Babesiosis is an infection caused by a protozoa Protozoa Nitroimidazoles belonging to the genus, Babesia. The most common Babesia seen in the United States is B. microti, which is transmitted by the Ixodes tick. The protozoa Protozoa Nitroimidazoles thrive and replicate within host erythrocytes Erythrocytes Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology. Lysis of erythrocytes Erythrocytes Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology and the body’s immune response result in clinical symptoms. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship usually present with a flu-like illness and jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice. In severe cases, organ damage may occur. The diagnosis is confirmed by the visual presence of parasites within RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology, which are often noted to be in a “Maltese Cross” configuration. Serological testing and PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) are also used in the diagnosis. Azithromycin Azithromycin A semi-synthetic macrolide antibiotic structurally related to erythromycin. It has been used in the treatment of Mycobacterium avium intracellulare infections, toxoplasmosis, and cryptosporidiosis. Macrolides and Ketolides and atovaquone Atovaquone A hydroxynaphthoquinone that has antimicrobial activity and is being used in antimalarial protocols. Antimalarial Drugs are often used in management. Coinfection with Borrelia Borrelia Borrelia are gram-negative microaerophilic spirochetes. Owing to their small size, they are not easily seen on Gram stain but can be visualized using dark-field microscopy, Giemsa, or Wright stain. Spirochetes are motile and move in a characteristic spinning fashion due to axial filaments in the periplasmic space. Borrelia and Anaplasma is common.
Last updated: Dec 28, 2024
For babesiosis:
For severe disease:
Outside a human host:
Inside a human host:
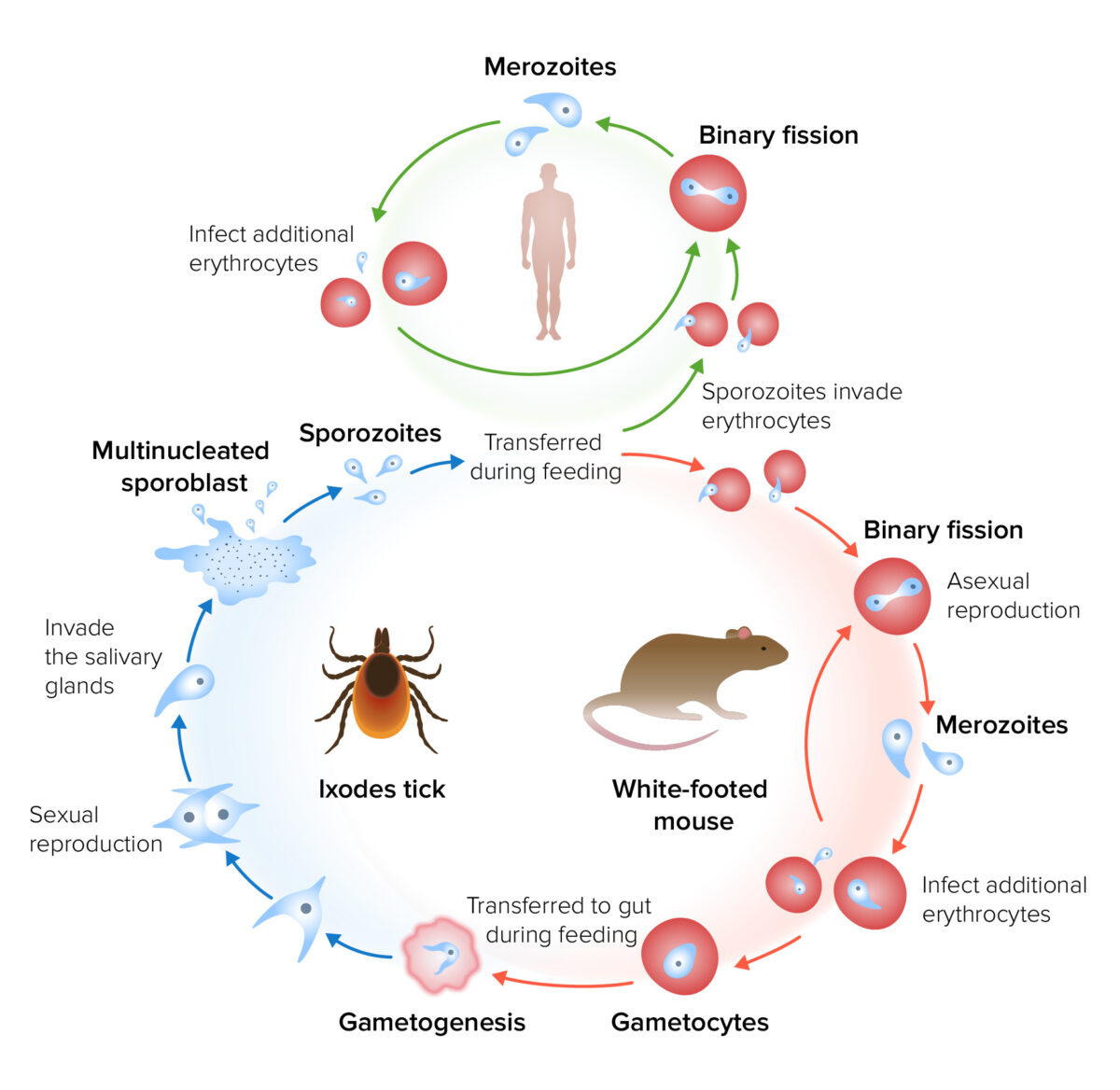
Life cycle and transmission of Babesia
Image by Lecturio.The incubation Incubation The amount time between exposure to an infectious agent and becoming symptomatic. Rabies Virus period for babesiosis is 1–4 weeks.
Mild-to-moderate disease:
Severe disease:
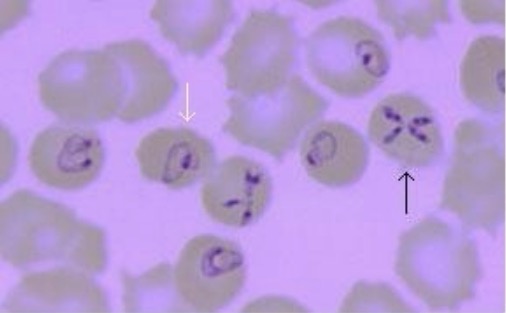
Peripheral blood smear demonstrating Babesia infection:
White arrow indicates pleomorphic, ring-like structures often found in Babesia infections. Black arrow shows the classic “Maltese Cross,” which is pathognomonic for babesiosis.
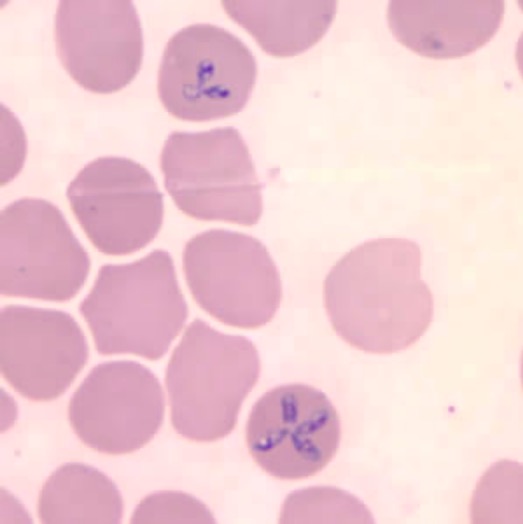
Blood smear showing RBCs infected with Babesia microti
Image: “Babesia microti” by U.S. Centers for Disease Control. License: Public DomainThe mainstay of treatment is antibiotics and educating individuals on preventive methods to avoid tick bites.
Precautions should be taken in endemic areas, particularly in individuals at risk for severe disease and complications.
The table below summarizes the characteristics of parasites that infect RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology.
| Organism | Babesia | Plasmodium Plasmodium A genus of protozoa that comprise the malaria parasites of mammals. Four species infect humans (although occasional infections with primate malarias may occur). These are plasmodium falciparum; plasmodium malariae; plasmodium ovale, and plasmodium vivax. Species causing infection in vertebrates other than man include: plasmodium berghei; plasmodium chabaudi; p. Vinckei, and plasmodium yoelii in rodents; p. Brasilianum, plasmodium cynomolgi; and plasmodium knowlesi in monkeys; and plasmodium gallinaceum in chickens. Antimalarial Drugs |
|---|---|---|
| Disease | Babesiosis | Malaria Malaria Malaria is an infectious parasitic disease affecting humans and other animals. Most commonly transmitted via the bite of a female Anopheles mosquito infected with microorganisms of the Plasmodium genus. Patients present with fever, chills, myalgia, headache, and diaphoresis. Plasmodium/Malaria |
| Microscopic appearance |
|
|
| Reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli | White-footed mouse |
|
| Transmission | Ixodes tick | Anopheles Anopheles A genus of mosquitoes (culicidae) that are known vectors of malaria. Plasmodium/Malaria mosquito |
| Common regions |
|
|
| Clinical |
|
|
| Diagnosis |
|
|
| Management |
|
Depends on species, severity, and
resistance
Resistance
Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow.
Ventilation: Mechanics of Breathing patterns, but may include a combination of:
|