The term vulvovaginitis is used to describe an acute inflammation Acute Inflammation Inflammation of the vulva Vulva The vulva is the external genitalia of the female and includes the mons pubis, labia majora, labia minora, clitoris, vestibule, vestibular bulb, and greater vestibular glands. Vagina, Vulva, and Pelvic Floor: Anatomy and vagina Vagina The vagina is the female genital canal, extending from the vulva externally to the cervix uteri internally. The structures have sexual, reproductive, and urinary functions and a rich blood supply, mainly arising from the internal iliac artery. Vagina, Vulva, and Pelvic Floor: Anatomy. Vulvovaginitis can be caused by several infectious and non-infectious etiologies, and results from disruption of the normal vaginal environment. Common signs and symptoms include pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, pruritis, erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion, and edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema of the affected region, as well as vaginal discharge and dyspareunia Dyspareunia Recurrent genital pain occurring during, before, or after sexual intercourse in either the male or the female. Primary Ovarian Insufficiency. The diagnosis is based on the clinical presentation, physical examination findings, and inspection Inspection Dermatologic Examination of vaginal secretions. Management depends on the etiology, including antimicrobials for infectious causes.
Last updated: Jul 5, 2023
Bacterial vaginosis (BV, may also be referred to as Gardnerella Gardnerella A genus of bacteria found in the human genital and urinary tract. It is considered to be a major cause of bacterial vaginosis. Nitroimidazoles vaginalis) is one of the most common causes of vulvovaginitis.
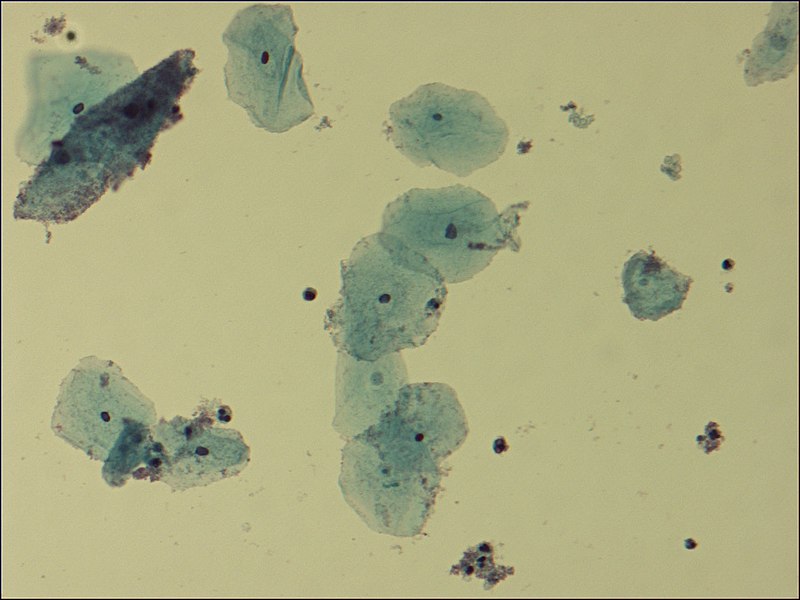
Microscopic view of clue cells in BV:
Tiny bacteria adhere to the periphery of the epithelial cells (the darker cell in the upper-left corner).
Pap smear showing clue cells, indicating BV
Image: “Pap smear” by the Department of Pathology, Muhimbili University of Health and Allied Sciences (MUHAS), P,O, Box 65001, Dar es Salaam, Tanzania. License: CC BY 2.0.Bacterial vaginosis is associated with an increased risk of:
Candidal vaginitis is a fungal vaginitis caused by:

Speculum exam findings in candidal vulvovaginitis:
thick, cottage cheese-like vaginal discharge on a slightly erythematous vaginal wall
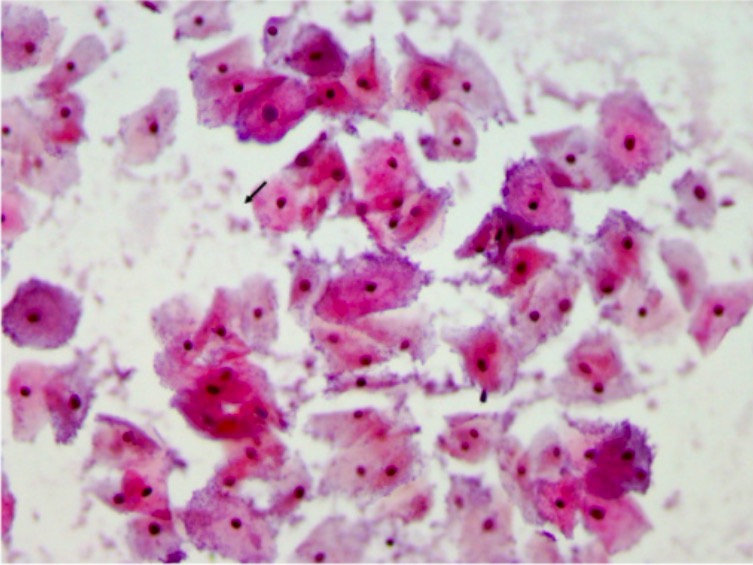
Wet mount demonstrating pseudohyphae of Candida albicans
Image: “Extra-leukocytic yeast and hyphal forms of candida” by Medanta The Medicity, Haematology, Gurgaon, India. License: CC BY 2.5Treatment options include oral or topical antifungals.
Trichomoniasis is the most common non-viral STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs).
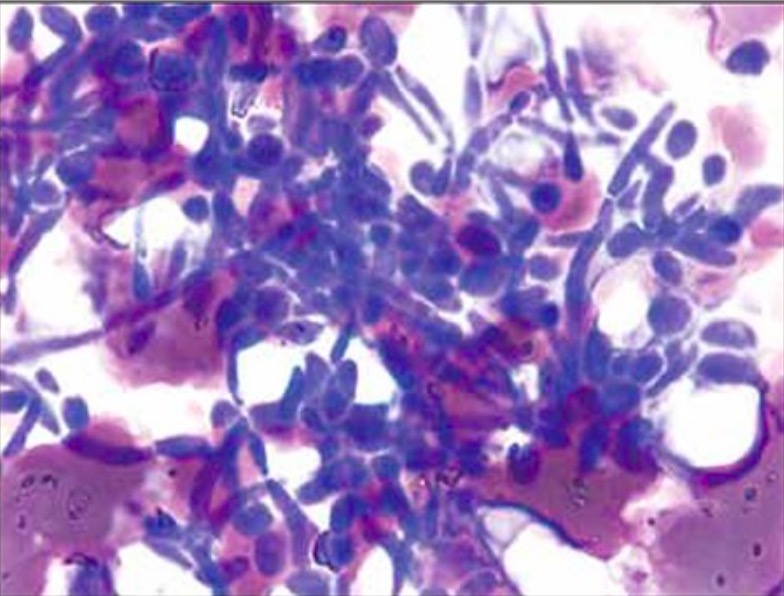
Microscopic images of Trichomonas vaginalis trophozoites
Image: “Trichomonas protozoa” by isis325. License: CC BY 2.0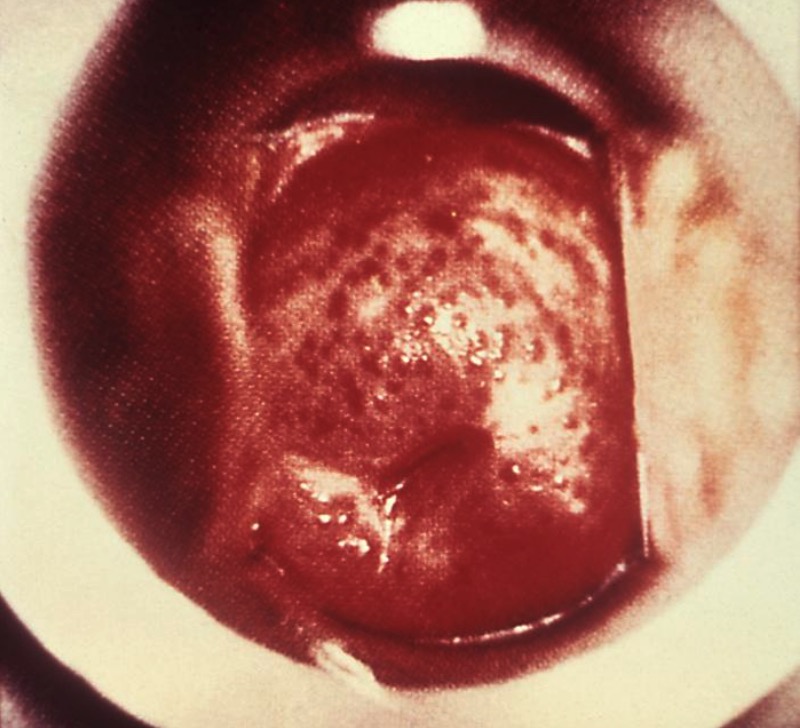
“Strawberry cervix” appearance seen in trichomoniasis
Image: “ 5240” by CDC. License: Public Domain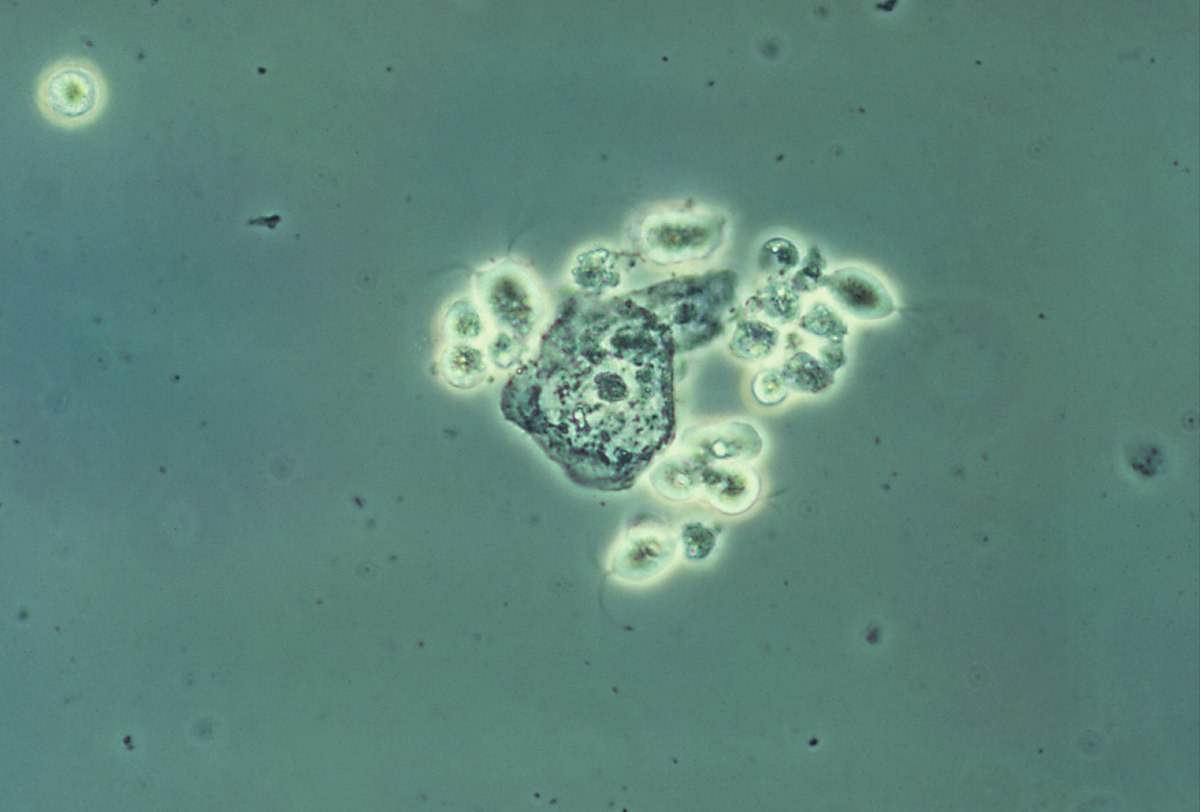
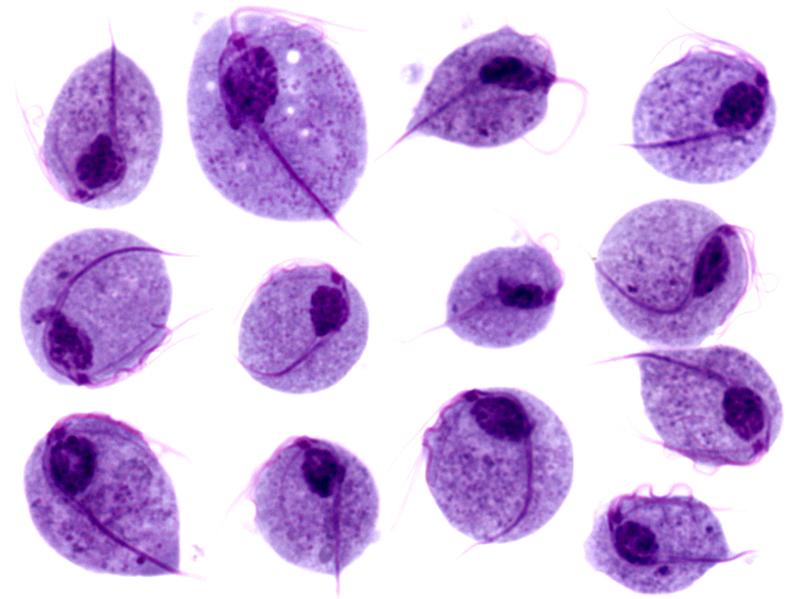
Wet mount image of vaginal secretions demonstrating several T. vaginalis protozoa (contrast-enhanced image)
Image: “Trichomonas vaginalis” by CDC. License: Public Domain
Physical exam findings in contact dermatitis:
This patient had an allergic reaction to hygiene products, resulting in red, edematous skin.