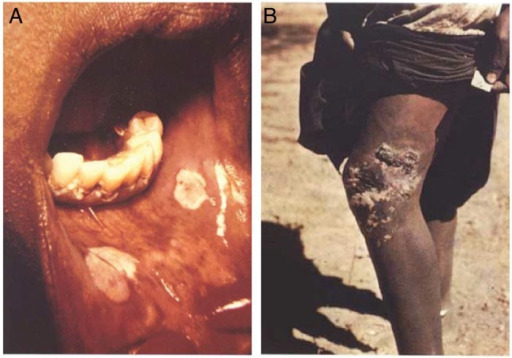
Mucocutaneous lesions of bejel
A: an oral lesion of primary bejel resulting from Treponema pallidum endemicum infection
B: chronic skin lesion of secondary bejel

Gummatous lesions in late-stage bejel (Treponema pallidum endemicum infection)
Image: “Infiltration of skin due to endemic syphilis” by Alireza Abdolrasouli, Adam Croucher, Yahya Hemmati, and David Mabey. License: Public DomainPrimary phase:
Secondary phase:
Tertiary or late phase Late Phase Sepsis in Children:
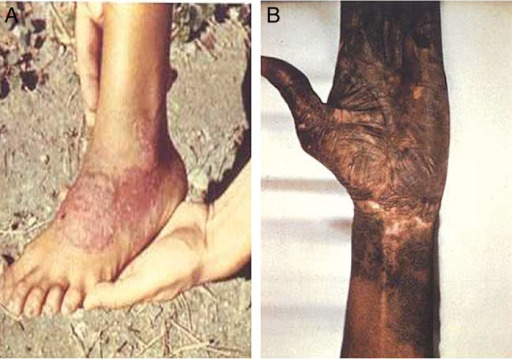
Cutaneous lesions of pinta (Treponema carateum infection)
A: erythematous plaque of early pinta
B: skin discoloration of late pinta
Because these treponemal species are morphologically indistinguishable, the diagnosis is based on the combination of demographics, geographic region, clinical presentation, and laboratory findings.
Serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus:
Direct methods:
Treatment is the same for all of these infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. Options include: