Male sexual dysfunction Sexual dysfunction Physiological disturbances in normal sexual performance in either the male or the female. Sexual Physiology is any disorder that interferes with the male sexual response cycle and includes desire disorders, erectile disorders, and ejaculatory disorders. Sexual dysfunction Sexual dysfunction Physiological disturbances in normal sexual performance in either the male or the female. Sexual Physiology has a varied etiology and may be due to psychological causes, endocrine diseases, neurogenic dysfunction, chronic medical illness, or medication/substance abuse. These disorders often cause significant distress to the patient and sexual partner. Treatment options include psychotherapy Psychotherapy Psychotherapy is interpersonal treatment based on the understanding of psychological principles and mechanisms of mental disease. The treatment approach is often individualized, depending on the psychiatric condition(s) or circumstance. Psychotherapy, physical therapy Physical Therapy Becker Muscular Dystrophy, and pharmacotherapy based on the causes of dysfunction.
Last updated: Apr 14, 2025
Male sexual dysfunction Sexual dysfunction Physiological disturbances in normal sexual performance in either the male or the female. Sexual Physiology is a group of disorders that interfere with any stage of the male’s sexual response cycle and result in disruption of normal sexual function.
| Stage | Changes in females | Changes in males | Changes in both |
|---|---|---|---|
| Desire |
|
||
| Excitement/arousal |
|
|
|
| Orgasm | Vaginal and uterine contractions |
|
|
| Resolution | Women experience little or no refractory period. | Men have a refractory period lasting minutes to hours during which they cannot reexperience orgasm. |
|
Normal male sexual function is the result of interaction between multiple systems:
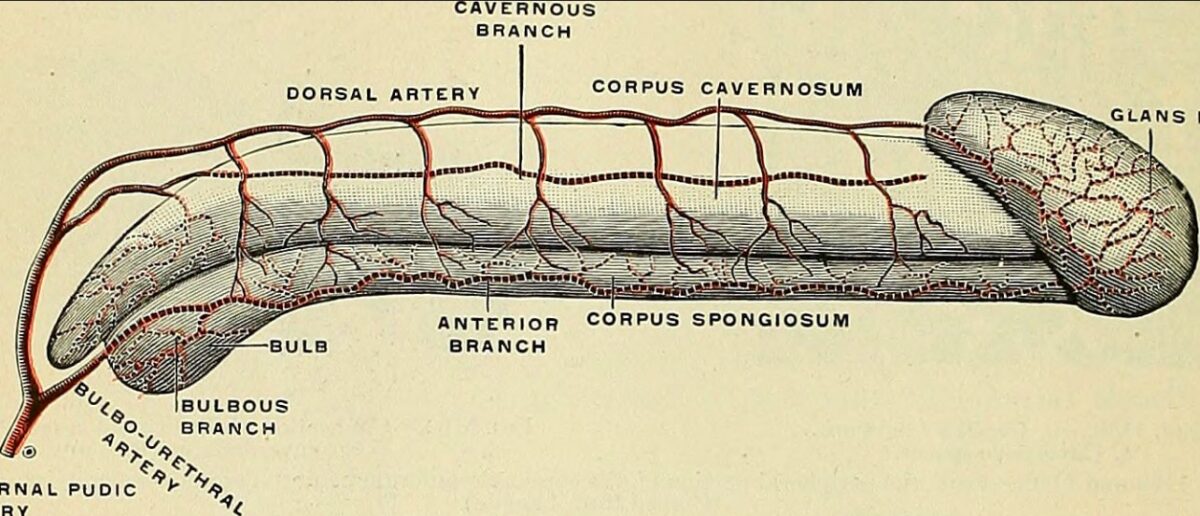
Penile vascular anatomy
Image: “Anatomy, descriptive and applied” by Henry Gray. License: Public DomainAutonomic innervation of male sexual response:
Neural pathways for different types of erections:
| Medications |
|
|---|---|
| Chronic medical conditions |
|
| Neurologic conditions |
|
| Psychogenic conditions (psychogenic ED) |
|
| Endocrine conditions |
|
| Exercise | Extensive bicycling and prolonged pressure on pudendal and cavernosal nerves increase the risk of ED. Regular Regular Insulin aerobic exercise not associated with nerve compression Nerve Compression Brachial Plexus Injuries decreases the risk of ED. |
| Penile conditions | Peyronie disease Peyronie Disease Penile Anomalies and Conditions |
| Medications | Mechanism of action | Side effects |
|---|---|---|
|
PDE5 inhibitors → increase intracavernosal cGMP cGMP Guanosine cyclic 3. Phosphodiesterase Inhibitors → increase intracavernosal NO |
|
| Alprostadil Alprostadil Coarctation of the Aorta | PGE1 agonist → increase cAMP cAMP An adenine nucleotide containing one phosphate group which is esterified to both the 3′- and 5′-positions of the sugar moiety. It is a second messenger and a key intracellular regulator, functioning as a mediator of activity for a number of hormones, including epinephrine, glucagon, and acth. Phosphodiesterase Inhibitors, decrease Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts)2+ → smooth muscle relaxation |
|

A modern penis pump utilizing a gaiter system in conjunction with water as a penis enlarger or penile rigidity device
Image: “A modern penis pump” by Arctic Sea Limited. License: CC BY 4.0