Disseminated intravascular coagulation (DIC) is a condition characterized by systemic bodywide activation of the coagulation cascade Coagulation cascade The coagulation cascade is a series of reactions that ultimately generates a strong, cross-linked fibrin clot. Hemostasis. This cascade results in both widespread microvascular thrombi contributing to multiple organ dysfunction and consumption of clotting factors and platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology, leading to hemorrhage. DIC is always triggered by another (often serious) condition, including severe sepsis Severe Sepsis Sepsis in Children, trauma, malignancy Malignancy Hemothorax, or obstetric complications. Acute DIC often presents dramatically, with rapid onset of spontaneous bleeding from multiple locations throughout the body simultaneously. A chronic form of DIC also exists, typically in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with late-stage malignancies. Management involves stabilizing the patient, replacing consumed platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology and coagulation factors Coagulation factors Endogenous substances, usually proteins, that are involved in the blood coagulation process. Hemostasis, and treating the triggering condition.
Last updated: Dec 30, 2024
Disseminated intravascular coagulation (DIC) is a condition characterized by systemic bodywide activation of the coagulation cascade Coagulation cascade The coagulation cascade is a series of reactions that ultimately generates a strong, cross-linked fibrin clot. Hemostasis that results in both:
Acute DIC:
Chronic DIC:
Disseminated intravascular coagulation is always a complication of other conditions:
| Infection |
|
|---|---|
| Inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation |
|
| Malignancy Malignancy Hemothorax |
|
| Obstetric causes |
|
| Trauma |
|
| Hematologic and vascular causes |
|
In DIC, coagulation and subsequent fibrinolysis are activated systemically, which is abnormal and leads to microthrombi throughout the vasculature. These microthrombi consume large amounts of platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology and coagulation factors Coagulation factors Endogenous substances, usually proteins, that are involved in the blood coagulation process. Hemostasis, leading to a severe coagulopathy and clinical bleeding.
Acute DIC is decompensated DIC:
Chronic DIC is compensated DIC:
Acute DIC typically presents rapidly and dramatically, with acute and severe bleeding from multiple sites simultaneously throughout the body. Other manifestations are related to thrombotic end-organ dysfunction.
| Vital signs |
|
|---|---|
| Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions |
|
| Mucosal |
|
| Renal |
|
| Pulmonary |
|
| GI |
|
| Neurologic |
|

Skin manifestation of DIC:
Note the petechiae and purpura.
The diagnosis is made on the basis of clinical history and laboratory findings, though no single test is diagnostic for DIC. Laboratory tests also aid in management.
In DIC, coagulation factors Coagulation factors Endogenous substances, usually proteins, that are involved in the blood coagulation process. Hemostasis and platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology are rapidly consumed in the formation of systemwide microthrombi. Lab findings in DIC include:
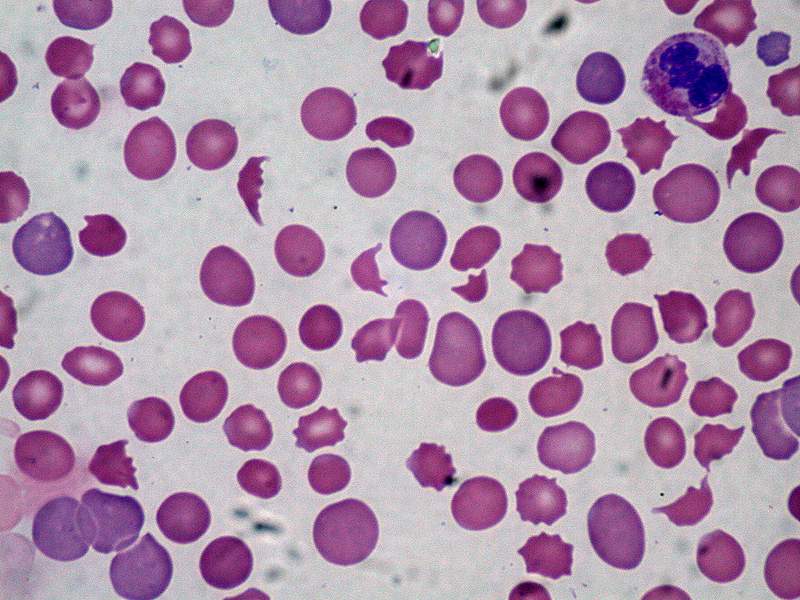
Peripheral blood smear showing schistocytes, which are indicative of intravascular hemolysis
Image: “Disseminated carcinomatosis with DIC” by Ed Uthman, MD. License: Public DomainNo specific imaging study confirms the diagnosis of DIC. Specific imaging methods may be indicated to assist in:
The most important principles in management are to treat the underlying cause and stabilize the patient.