Primary amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System is defined as the absence of menstruation Menstruation The periodic shedding of the endometrium and associated menstrual bleeding in the menstrual cycle of humans and primates. Menstruation is due to the decline in circulating progesterone, and occurs at the late luteal phase when luteolysis of the corpus luteum takes place. Menstrual Cycle in a girl by age 15 years in the presence of normal secondary sex characteristics Secondary sex characteristics Gonadal Hormones. Etiologies can originate in the hypothalamic– pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types–ovarian (HPO) axis or from anatomic abnormalities in the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy or vagina Vagina The vagina is the female genital canal, extending from the vulva externally to the cervix uteri internally. The structures have sexual, reproductive, and urinary functions and a rich blood supply, mainly arising from the internal iliac artery. Vagina, Vulva, and Pelvic Floor: Anatomy. Sometimes other endocrinopathies interfere with the sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types enough to suppress menstruation Menstruation The periodic shedding of the endometrium and associated menstrual bleeding in the menstrual cycle of humans and primates. Menstruation is due to the decline in circulating progesterone, and occurs at the late luteal phase when luteolysis of the corpus luteum takes place. Menstrual Cycle. Important factors to assess when working through the differential diagnosis are whether the patient has breast development (indicating exposure to estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy from functional ovaries Ovaries Ovaries are the paired gonads of the female reproductive system that contain haploid gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis, just posterior to the broad ligament, and are connected to the pelvic sidewall and to the uterus by ligaments. These organs function to secrete hormones (estrogen and progesterone) and to produce the female germ cells (oocytes). Ovaries: Anatomy), the presence or absence of a uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy (indicating a potential genetic anomaly), and whether follicle-stimulating hormone ( FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle) levels are high, low, or normal (providing insight Insight Psychiatric Assessment into the HPO axis HPO axis Gonadal Hormones). Management includes correcting the underlying hormonal or anatomic issue, providing hormone replacement therapy Hormone Replacement Therapy Hormone replacement therapy (HRT) is used to treat symptoms associated with female menopause and in combination to suppress ovulation. Risks and side effects include uterine bleeding, predisposition to cancer, breast tenderness, hyperpigmentation, migraine headaches, hypertension, bloating, and mood changes. Noncontraceptive Estrogen and Progestins ( HRT HRT Hormone replacement therapy (HRT) is used to treat symptoms associated with female menopause and in combination to suppress ovulation. Risks and side effects include uterine bleeding, predisposition to cancer, breast tenderness, hyperpigmentation, migraine headaches, hypertension, bloating, and mood changes. Noncontraceptive Estrogen and Progestins), addressing fertility implications, and psychotherapy Psychotherapy Psychotherapy is interpersonal treatment based on the understanding of psychological principles and mechanisms of mental disease. The treatment approach is often individualized, depending on the psychiatric condition(s) or circumstance. Psychotherapy.
Last updated: Aug 2, 2023
Primary amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System is defined as:
Hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types of the hypothalamic– pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types–ovarian (HPO) axis and all relevant anatomy must be present and functioning in order for a girl to get her first menses Menses The periodic shedding of the endometrium and associated menstrual bleeding in the menstrual cycle of humans and primates. Menstruation is due to the decline in circulating progesterone, and occurs at the late luteal phase when luteolysis of the corpus luteum takes place. Menstrual Cycle.
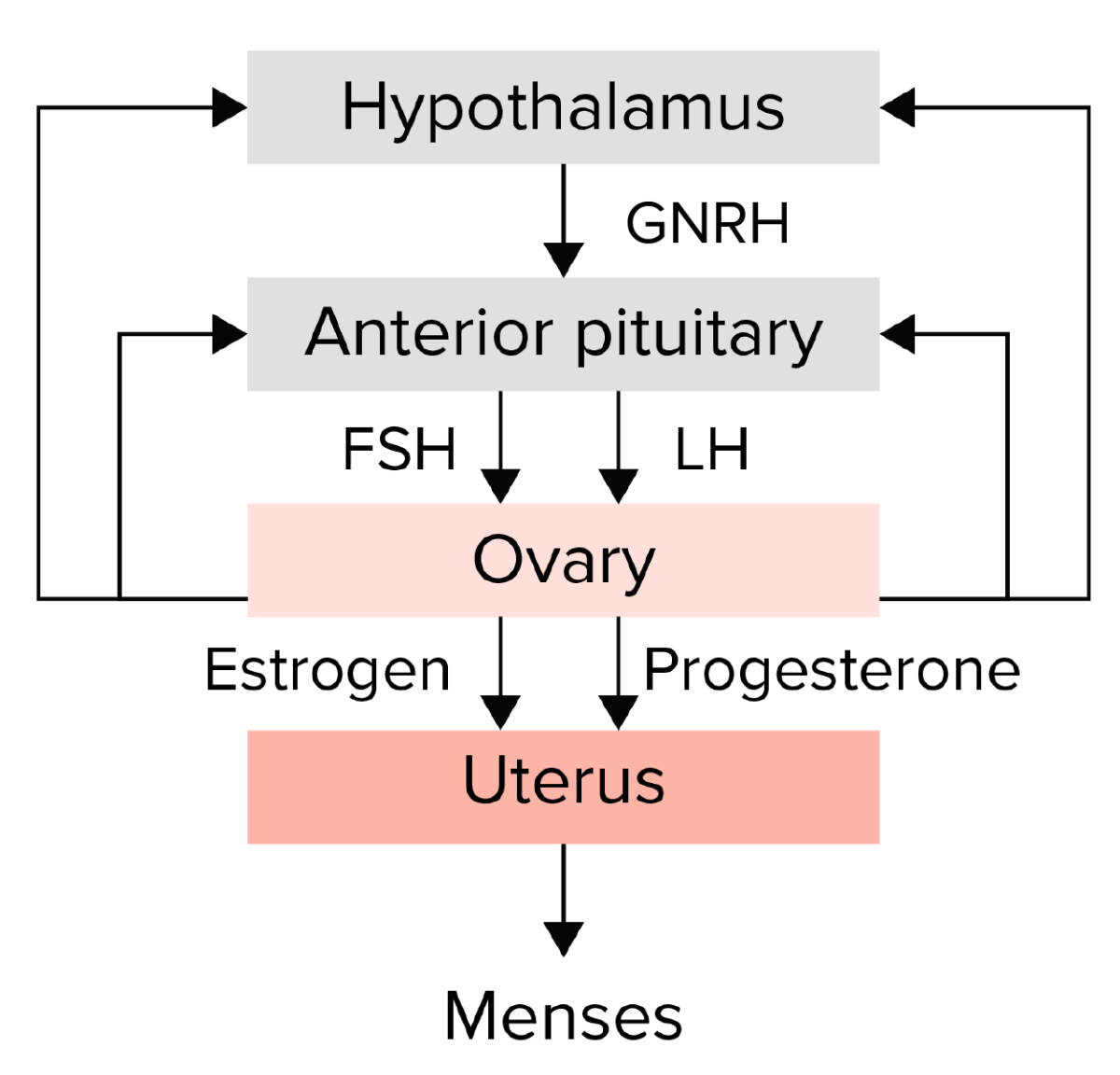
Summary of the hypothalamic–pituitary–ovarian axis:
The hypothalamus secretes gonadotropin-releasing hormone (GNRH), which stimulates the anterior pituitary to release the gonadotropins follicle-stimulating hormone (FSH) and luteinizing hormone (LH). The gonadotropins then stimulate the ovary to produce estrogen and progesterone, which in turn lead to endometrial growth and maturation. Any disruption in this pathway could lead to amenorrhea.
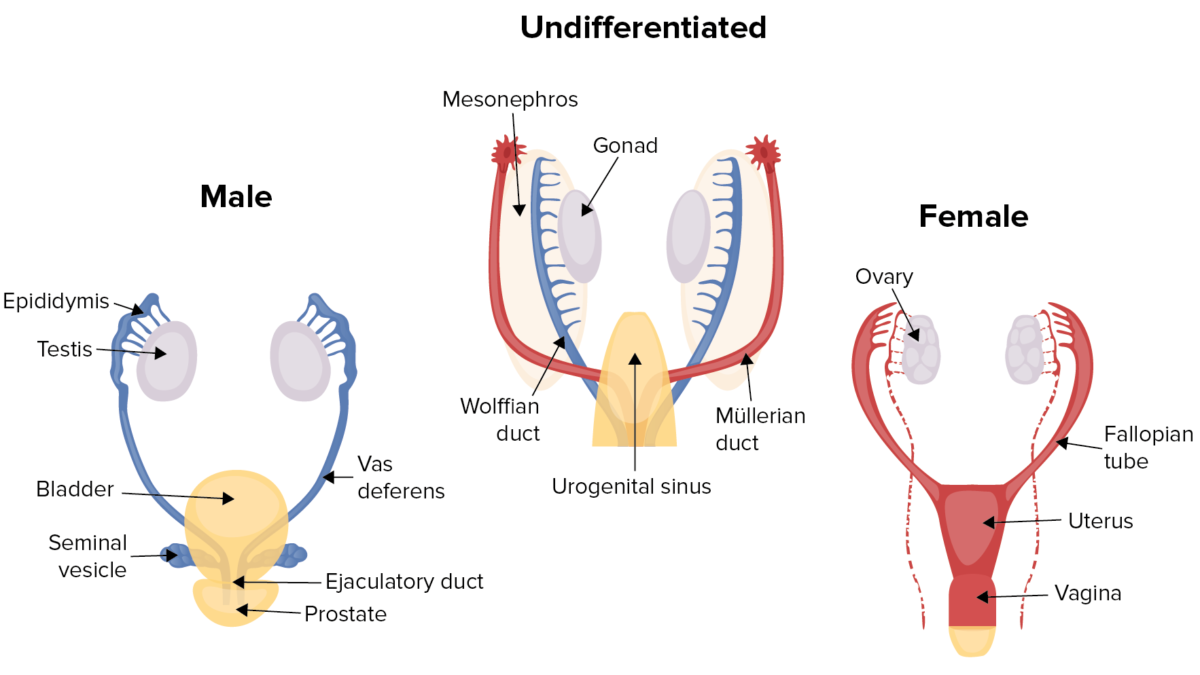
Human sex differentiation:
Males and female fetuses develop in an identical fashion for the first 6 weeks, developing both Wolffian (male) and Müllerian (female) ducts. The presence or absence of the SRY gene causes the gonads to develop into either testes or ovaries.
Start by assessing 4 things:
Management is dependent on the etiology and is usually aimed at correcting the underlying hormonal or anatomic issue.