Secondary amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System is defined as the absence of menses Menses The periodic shedding of the endometrium and associated menstrual bleeding in the menstrual cycle of humans and primates. Menstruation is due to the decline in circulating progesterone, and occurs at the late luteal phase when luteolysis of the corpus luteum takes place. Menstrual Cycle for 3 months in a woman with previously regular Regular Insulin menstrual cycles or for 6 months in a woman with previously irregular cycles. Etiologies involve either disruptions to the hypothalamic– pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types–ovarian (HPO) axis or acquired obstructions in the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy or outflow tract. The most common cause of secondary amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System is pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care. The most common pathologic etiologies include functional hypothalamic amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System, polycystic ovary syndrome, hyperprolactinemia Hyperprolactinemia Hyperprolactinemia is defined as a condition of elevated levels of prolactin (PRL) hormone in the blood. The PRL hormone is secreted by the anterior pituitary gland and is responsible for breast development and lactation. The most common cause is PRL-secreting pituitary adenomas (prolactinomas). Hyperprolactinemia, premature Premature Childbirth before 37 weeks of pregnancy (259 days from the first day of the mother's last menstrual period, or 245 days after fertilization). Necrotizing Enterocolitis ovarian insufficiency, and Asherman's syndrome. The diagnosis is made with a thorough history and physical examination, measurement of hormone levels, a pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care test, and imaging with pelvic ultrasonography. A progestin and/or combined estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy–progestin challenge can help further identify the location of the abnormality. Management depends on the underlying etiology, clinical presentation, and patient desires regarding fertility. Treatment can include lifestyle, medical, and surgical management options.
Last updated: Mar 16, 2023
Secondary amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System is defined as:
Hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types of the hypothalamic– pituitary Pituitary A small, unpaired gland situated in the sella turcica. It is connected to the hypothalamus by a short stalk which is called the infundibulum. Hormones: Overview and Types–ovarian (HPO) axis and all relevant anatomy must be present and functioning in order for menstruation Menstruation The periodic shedding of the endometrium and associated menstrual bleeding in the menstrual cycle of humans and primates. Menstruation is due to the decline in circulating progesterone, and occurs at the late luteal phase when luteolysis of the corpus luteum takes place. Menstrual Cycle to occur regularly.
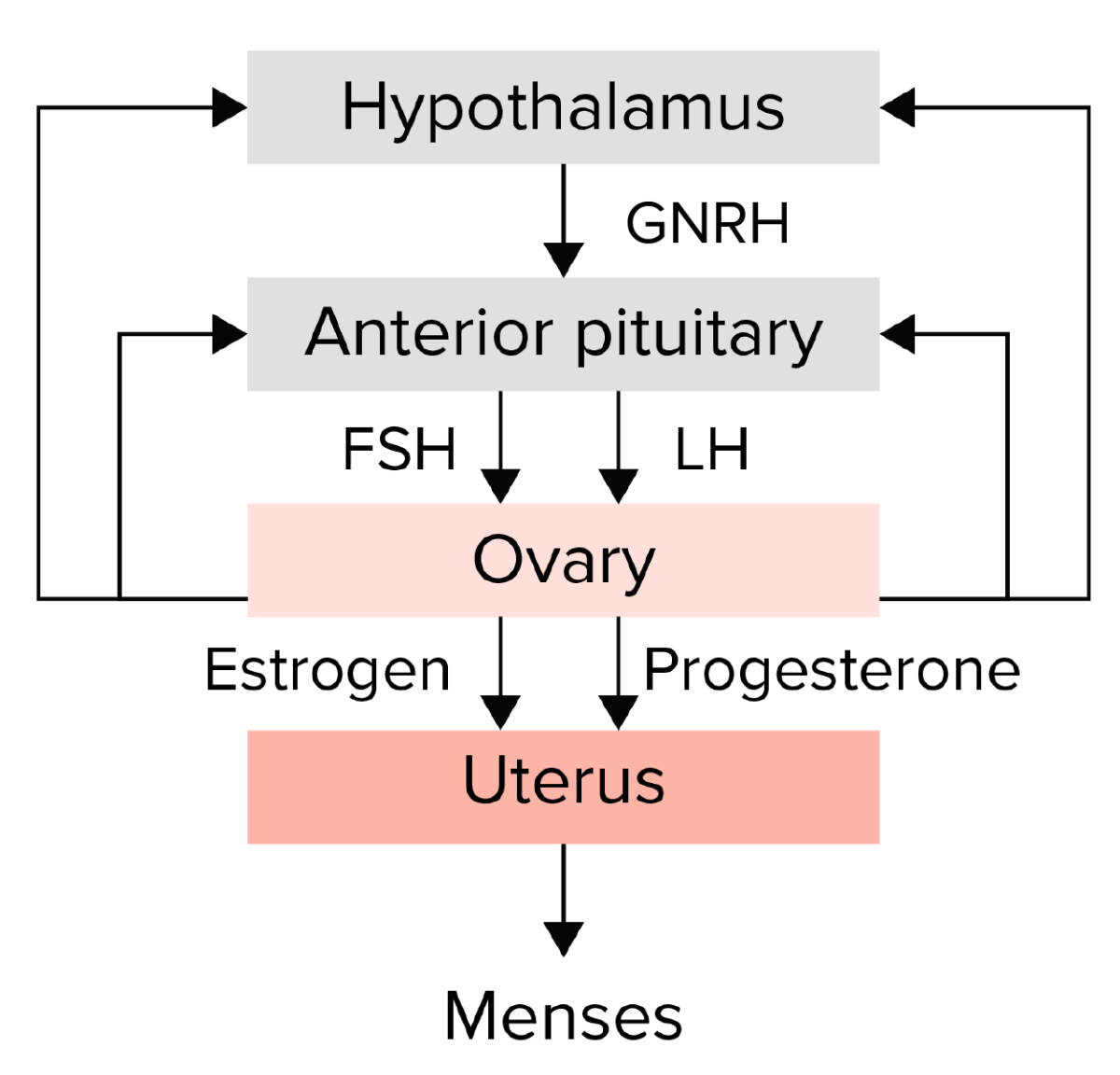
Summary of the hypothalamic–pituitary–ovarian axis:
The hypothalamus secretes gonadotropin-releasing hormone (GNRH), which stimulates the anterior pituitary to release the gonadotropins follicle-stimulating hormone (FSH) and luteinizing hormone (LH). The gonadotropins then stimulate the ovary to produce estrogen and progesterone, which in turn lead to endometrial growth and maturation. Any disruption in this pathway could lead to amenorrhea.
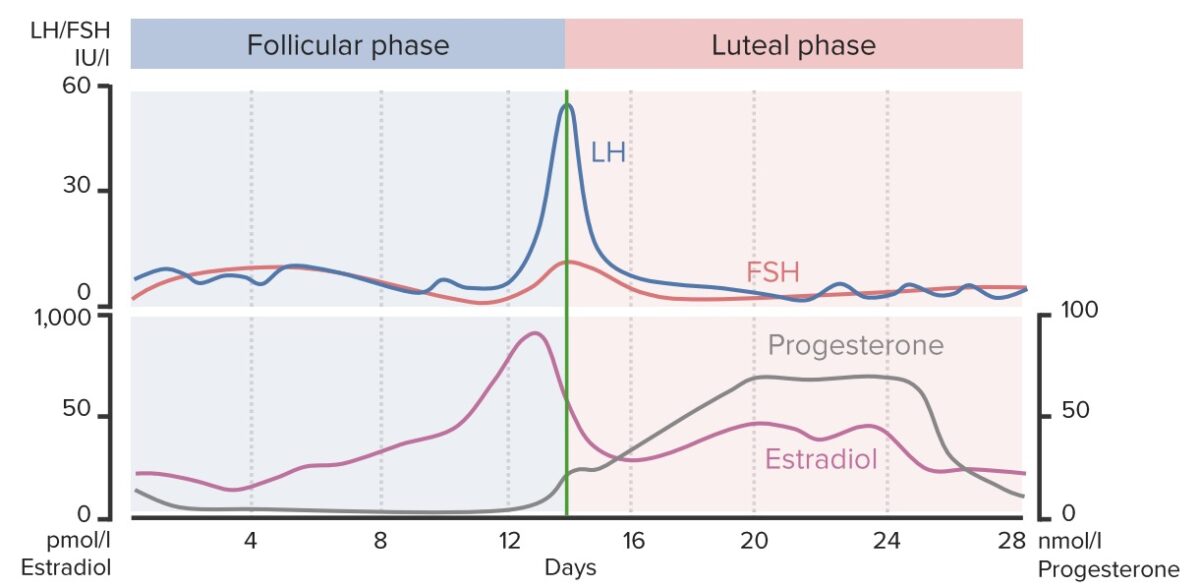
Hormone changes throughout the menstrual cycle:
This chart shows the changing concentrations of FSH, LH, estradiol, and progesterone throughout the length of the menstrual cycle. Notice the sudden rise in estradiol, LH, and FSH around day 14 (green line) during ovulation and the rise in progesterone during the luteal phase in anticipation of fertilization and implantation of the ovum. Disruptions in ovulation can lead to amenorrhea.
Pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care is the most common cause of secondary amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System. Always rule this out first!
| Cause of secondary amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System | Approximate frequency |
|---|---|
| Functional hypothalamic amenorrhea Amenorrhea Absence of menstruation. Congenital Malformations of the Female Reproductive System | 35% |
| PCOS PCOS Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder of reproductive-age women, affecting nearly 5%-10% of women in the age group. It is characterized by hyperandrogenism, chronic anovulation leading to oligomenorrhea (or amenorrhea), and metabolic dysfunction. Polycystic Ovarian Syndrome | 30% |
| Hyperprolactinemia Hyperprolactinemia Hyperprolactinemia is defined as a condition of elevated levels of prolactin (PRL) hormone in the blood. The PRL hormone is secreted by the anterior pituitary gland and is responsible for breast development and lactation. The most common cause is PRL-secreting pituitary adenomas (prolactinomas). Hyperprolactinemia | 13% |
| POI | 10% |
| Asherman’s syndrome | 5% |
| Other | 7% |
A woman of reproductive age with absence of menses Menses The periodic shedding of the endometrium and associated menstrual bleeding in the menstrual cycle of humans and primates. Menstruation is due to the decline in circulating progesterone, and occurs at the late luteal phase when luteolysis of the corpus luteum takes place. Menstrual Cycle for:
Clinical features depend on underlying etiology but may include:
Initial tests:
If signs of ↑ androgens Androgens Androgens are naturally occurring steroid hormones responsible for development and maintenance of the male sex characteristics, including penile, scrotal, and clitoral growth, development of sexual hair, deepening of the voice, and musculoskeletal growth. Androgens and Antiandrogens are present, but testosterone Testosterone A potent androgenic steroid and major product secreted by the leydig cells of the testis. Its production is stimulated by luteinizing hormone from the pituitary gland. In turn, testosterone exerts feedback control of the pituitary LH and FSH secretion. Depending on the tissues, testosterone can be further converted to dihydrotestosterone or estradiol. Androgens and Antiandrogens is normal:
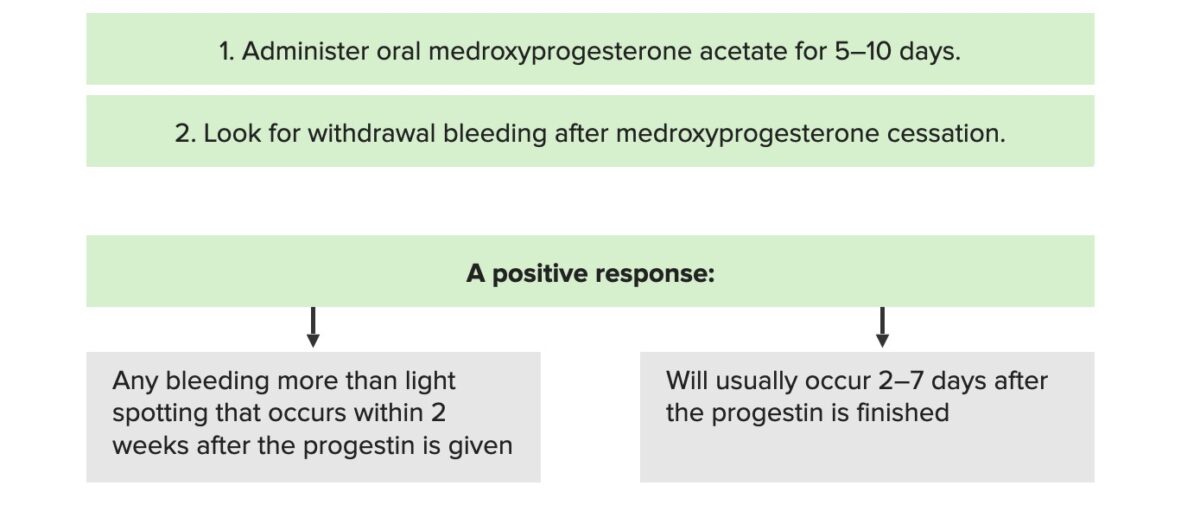
Progesterone challenge test
Image by Lecturio.Management depends on the etiology.
Treat other medical conditions:
Lifestyle management:
Medical management:
Surgical management:
Fertility treatment, if desired: