Appendectomy is an invasive surgical procedure performed with the goal of resecting and extracting the vermiform appendix Appendix A worm-like blind tube extension from the cecum. Colon, Cecum, and Appendix: Anatomy through either an open or a laparoscopic approach. The most common indication is acute appendicitis Appendicitis Appendicitis is the acute inflammation of the vermiform appendix and the most common abdominal surgical emergency globally. The condition has a lifetime risk of 8%. Characteristic features include periumbilical abdominal pain that migrates to the right lower quadrant, fever, anorexia, nausea, and vomiting. Appendicitis, which is why appendectomies are usually carried out in an urgent fashion. It is one of the most commonly performed emergent abdominal procedures. It can be associated with a number of postoperative complications Postoperative Complications Pathologic processes that affect patients after a surgical procedure. They may or may not be related to the disease for which the surgery was done, and they may or may not be direct results of the surgery. Postoperative Care; however, the majority of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship do very well and recover quickly.
Last updated: Jun 18, 2025
Appendectomy refers to surgical removal of the vermiform appendix Appendix A worm-like blind tube extension from the cecum. Colon, Cecum, and Appendix: Anatomy.
A review of the development of the abdominal organs Development of the Abdominal organs The abdominal organs are derived primarily from endoderm, which forms the primitive gut tube. The gut tube is divided into 3 regions: foregut, midgut, and hindgut. Development of the Abdominal Organs is important in order to understand the location of the appendix Appendix A worm-like blind tube extension from the cecum. Colon, Cecum, and Appendix: Anatomy within the abdominal cavity and its possible variants.
A review of the anatomy of the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy is important in order to more easily locate and recognize the cecum Cecum The blind sac or outpouching area of the large intestine that is below the entrance of the small intestine. It has a worm-like extension, the vermiform appendix. Colon, Cecum, and Appendix: Anatomy and appendix Appendix A worm-like blind tube extension from the cecum. Colon, Cecum, and Appendix: Anatomy within the abdominal cavity during surgery.
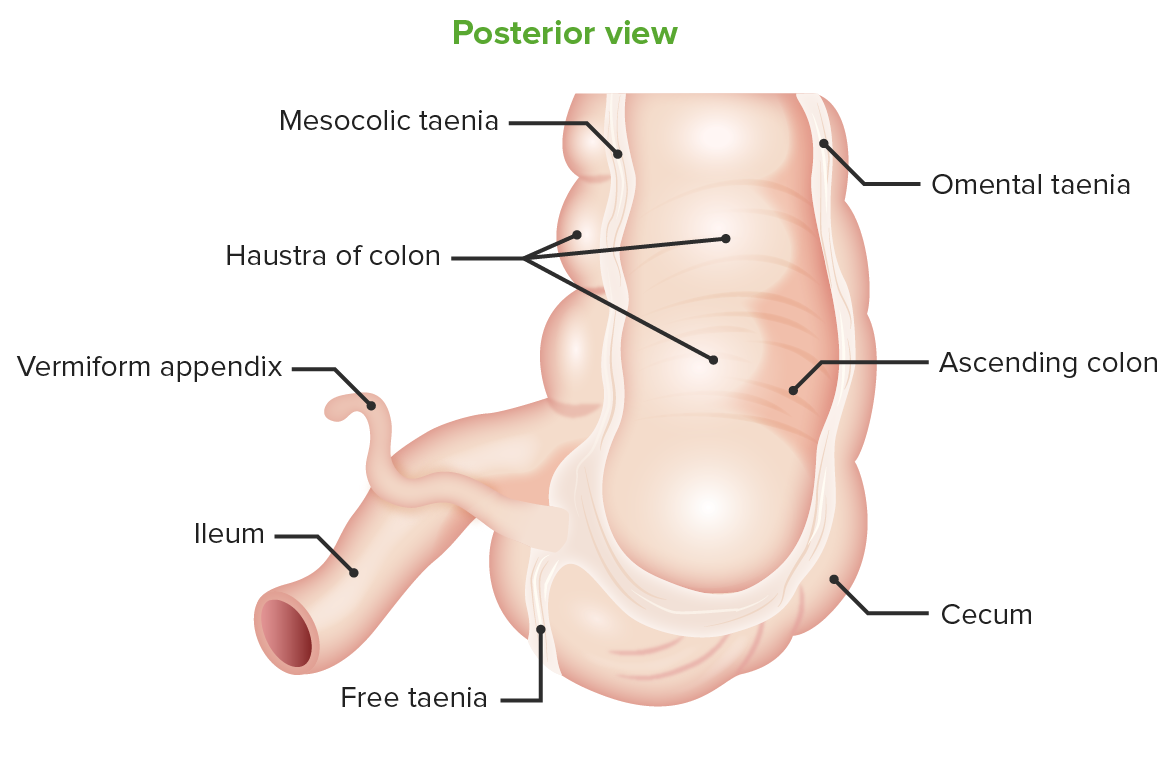
Posterior view of the cecum:
Location of the vermiform appendix at the taenia confluence
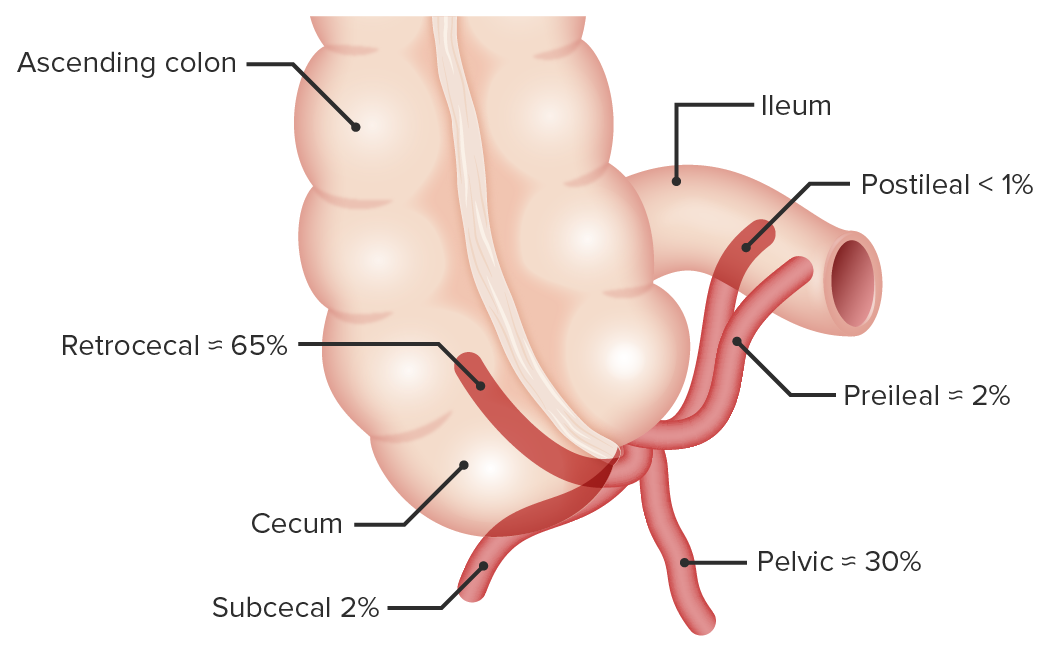
Location variants of the vermiform appendix
Image by Lecturio. License: CC BY-NC-SA 4.0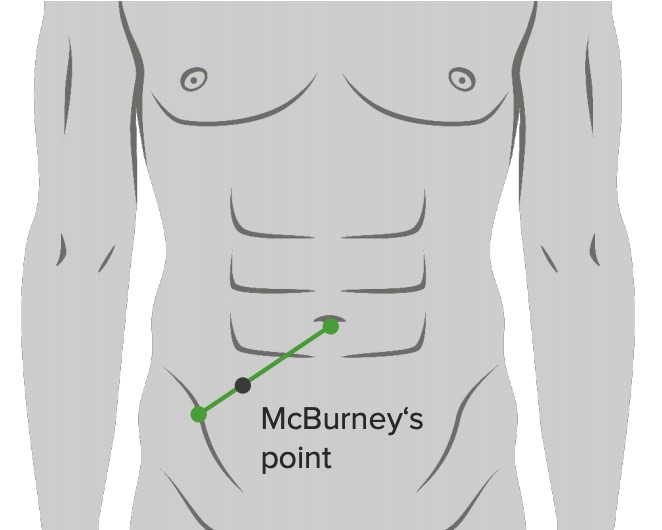
Location of McBurney’s point: ⅔ from umbilicus on a straight line from the umbilicus to anterior superior iliac spine
Image by Lecturio. License: CC BY-NC-SA 4.0Both open and laparoscopic approaches are considered acceptable. The choice should be made on the basis of the surgeon’s expertise and the patient’s preference. Laparoscopic appendectomies are associated with slightly shorter hospital stays and better pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways scores.
Open appendectomy:
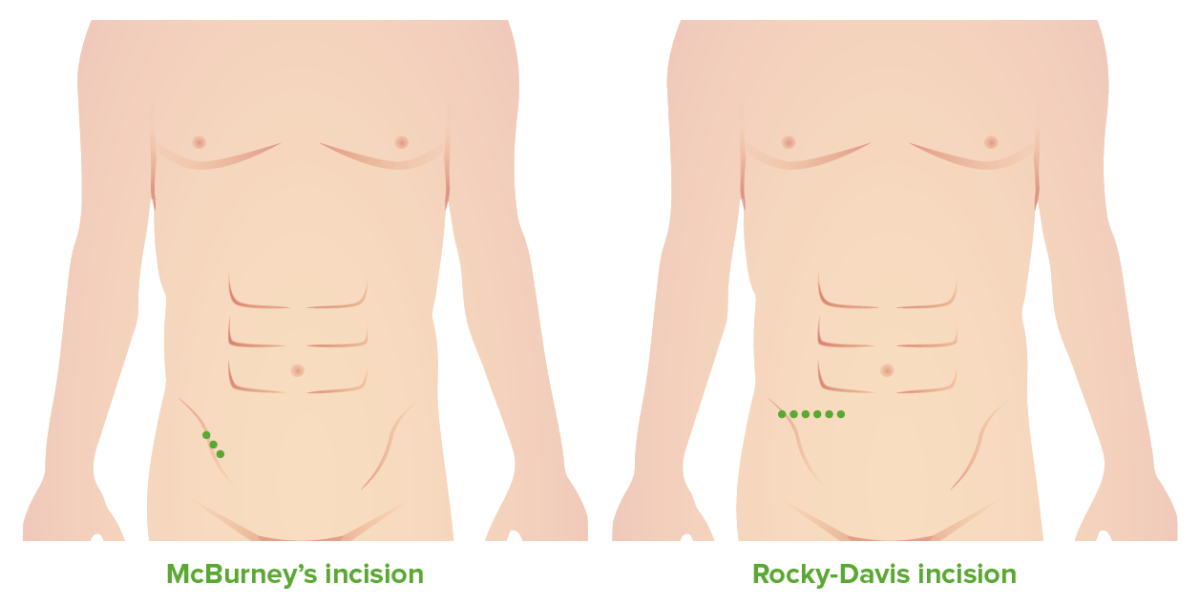
McBurney’s and Rocky–Davis incisions
Image by Lecturio. License: CC BY-NC-SA 4.0Laparoscopic appendectomy:
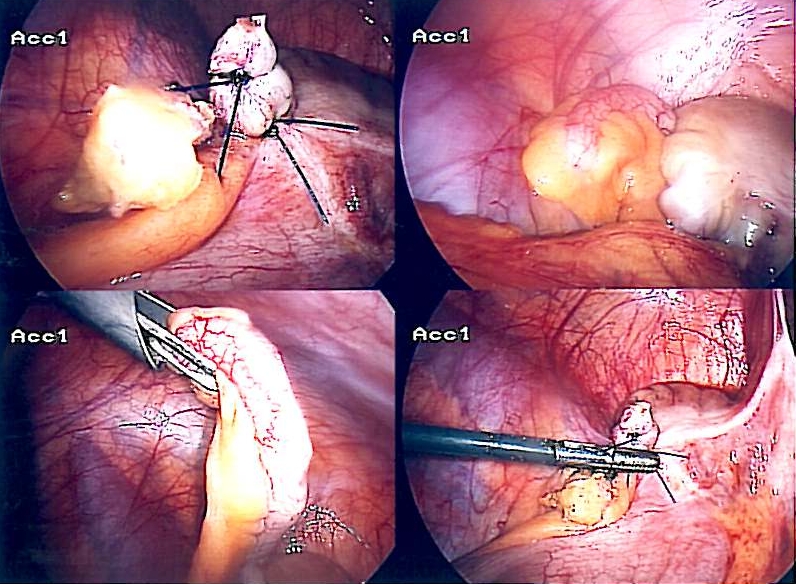
Laparoscopic appendectomy
Image: “Appendix-Entfernung” by Life-of-hannes.de. License: Public DomainPeritoneal lavage or “toilet”:
Exploratory laparotomy Exploratory Laparotomy Laparotomy and Laparoscopy:
Pregnant women: