Pelvic inflammatory disease (PID) is defined as a polymicrobial infection of the upper female reproductive system. The disease can affect the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy, fallopian tubes Fallopian tubes The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The fallopian tubes receive an ovum after ovulation and help move it and/or a fertilized embryo toward the uterus via ciliated cells lining the tubes and peristaltic movements of its smooth muscle. Uterus, Cervix, and Fallopian Tubes: Anatomy, ovaries Ovaries Ovaries are the paired gonads of the female reproductive system that contain haploid gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis, just posterior to the broad ligament, and are connected to the pelvic sidewall and to the uterus by ligaments. These organs function to secrete hormones (estrogen and progesterone) and to produce the female germ cells (oocytes). Ovaries: Anatomy, and adjacent structures. Pelvic inflammatory disease is closely linked with sexually transmitted diseases, most commonly caused by Chlamydia trachomatis Chlamydia trachomatis Type species of Chlamydia causing a variety of ocular and urogenital diseases. Chlamydia and Neisseria gonorrhoeae Neisseria gonorrhoeae A species of gram-negative, aerobic bacteria primarily found in purulent venereal discharges. It is the causative agent of gonorrhea. Neisseria, as well as organisms associated with bacterial vaginosis Bacterial vaginosis Polymicrobial, nonspecific vaginitis associated with positive cultures of gardnerella vaginalis and other anaerobic organisms and a decrease in lactobacilli. It remains unclear whether the initial pathogenic event is caused by the growth of anaerobes or a primary decrease in lactobacilli. Vulvovaginitis, such as Gardnerella vaginalis Gardnerella vaginalis Polymicrobial, nonspecific vaginitis associated with positive cultures of gardnerella vaginalis and other anaerobic organisms and a decrease in lactobacilli. It remains unclear whether the initial pathogenic event is caused by the growth of anaerobes or a primary decrease in lactobacilli. Vulvovaginitis. Common symptoms are lower abdominal pain Abdominal Pain Acute Abdomen, cervical discharge, and irregular vaginal bleeding. Complications of PID can include ectopic pregnancy Ectopic pregnancy Ectopic pregnancy refers to the implantation of a fertilized egg (embryo) outside the uterine cavity. The main cause is disruption of the normal anatomy of the fallopian tube. Ectopic Pregnancy, chronic pelvic pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, and infertility Infertility Infertility is the inability to conceive in the context of regular intercourse. The most common causes of infertility in women are related to ovulatory dysfunction or tubal obstruction, whereas, in men, abnormal sperm is a common cause. Infertility. Diagnosis is primarily clinical in addition to PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) testing of cervical specimens and sometimes imaging or laparoscopy Laparoscopy Laparoscopy is surgical exploration and interventions performed through small incisions with a camera and long instruments. Laparotomy and Laparoscopy. Due to its polymicrobial nature, PID treatment is with combination antibiotic regimens.
Last updated: May 16, 2024
Pelvic inflammatory disease (PID) is an acute upper genital tract infection in women that affects the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy, oviducts, ovaries Ovaries Ovaries are the paired gonads of the female reproductive system that contain haploid gametes known as oocytes. The ovaries are located intraperitoneally in the pelvis, just posterior to the broad ligament, and are connected to the pelvic sidewall and to the uterus by ligaments. These organs function to secrete hormones (estrogen and progesterone) and to produce the female germ cells (oocytes). Ovaries: Anatomy, and possibly the adjacent pelvic organs.
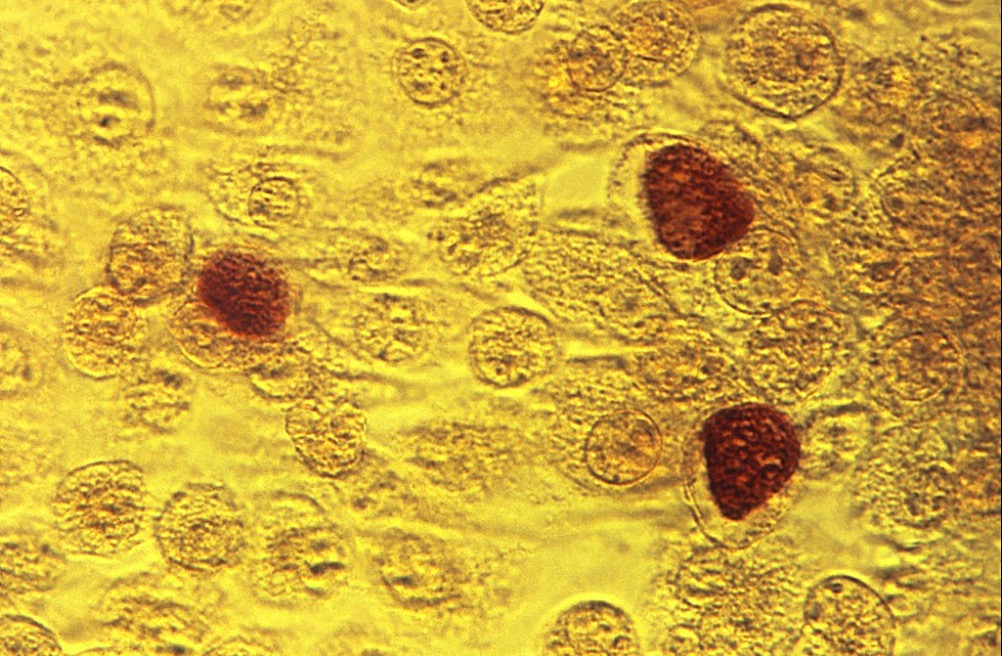
Photomicrograph showcasing McCoy cell monolayers with Chlamydia trachomatis inclusion bodies
Image: “Chlamydia trachomatis inclusion bodies” by CDC/Dr. E. Arum. License: Public Domain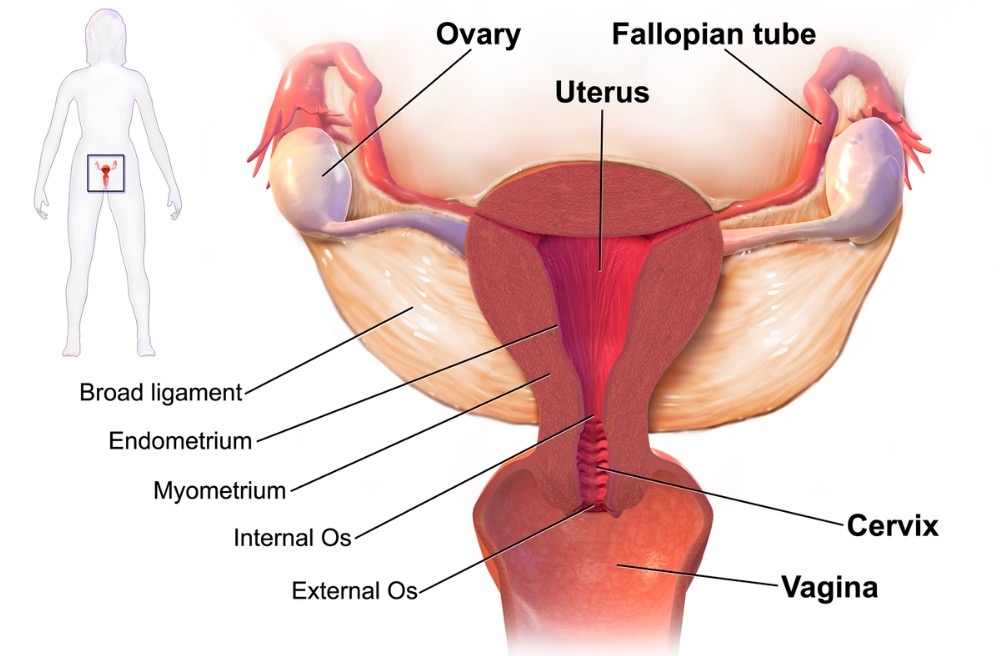
Sites of infection in PID: cervix, endometrium/uterus, ovary, and fallopian tubes
Image: “PID-Sites” by BruceBlaus. License: Public DomainDiagnosis is primarily clinical with a high index of suspicion.
Laboratory tests:
Imaging:
Laparoscopic exploration:
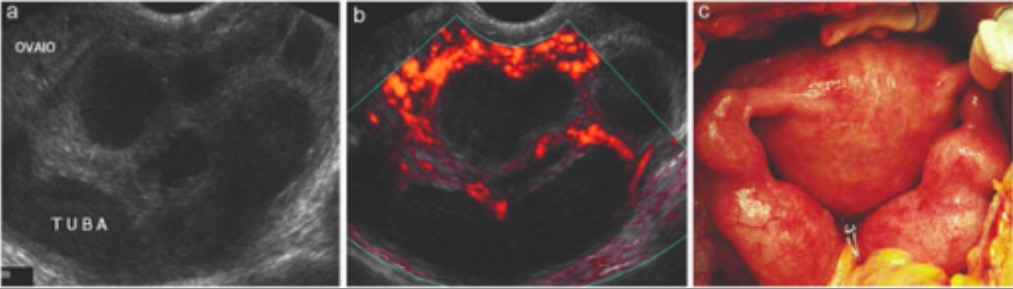
Pelvic inflammatory disease: grayscale ultrasound (A) and color Doppler (B) showing increased vascularity in the uterus (consistent with PID). Laparoscopy (C) confirms PID (uterine and adnexal swelling).
Image: “Pelvic inflammatory disease” by Department of Medical, Surgical and Neuro Sciences, Section of Radiological Sciences, Siena, Italy. License: CC BY 2.0