For Clinical Practice Version: Click here
Deep vein thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus (DVT) is a blood clot in the deep veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology, usually in the lower extremities (though they can occur in the upper extremities, mesenteric, and cerebral veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology as well). The affected veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology commonly include the popliteal, femoral, iliac, and pelvic veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology. The 3 primary factors (known as the Virchow triad) that contribute to DVT formation include: venous stasis, hypercoagulability Hypercoagulability Hypercoagulable States, and vascular endothelial damage. Any condition that worsens 1 (or more) of these 3 factors increases the risk of DVT formation. Individuals can present with unilateral extremity pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, swelling Swelling Inflammation, and/or redness Redness Inflammation around the DVT; however, a majority of cases are asymptomatic. Ultrasound can visualize the thrombus. Anticoagulation Anticoagulation Pulmonary Hypertension Drugs is the primary mode of treatment; the main objective is preventing a pulmonary embolism Pulmonary Embolism Pulmonary embolism (PE) is a potentially fatal condition that occurs as a result of intraluminal obstruction of the main pulmonary artery or its branches. The causative factors include thrombi, air, amniotic fluid, and fat. In PE, gas exchange is impaired due to the decreased return of deoxygenated blood to the lungs. Pulmonary Embolism (PE).
Last updated: Jul 10, 2023
The 3 primary factors (known as the Virchow triad) that contribute to DVT formation include: venous stasis, hypercoagulability Hypercoagulability Hypercoagulable States, and vascular endothelial damage. Any condition which worsens one (or more) of these three factors increases the risk of DVT formation.
Factors resulting in endothelial damage:
Factors resulting in venous stasis:
Factors resulting in hypercoagulability Hypercoagulability Hypercoagulable States:
Other risk factors and/or conditions affecting multiple components of the Virchow triad:
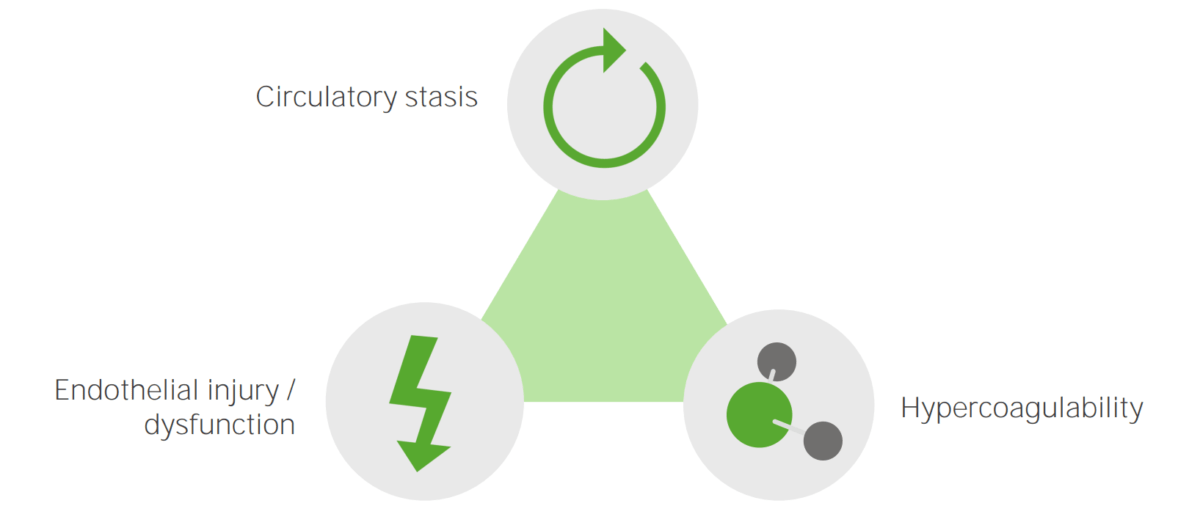
The primary etiologic factors that cause DVT: circulatory stasis, endothelial injury or dysfunction, and hypercoagulability
Image by Lecturio.To remember DVT risk factors, think THROMBOSIS Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus.
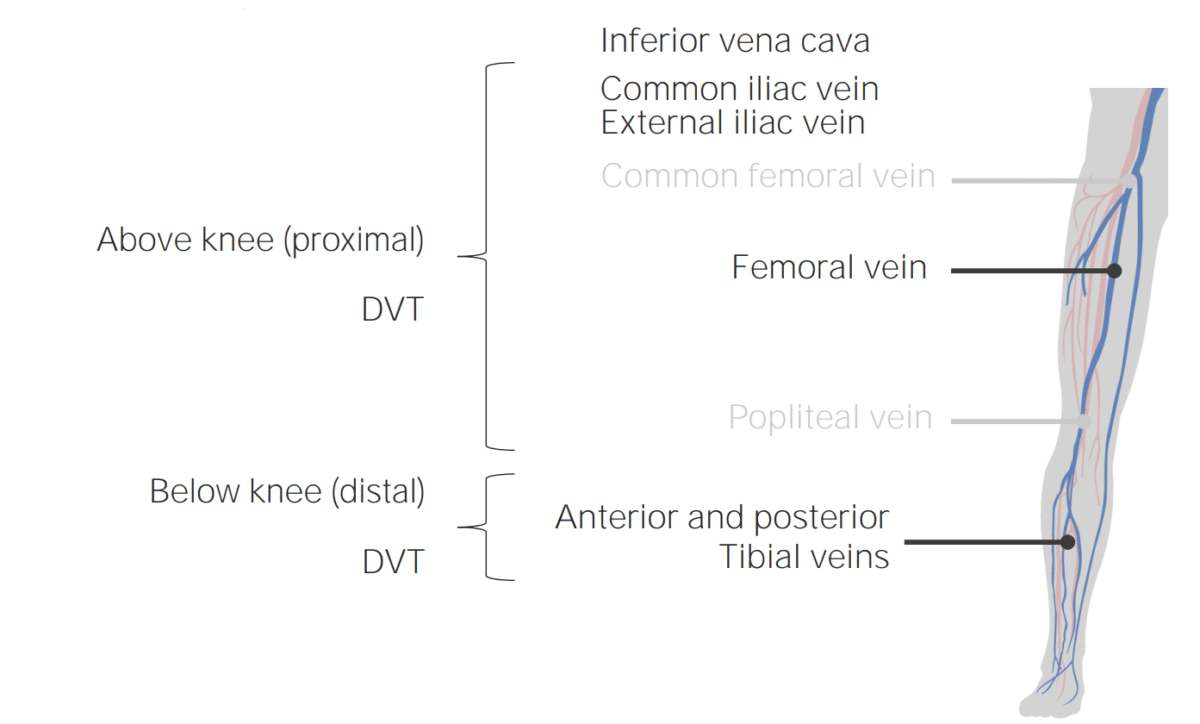
Common locations of DVT.
Image by Lecturio.
The image shows erythema, swelling, and cyanosis in a patient with phlegmasia cerulea dolens.
a) Initial appearance of the left leg, showing significant swelling and cyanosis
b) Appearance of the left leg 35 days after surgery, at the time of the patient’s discharge
| Tenderness along the deep venous system | +1 |
| Unilateral pitting edema Pitting edema Edema caused by excess fluid without excess colloid. Leaves “pits” due to fluid displacement when pressure is applied to the area Edema | +1 |
| Swelling Swelling Inflammation of the entire leg Leg The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint. The bony structure is composed of the tibia and fibula bones, and the muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia. Leg: Anatomy | +1 |
| Calf swelling Swelling Inflammation ≥ 3 cm (compared to asymptomatic calf) | +1 |
| Collateral superficial non-varicose veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology | +1 |
| Active cancer | +1 |
| Previous DVT | +1 |
| Paralysis or cast immobilization Immobilization Delirium | +1 |
| Bedridden ≥ 3 days or major surgery within past 4 weeks | +1 |
| Alternative diagnosis as likely/more likely than DVT | -2 |
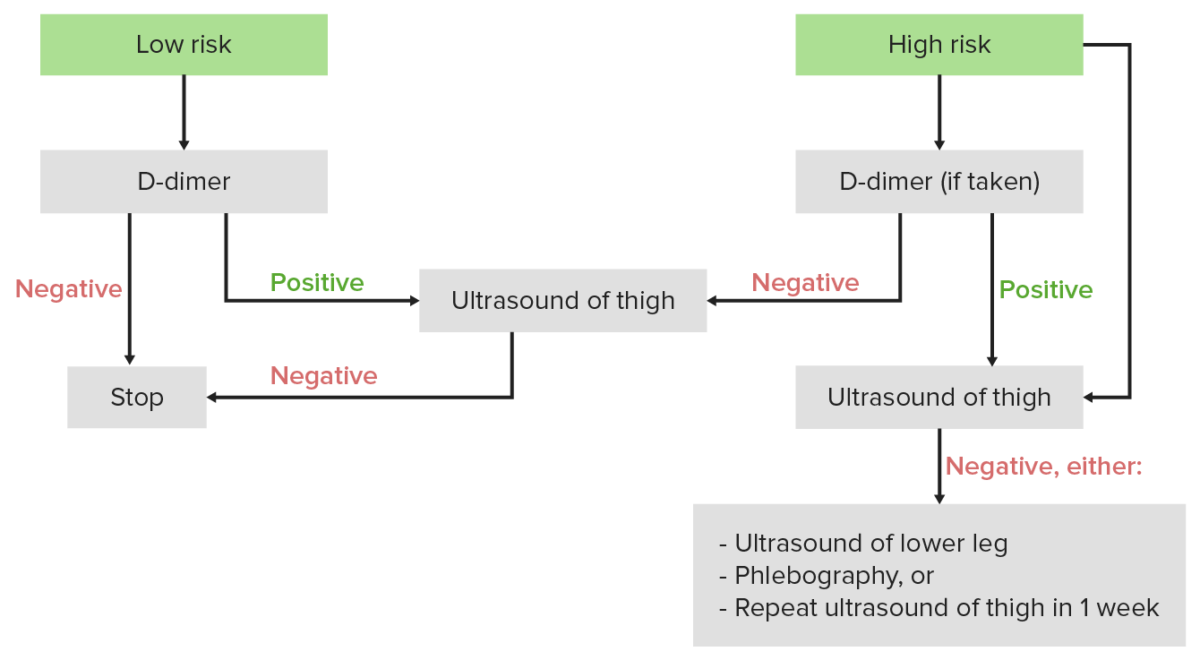
Diagnostic algorithm for DVT: If the Wells score is < 2, the individual is considered low risk, and the 1st test should be a D-dimer. If the Wells score is ≥ 2, the individual is considered high risk, and the 1st test should be an ultrasound.
Image by Lecturio.Anticoagulation Anticoagulation Pulmonary Hypertension Drugs is the mainstay of therapy for DVTs. Depending on the situation, some individuals may require thrombolysis, an invasive procedure, and/or lifelong anticoagulation Anticoagulation Pulmonary Hypertension Drugs.
The following conditions can present similarly to DVT: