Hypogonadism is a condition characterized by reduced or no sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria hormone production by the testes Testes Gonadal Hormones or ovaries Ovaries Ovaries are the paired gonads of the female reproductive system that contain haploid gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis, just posterior to the broad ligament, and are connected to the pelvic sidewall and to the uterus by ligaments. These organs function to secrete hormones (estrogen and progesterone) and to produce the female germ cells (oocytes). Ovaries: Anatomy. Hypogonadism can result from primary (hypergonadotropic) or secondary (hypogonadotropic) failure. Hypergonadotropic hypogonadism results when the gonads Gonads The gamete-producing glands, ovary or testis. Hormones: Overview and Types fail to produce sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria hormone, and hypogonadotropic hypogonadism results from failures in the hypothalamic– pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types–gonadal axis. Symptoms include infertility Infertility Infertility is the inability to conceive in the context of regular intercourse. The most common causes of infertility in women are related to ovulatory dysfunction or tubal obstruction, whereas, in men, abnormal sperm is a common cause. Infertility, increased risk of osteoporosis Osteoporosis Osteoporosis refers to a decrease in bone mass and density leading to an increased number of fractures. There are 2 forms of osteoporosis: primary, which is commonly postmenopausal or senile; and secondary, which is a manifestation of immobilization, underlying medical disorders, or long-term use of certain medications. Osteoporosis, erectile dysfunction Erectile Dysfunction Erectile dysfunction (ED) is defined as the inability to achieve or maintain a penile erection, resulting in difficulty to perform penetrative sexual intercourse. Local penile factors and systemic diseases, including diabetes, cardiac disease, and neurological disorders, can cause ED. Erectile Dysfunction, decreased libido, and regression Regression Corneal Abrasions, Erosion, and Ulcers (or absence) of secondary sexual characteristics Secondary Sexual Characteristics Precocious Puberty. Diagnosis is guided by the history, physical exam, measurement of hormone levels, and an evaluation for an underlying etiology. Management is with hormone replacement.
Last updated: Apr 4, 2023
Hypogonadism is a condition in which there is decreased sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria hormone production by the testes Testes Gonadal Hormones or ovaries Ovaries Ovaries are the paired gonads of the female reproductive system that contain haploid gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis, just posterior to the broad ligament, and are connected to the pelvic sidewall and to the uterus by ligaments. These organs function to secrete hormones (estrogen and progesterone) and to produce the female germ cells (oocytes). Ovaries: Anatomy.
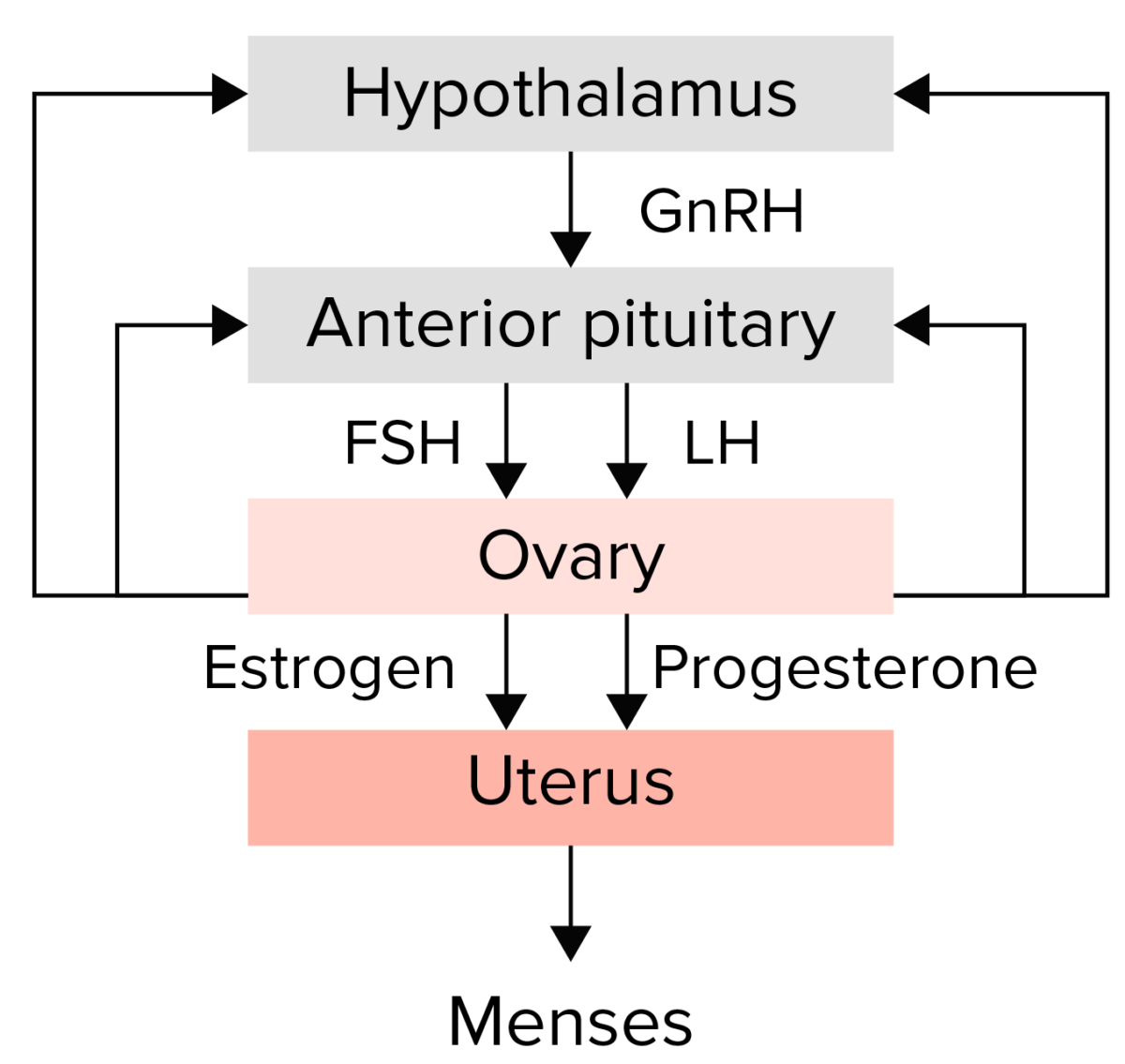
Summary of the hypothalamic–pituitary–ovarian axis:
The hypothalamus secretes gonadotropin-releasing hormone (GnRH), which stimulates the anterior pituitary to release the gonadotropins follicle-stimulating hormone (FSH) and luteinizing hormone (LH). The gonadotropins then stimulate the ovary to produce estrogen and progesterone, which in turn lead to endometrial growth and maturation. Any disruption in this pathway could lead to amenorrhea.
Hypogonadism occurs if the hypothalamic– pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types–gonadal axis is interrupted at any level.
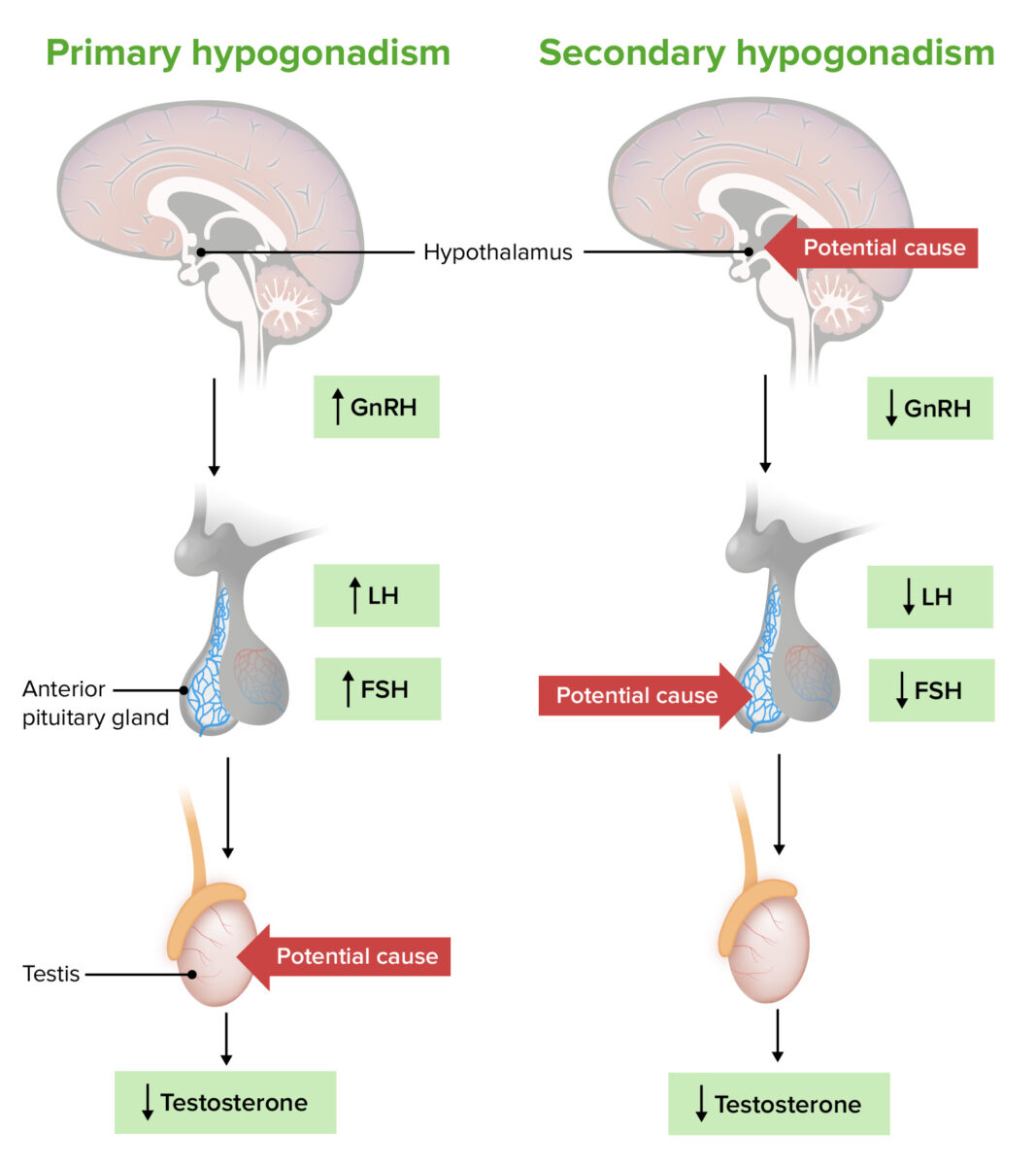
Pathogenesis of primary versus secondary hypogonadism:
Primary hypogonadism results from an issue with the testes (or ovaries), resulting in decreased sex hormone production despite adequate (or high) levels of gonadotropin-releasing hormone (GnRH), luteinizing hormone (LH), and follicle-stimulating hormone (FSH).
In secondary hypogonadism, an issue in the hypothalamus or pituitary gland results in decreased GnRH, LH, and FSH, resulting in decreased sex hormone production (despite normal testes or ovaries).
Clinical presentation will vary depending on the age at onset and sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria.
Men:
Women: