Cirrhosis is a late stage of hepatic parenchymal necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage and scarring Scarring Inflammation ( fibrosis Fibrosis Any pathological condition where fibrous connective tissue invades any organ, usually as a consequence of inflammation or other injury. Bronchiolitis Obliterans) most commonly due to hepatitis C Hepatitis C Hepatitis C is an infection of the liver caused by the hepatitis C virus (HCV). The infection can be transmitted through infectious blood or body fluids and may be transmitted during childbirth or through IV drug use or sexual intercourse. Hepatitis C virus can cause both acute and chronic hepatitis, ranging from a mild to a serious, lifelong illness including liver cirrhosis and hepatocellular carcinoma (HCC). Hepatitis C Virus infection and alcoholic Alcoholic Persons who have a history of physical or psychological dependence on ethanol. Mallory-Weiss Syndrome (Mallory-Weiss Tear) liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may present with jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice, ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites, and hepatosplenomegaly Hepatosplenomegaly Cytomegalovirus. Cirrhosis can also cause complications such as hepatic encephalopathy Encephalopathy Hyper-IgM Syndrome, portal hypertension Portal hypertension Portal hypertension is increased pressure in the portal venous system. This increased pressure can lead to splanchnic vasodilation, collateral blood flow through portosystemic anastomoses, and increased hydrostatic pressure. There are a number of etiologies, including cirrhosis, right-sided congestive heart failure, schistosomiasis, portal vein thrombosis, hepatitis, and Budd-Chiari syndrome. Portal Hypertension, portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus, and hepatorenal syndrome Hepatorenal Syndrome Hepatorenal syndrome (HRS) is a potentially reversible cause of acute kidney injury that develops secondary to liver disease. The main cause of HRS is hypovolemia, often as a result of forced diuresis or drainage of ascites. This leads to renal vasoconstriction resulting in hypoperfusion of the kidneys. Hepatorenal Syndrome. Diagnosis is clinical. Management requires treating the underlying disease, managing complications, and, if required, liver transplantation Liver transplantation The transference of a part of or an entire liver from one human or animal to another. Hepatocellular Carcinoma (HCC) and Liver Metastases.
Last updated: Jun 3, 2025
Leading causes of cirrhosis in resource-abundant countries:
Overview of potential causes:
Cirrhosis due to alcoholic liver disease
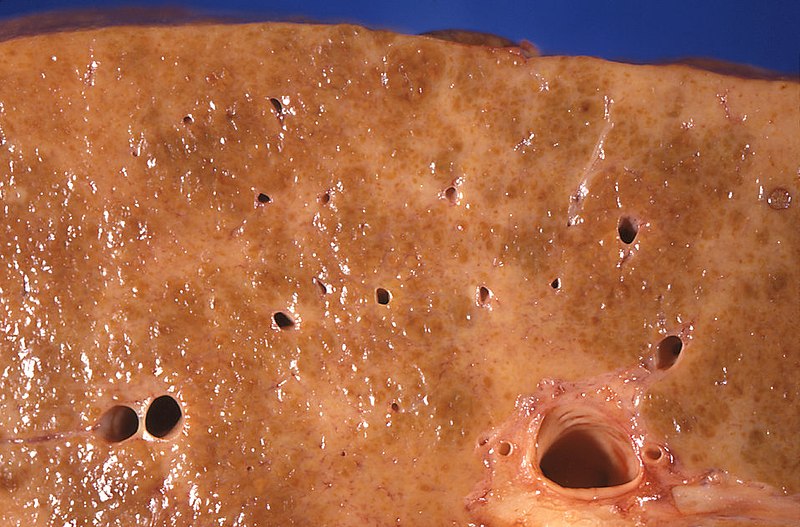
Image: “Gross pathology of alcoholic liver cirrhosis” by Centers for Disease Control and Prevention/ Dr. Edwin P. Ewing, Jr. License: CC0 1.0Cirrhosis is liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy damage that is characterized by diffuse distortion Distortion Defense Mechanisms of the basic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy architecture and replacement with scar Scar Dermatologic Examination tissue and regenerative nodules.
The Child-Pugh score is used to estimate life expectancy Life expectancy Based on known statistical data, the number of years which any person of a given age may reasonably expected to live. Population Pyramids. It serves as the basis for the treatment regimen and transplant eligibility.
| Classification | 1 point | 2 points | 3 points |
|---|---|---|---|
| Serum bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism (mg/dL) | < 2.0 | 2.0–3.0 | > 3.0 |
| Serum albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests (g/dL) | > 3.5 | 2.8–3.5 | < 2.8 |
| International normalized ratio International normalized ratio System established by the world health organization and the international committee on thrombosis and hemostasis for monitoring and reporting blood coagulation tests. Under this system, results are standardized using the international sensitivity index for the particular test reagent/instrument combination used. Hemostasis (INR) | < 1.7 | 1.7–2.3 | > 2.3 |
| Presence of ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites | None | Mild | Moderate |
| Hepatic encephalopathy Encephalopathy Hyper-IgM Syndrome | None | Minimal | Advanced |
The sum of the points determines the class and the expected remaining life expectancy Life expectancy Based on known statistical data, the number of years which any person of a given age may reasonably expected to live. Population Pyramids:
| Points | Class | Life expectancy Life expectancy Based on known statistical data, the number of years which any person of a given age may reasonably expected to live. Population Pyramids |
|---|---|---|
| 5–6 | A | 15–50 years |
| 7–9 | B | 4–14 years |
| 10–15 | C | 1–3 years |

Ascites secondary to hepatic cirrhosis being drained via paracentesis
Image: “Draining ascites, secondary to hepatic cirrhosis” by John Campbell. License: Public Domain
Jaundice: yellow discoloration of the skin due to bilirubin deposition
Image: “Jaundice08” by James Heilman, MD. License: CC BY 3.0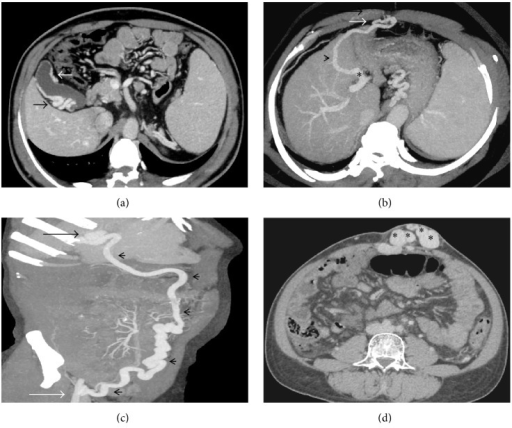
(a) Axial CECT image showing multiple pericholecystic collaterals (arrows); (b) axial-oblique MIP image showing a right infradiaphragmatic type of shunt (arrowhead) arising from the left portal vein branch (asterisk) and draining into the intercostal vein; (c) coronal-oblique MIP image demonstrating a prominent recanalized paraumbilical vein (arrowheads) arising from the left branch of portal vein (black arrow) and draining into the right internal iliac vein (white arrow); (d) caput medusa, multiple periumbilical abdominal wall varices (asterisks).
Image: “caput medusae” by US National Library of Medicine. License: CC BY 4.0
Symptoms resulting from portal hypertension
Image by Lecturio.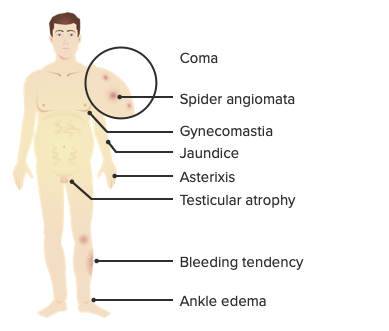
Symptoms resulting from liver cell failure
Image by Lecturio.Cirrhosis can be diagnosed via clinical signs, laboratory testing, and ultrasound. The definitive diagnosis and classification is histopathologic (gold standard), which shows fibrosis Fibrosis Any pathological condition where fibrous connective tissue invades any organ, usually as a consequence of inflammation or other injury. Bronchiolitis Obliterans and replacement of normal liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy tissue with collagenous regenerative nodules. However, a biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is usually not necessary if the clinical, laboratory, and radiologic data are strongly suggestive of cirrhosis.
| Type | Size of the regenerative nodules | Etiology |
|---|---|---|
| Micronodular | 1–3 mm |
|
| Macronodular (also called post-necrotic cirrhosis | > 3 mm |
|
Liver function tests Liver function tests Liver function tests, also known as hepatic function panels, are one of the most commonly performed screening blood tests. Such tests are also used to detect, evaluate, and monitor acute and chronic liver diseases. Liver Function Tests:
Liver function tests Liver function tests Liver function tests, also known as hepatic function panels, are one of the most commonly performed screening blood tests. Such tests are also used to detect, evaluate, and monitor acute and chronic liver diseases. Liver Function Tests are an unreliable indicator Indicator Methods for assessing flow through a system by injection of a known quantity of an indicator, such as a dye, radionuclide, or chilled liquid, into the system and monitoring its concentration over time at a specific point in the system. Body Fluid Compartments of liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy damage. High levels are predictive of liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy damage, but low levels do not rule out liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy damage (especially cirrhosis).
Early findings of cirrhosis:
Late findings of cirrhosis:
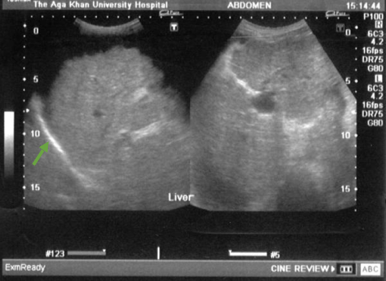
Cirrhosis: nodular, coarse echotexture (arrow) of the liver
Image: “Ultrasound upper abdomen showing coarse liver parenchyma, irregular margins of liver, parahepatic ascities” by Subhan et al; licensee BioMed Central Ltd. License: CC BY 2.0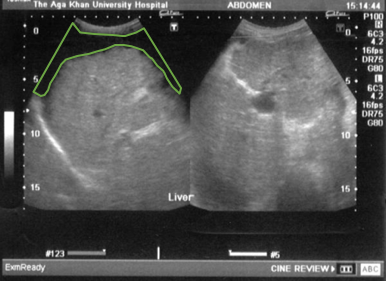
Cirrhosis: ascites (outlined in green) and splenomegaly
Image: “Ultrasound upper abdomen showing coarse liver parenchyma, irregular margins of liver, parahepatic ascities” by Subhan et al; licensee BioMed Central Ltd. License: CC BY 2.0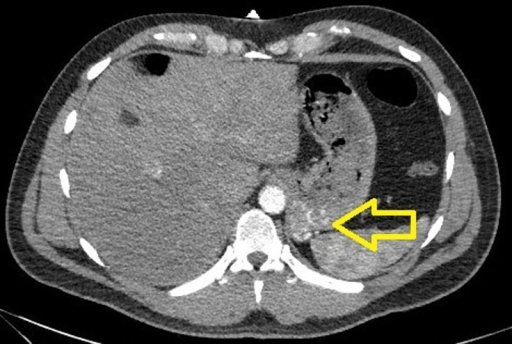
CT scan showing gastric varices
Image: “CTA of the abdomen showing a small tangle of enlarged tortuous blood vessels along the posterior cardia of the stomach” by U.S. National Library of Medicine. License: CC BY 3.0Cirrhosis complications: VARICES

Endoscopic view of the esophageal varices
Image: “Gastroscopy image of esophageal varices with prominent red wale spots” by Samir. License: Public Domain