Hyperprolactinemia is defined as a condition of elevated levels of prolactin Prolactin A lactogenic hormone secreted by the adenohypophysis. It is a polypeptide of approximately 23 kd. Besides its major action on lactation, in some species prolactin exerts effects on reproduction, maternal behavior, fat metabolism, immunomodulation and osmoregulation. Breasts: Anatomy (PRL) hormone in the blood. The PRL hormone is secreted by the anterior pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types gland and is responsible for breast development and lactation Lactation The processes of milk secretion by the maternal mammary glands after parturition. The proliferation of the mammary glandular tissue, milk synthesis, and milk expulsion or let down are regulated by the interactions of several hormones including estradiol; progesterone; prolactin; and oxytocin. Breastfeeding. Many factors contribute to the development of hyperprolactinemia. The most common cause is PRL-secreting pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types adenomas (prolactinomas). Diagnosis is achieved through hormonal testing to rule out other endocrine conditions and confirmatory imaging tests. Dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS agonists are the 1st-line drugs for treatment. Refractory cases require surgery and possibly radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy.
Last updated: May 17, 2024
Hyperprolactinemia means abnormally high levels of prolactin Prolactin A lactogenic hormone secreted by the adenohypophysis. It is a polypeptide of approximately 23 kd. Besides its major action on lactation, in some species prolactin exerts effects on reproduction, maternal behavior, fat metabolism, immunomodulation and osmoregulation. Breasts: Anatomy (PRL) in the blood.
Normal PRL levels (may vary according to the lab):
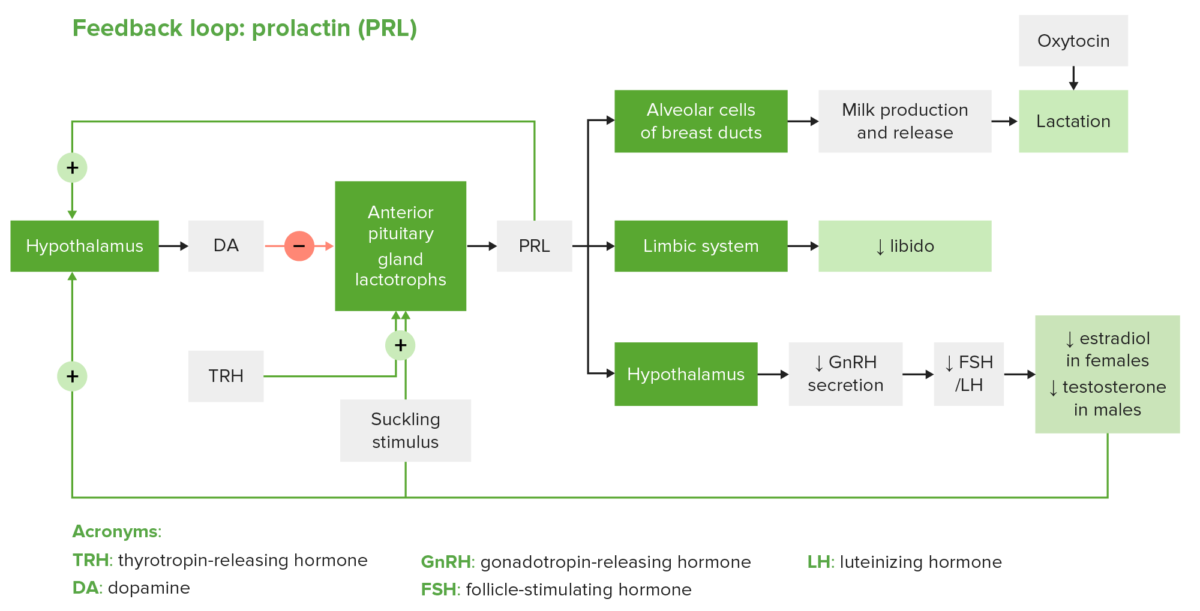
The regulatory feedback loop of PRL: Note that TRH has a stimulatory effect on PRL; however, dopamine is the main regulator of PRL secretion.
Image by Lecturio.Excessive and prolonged increase in PRL levels → suppression Suppression Defense Mechanisms of GnRH → lower levels of LH LH A major gonadotropin secreted by the adenohypophysis. Luteinizing hormone regulates steroid production by the interstitial cells of the testis and the ovary. The preovulatory luteinizing hormone surge in females induces ovulation, and subsequent luteinization of the follicle. Luteinizing hormone consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle, FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle → chronically low estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy and testosterone Testosterone A potent androgenic steroid and major product secreted by the leydig cells of the testis. Its production is stimulated by luteinizing hormone from the pituitary gland. In turn, testosterone exerts feedback control of the pituitary LH and FSH secretion. Depending on the tissues, testosterone can be further converted to dihydrotestosterone or estradiol. Androgens and Antiandrogens → hypogonadotropic hypogonadism Hypogonadotropic Hypogonadism Hypogonadism
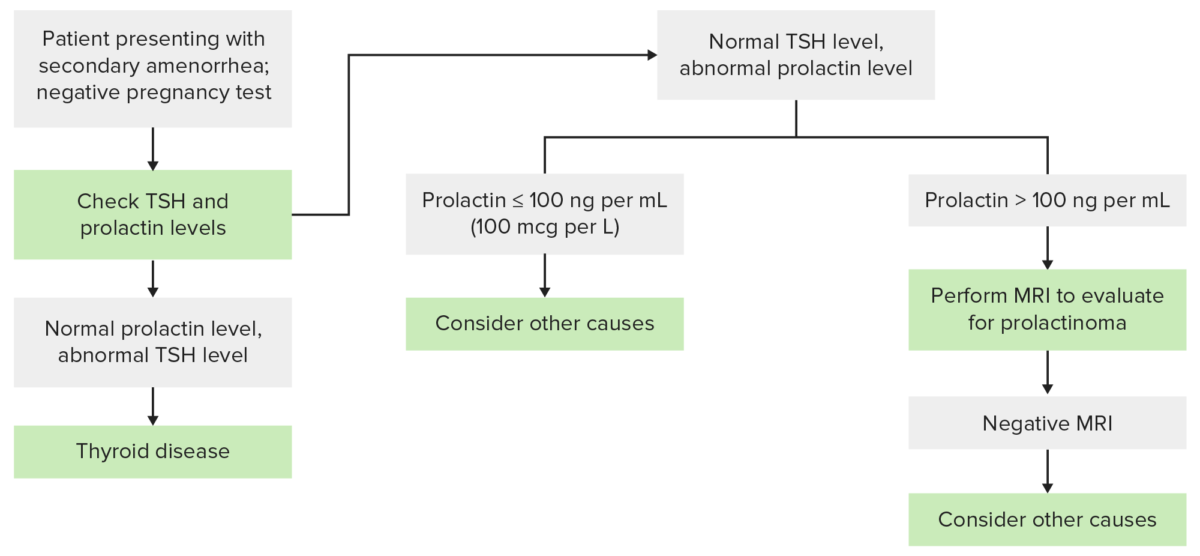
Diagnostic algorithm to follow for a patient presenting with secondary amenorrhea
Image by Lecturio.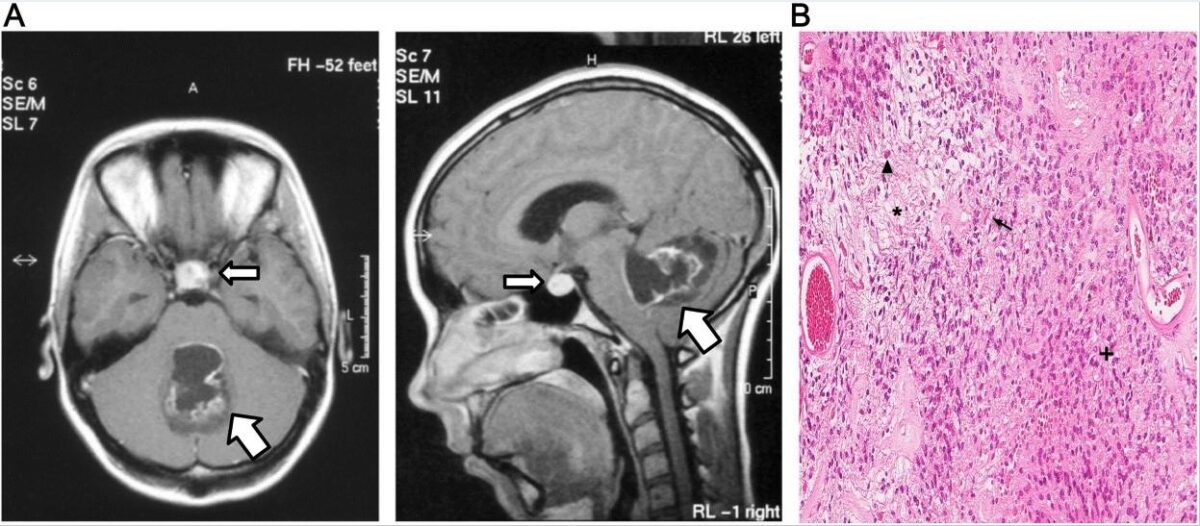
Axial (left) and sagittal (right) MRI images of a prolactinoma (slim arrow)
Image: “Prolactinoma” by Tajana Tešan Tomić et al. License: CC BY 4.0, edited by Lecturio.The following conditions should be ruled out in the case of hyperprolactinemia: