Postpartum hemorrhage is one of the most common and deadly obstetric complications. Since 2017, postpartum hemorrhage has been defined as blood loss greater than 1,000 mL for both cesarean and vaginal deliveries, or excessive blood loss with signs of hemodynamic instability. Blood loss of more than 500 mL following a vaginal delivery is considered abnormal, though no longer classified as postpartum hemorrhage. The most common cause of postpartum hemorrhage is uterine atony. Retained products of conception, trauma, and coagulopathies Coagulopathies Hemothorax may also cause postpartum hemorrhage. Appropriate management requires rapid identification Identification Defense Mechanisms of the cause of the hemorrhage, medical and/or surgical correction, and patient resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome.
Last updated: Sep 29, 2022
Postpartum hemorrhage is defined as excessive blood loss following the delivery of an infant > 20 weeks gestational age Gestational age The age of the conceptus, beginning from the time of fertilization. In clinical obstetrics, the gestational age is often estimated as the time from the last day of the last menstruation which is about 2 weeks before ovulation and fertilization. Pregnancy: Diagnosis, Physiology, and Care.
The primary etiologies can be remembered as “the 4 Ts” (tone, tissue, trauma, and thrombin Thrombin An enzyme formed from prothrombin that converts fibrinogen to fibrin. Hemostasis).
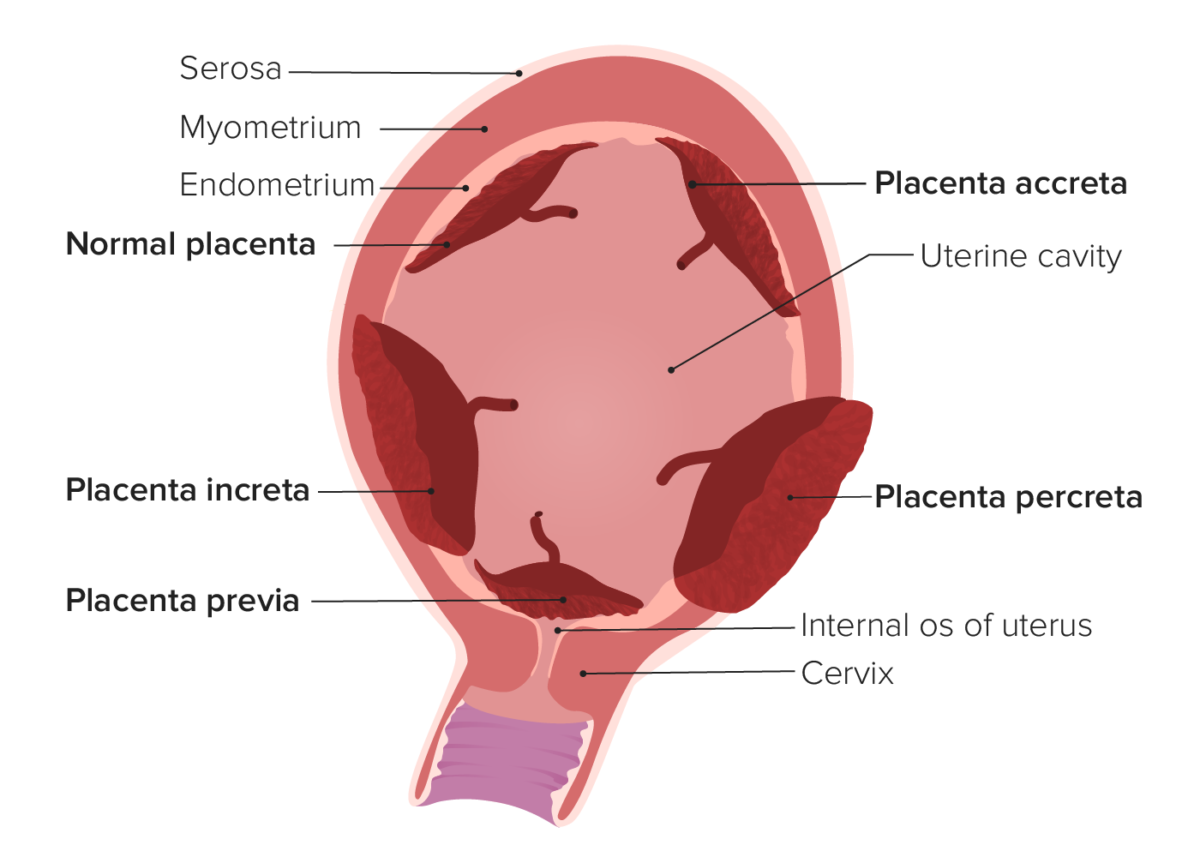
Types of abnormal placentation.
In placenta accreta, the placenta attaches (at least in part) to the underlying myometrium. In placenta increta, the placental villi actually invade into the myometrium. In placenta percreta, the placental villi invade through the entire uterine wall and may invade surrounding structures (e.g., the bladder). Placenta previa occurs when the placenta covers the internal cervical os.
Postpartum hemorrhage due to a nontraumatic etiology results when 1 or both of the primary mechanisms required for normal postpartum hemostasis Hemostasis Hemostasis refers to the innate, stepwise body processes that occur following vessel injury, resulting in clot formation and cessation of bleeding. Hemostasis occurs in 2 phases, namely, primary and secondary. Primary hemostasis involves forming a plug that stops the bleeding temporarily. Secondary hemostasis involves the activation of the coagulation cascade. Hemostasis are disrupted. The 2 primary mechanisms are mechanical hemostasis Hemostasis Hemostasis refers to the innate, stepwise body processes that occur following vessel injury, resulting in clot formation and cessation of bleeding. Hemostasis occurs in 2 phases, namely, primary and secondary. Primary hemostasis involves forming a plug that stops the bleeding temporarily. Secondary hemostasis involves the activation of the coagulation cascade. Hemostasis and hemostatic factors.
Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with heavy bleeding and/or signs of hemodynamic instability. Diagnosis is usually clinical.
The 4 classes of hemorrhage are described by the Advanced Trauma Life Support manual, which can also classify postpartum hemorrhage.
| Class | Percentage of blood volume lost | Clinical findings |
|---|---|---|
| Class I | Up to 15% | Mild tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children |
| Class II | 15%–30% |
|
| Class III | 30%–40% |
|
| Class IV | > 40% |
|
| Medication (generic) | Class | Route | Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation |
|---|---|---|---|
| Oxytocin | Natural hormone | IV, IM | None |
| Methylergonovine | Ergot alkaloid | IM | Hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension |
| Carboprost Carboprost A nonsteroidal abortifacient agent that is effective in both the first and second trimesters of pregnancy. Eicosanoids (PGF2α) | Prostaglandin analogue | IM | Severe hepatic, renal, and cardiovascular disease, and asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma |
| Misoprostol Misoprostol A synthetic analog of natural prostaglandin e1. It produces a dose-related inhibition of gastric acid and pepsin secretion, and enhances mucosal resistance to injury. It is an effective anti-ulcer agent and also has oxytocic properties. Eicosanoids | Prostaglandin analogue | Oral, rectal | None |
Activate the hospital’s massive transfusion protocol and administer blood products: