Herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology (HSV) is a double-stranded DNA DNA A deoxyribonucleotide polymer that is the primary genetic material of all cells. Eukaryotic and prokaryotic organisms normally contain DNA in a double-stranded state, yet several important biological processes transiently involve single-stranded regions. DNA, which consists of a polysugar-phosphate backbone possessing projections of purines (adenine and guanine) and pyrimidines (thymine and cytosine), forms a double helix that is held together by hydrogen bonds between these purines and pyrimidines (adenine to thymine and guanine to cytosine). DNA Types and Structure virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology belonging to the family Herpesviridae. Herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology commonly causes recurrent infections Recurrent infections Common Variable Immunodeficiency (CVID) involving the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and mucosal surfaces, including the mouth, lips Lips The lips are the soft and movable most external parts of the oral cavity. The blood supply of the lips originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy, eyes, and genitals. Typical mucocutaneous infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are characterized by an acute localized appearance of clusters of small, painful vesicles Vesicles Female Genitourinary Examination on an erythematous base. Although overlap exists, HSV-1 is classically associated with oropharyngeal lesions, whereas HSV-2 is mostly responsible for genital herpes Genital Herpes Genital herpes infections are common sexually transmitted infections caused by herpes simplex virus (HSV) type 1 or 2. Primary infection often presents with systemic, prodromal symptoms followed by clusters of painful, fluid-filled vesicles on an erythematous base, dysuria, and painful lymphadenopathy. Labial and Genital Herpes, an STI STI Sexually transmitted infections (STIs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs). Systemic and severe infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease including encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis, meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis, and neonatal herpes may also occur. The diagnosis is made based on clinical presentation and history, which can be confirmed by the microscopic examination of a stained smear of a fresh vesicle Vesicle Primary Skin Lesions, nucleic amplification test using PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR), direct immunofluorescence, or serologic tests. The therapy for mucocutaneous lesions is usually symptomatic, but antiviral Antiviral Antivirals for Hepatitis B therapies involving acyclovir Acyclovir A guanosine analog that acts as an antimetabolite. Viruses are especially susceptible. Used especially against herpes. Herpes Zoster (Shingles), valacyclovir Valacyclovir A prodrug of acyclovir that is used in the treatment of herpes zoster and herpes simplex virus infection of the skin and mucous membranes, including genital herpes. Herpes Zoster (Shingles), or famciclovir Famciclovir An aminopurine derivative and prodrug of penciclovir which is a competitive inhibitor of herpes simplex 2 DNA polymerase. It is used to treat herpes simplex virus infection. Antivirals for Herpes Virus are useful if given early, and are always part of the therapy for serious systemic infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease.
Last updated: May 16, 2024
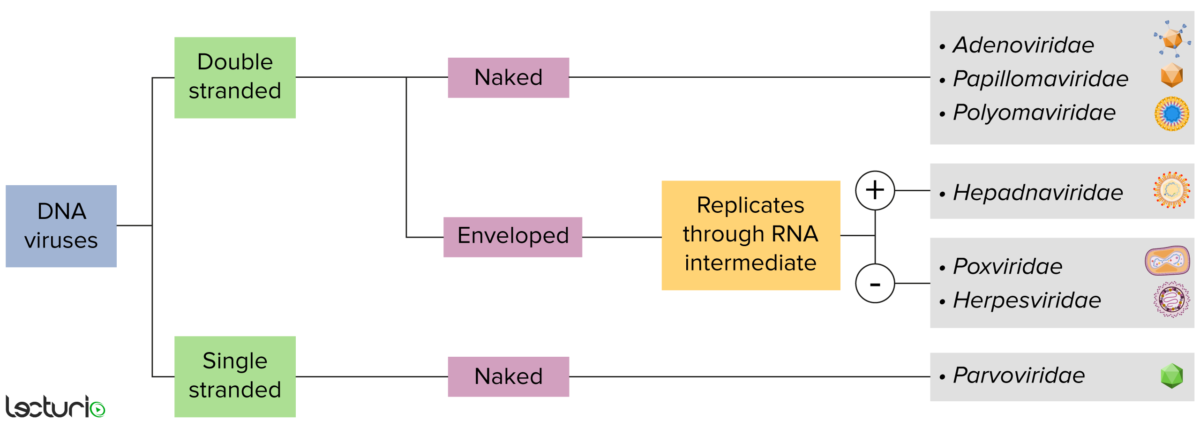
DNA virus identification:
Viruses can be classified in many ways. Most viruses, however, will either have a genome formed by DNA or RNA. Viruses with a DNA genome can be further characterized by whether that DNA is single or double stranded. If the viruses are covered by a thin coat of cell membrane (usually taken from the host cell), they are called “enveloped” viruses. If that coat is absent, the viruses are called “naked” viruses. Some of the enveloped viruses translate their DNA into RNA before it is incorporated into the host cell’s genome.
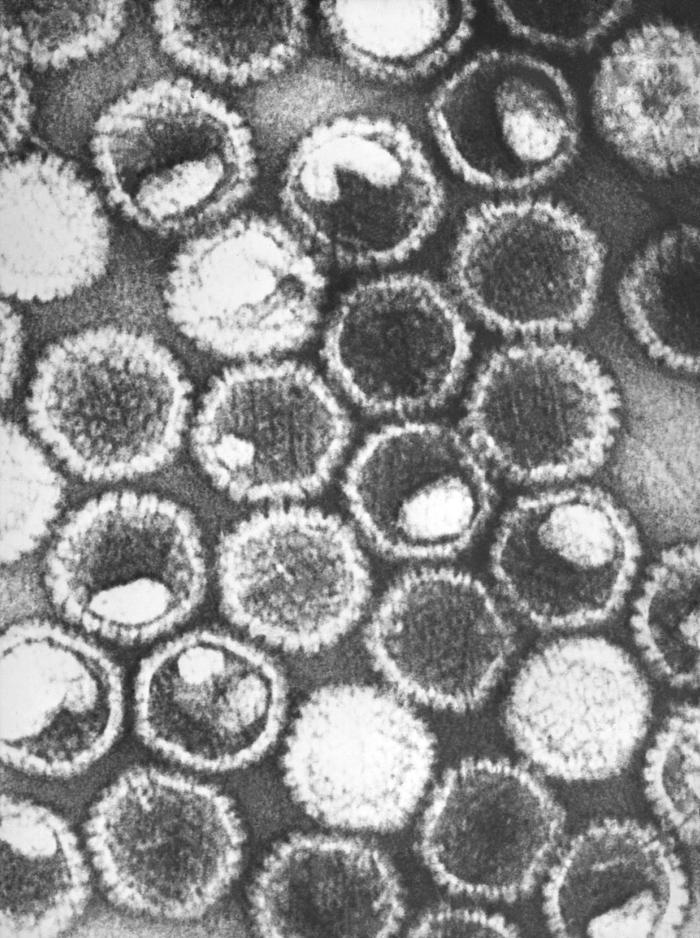
A negative-stained transmission electron micrograph showing numerous herpes simplex virions, members of the Herpesviridae virus family:
At the core of its icosahedral proteinaceous capsid, the herpes simplex virus contains a double-stranded DNA linear genome.
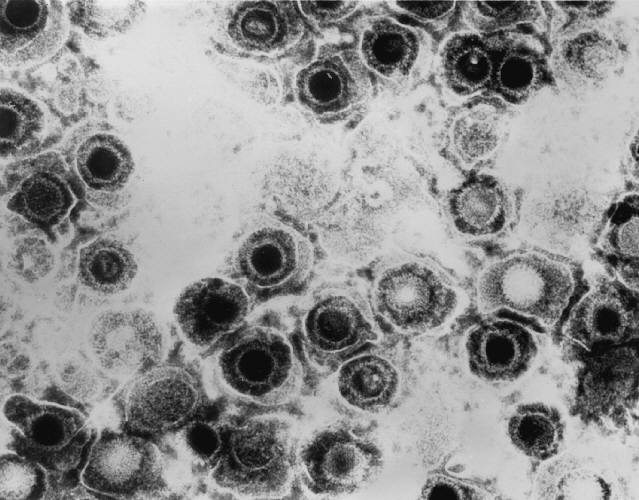
Transmission electron micrograph of herpes simplex virions
Image: “Transmission electron micrograph of herpes simplex virions” by CDC/Dr. Erskine Palmer. License: Public Domain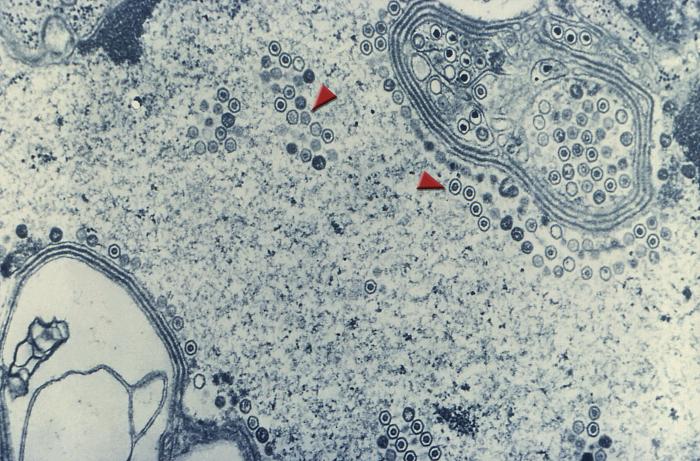
Transmission electron microscopic image demonstrating numerous, round herpes simplex virions inside the nucleus of a cell (arrows)
Image: “Transmission electron microscopic image demonstrating numerous, round herpes simplex virions inside the nucleus of a cell (arrows)” by CDC. License: Public DomainTwo types have been recognized to cause infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease:
HSV-1:
HSV-2:
Neonatal herpes infection:
Humans are the main reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli.
HSV-1:
HSV-2:
Primary infection:
Lifetime latency:
Reactivation:
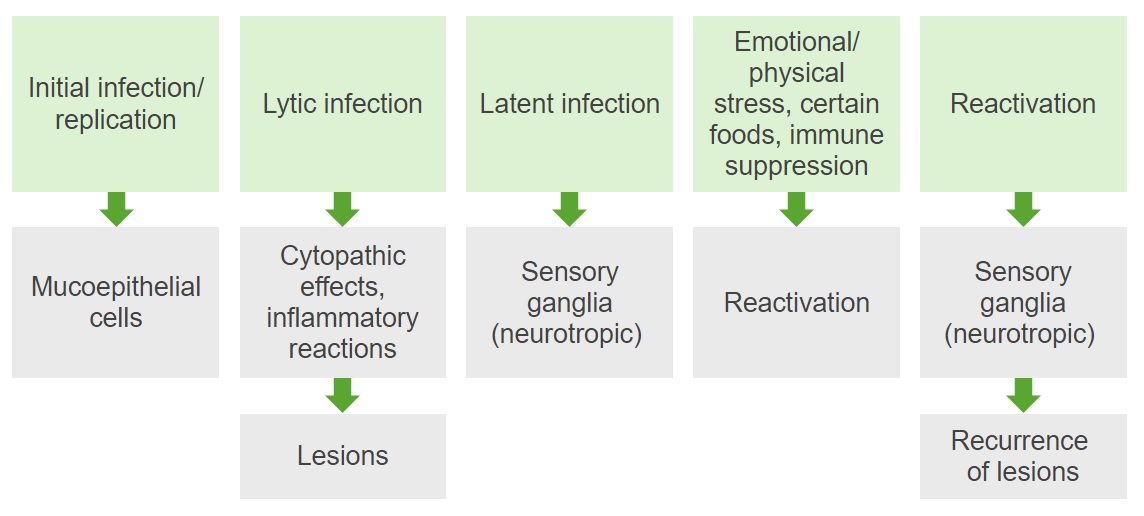
Diagram summarizing the pathogenesis of HSV-1 and -2 infections
Image by Lecturio. License: CC BY-NC-SA 4.0Herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections viruses Viruses Minute infectious agents whose genomes are composed of DNA or RNA, but not both. They are characterized by a lack of independent metabolism and the inability to replicate outside living host cells. Virology cause cytolytic infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease that form the basis of all pathologic changes: necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage of infected cells together with the inflammatory response
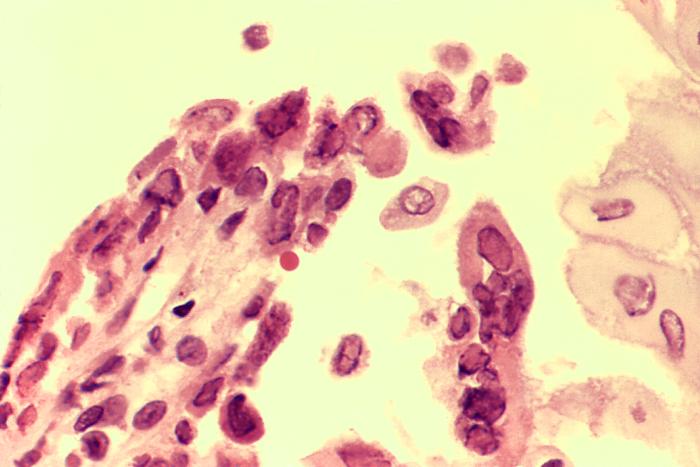
Biopsied esophageal ulcer caused by an active herpes simplex virus (HSV) infection in a patient with AIDS:
The specimen was harvested at the ulcerative border and reveals the presence of intranuclear inclusions, and cells with multiple nuclei
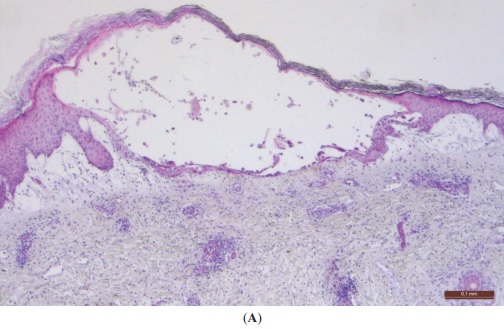
Low-power photomicrograph of a typical herpes virus vesicle:
The vesicle will fill with neutrophils (and change from a clear-fluid to a yellow, cloudy appearance) before it ruptures and leaves a superficial ulcer. Note how the viral cytopathic lesion stays within the epidermis, which explains why it heals without scarring, which can occur with severe dermal inflammation.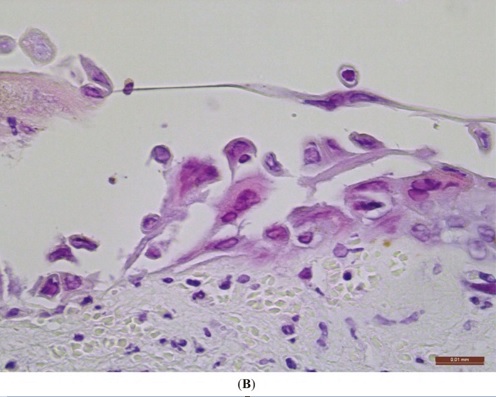
High-power photomicrograph of a herpes virus lesion in the skin:
Note the acantholysis (keratinocytes separated from each other), which is the basis of blister formation. Infected keratinocytes are enlarged and have glassy intranuclear inclusions (“Cowdry type A inclusions”). A few keratinocytes show multinucleation.
A number of conditions are caused by HSV. The infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease listed below are most commonly caused by HSV-1. Note: HSV-2 can also be (though often less commonly) associated with many of these diagnoses.
Only 20%‒25% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with HSV-1 antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions have a positive clinical history of oral-labial or genital infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease.
Gingivostomatitis:
Pharyngitis Pharyngitis Pharyngitis is an inflammation of the back of the throat (pharynx). Pharyngitis is usually caused by an upper respiratory tract infection, which is viral in most cases. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, and hoarseness. Pharyngitis:
Herpes labialis:

Lesions on the soft palate and tongue caused by the herpes simplex virus
Image: “This photograph depicts a close view of an elderly African American female patient’s oral cavity” by CDC/ Robert E. Sumpter. License: Public Domain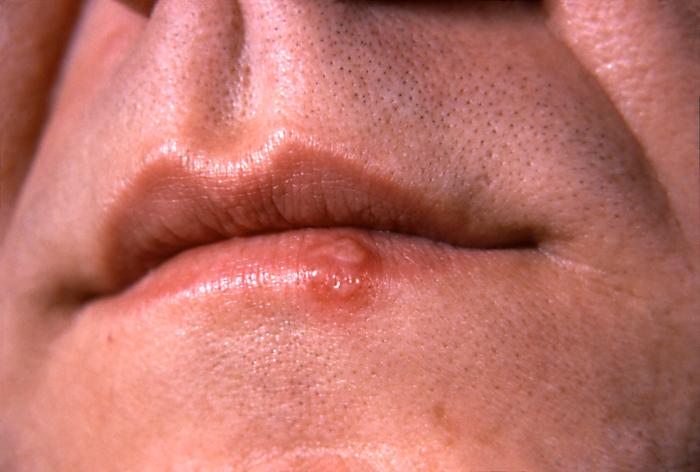
Herpes simplex lesion on the lower lip, at the vermilion border, on the 2nd day after onset
Image: “This photograph depicts a close-up of the lips of a patient with a herpes simplex lesion on the lower lip” by CDC/ Dr. Hermann. License: Public DomainHerpetic whitlow:
Herpes gladiatorum:
Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion multiforme:
Eczema Eczema Atopic dermatitis, also known as eczema, is a chronic, relapsing, pruritic, inflammatory skin disease that occurs more frequently in children, although adults can also be affected. The condition is often associated with elevated serum levels of IgE and a personal or family history of atopy. Skin dryness, erythema, oozing, crusting, and lichenification are present. Atopic Dermatitis (Eczema) herpeticum:

A patient with vesicles on the finger due to herpetic whitlow
Image: “Herpetic Whitlow” by Salford Royal Foundation Trust, Manchester, UK. License: CC BY 3.0
Diffuse vesicular lesions on the face of a patient suffering from eczema herpeticum while undergoing UV therapy
Image: “Multiple pustules on the face surface” by AUTHOR. License: CC BY 2.0Eye infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease occur in < 5% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with HSV-1 infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, leading to vision Vision Ophthalmic Exam loss and/or blindness Blindness The inability to see or the loss or absence of perception of visual stimuli. This condition may be the result of eye diseases; optic nerve diseases; optic chiasm diseases; or brain diseases affecting the visual pathways or occipital lobe. Retinopathy of Prematurity.
Keratitis:
Acute retinal necrosis Acute Retinal Necrosis Herpes Zoster (Shingles):
Conjunctivitis Conjunctivitis Conjunctivitis is a common inflammation of the bulbar and/or palpebral conjunctiva. It can be classified into infectious (mostly viral) and noninfectious conjunctivitis, which includes allergic causes. Patients commonly present with red eyes, increased tearing, burning, foreign body sensation, and photophobia. Conjunctivitis and blepharitis Blepharitis Blepharitis is an ocular condition characterized by eyelid inflammation. Anterior blepharitis involves the eyelid skin and eyelashes, while the posterior type affects the meibomian glands. Often, these conditions overlap. Blepharitis:
Chorioretinitis Chorioretinitis Chorioretinitis is the inflammation of the posterior segment of the eye, including the choroid and the retina. The condition is usually caused by infections, the most common of which is toxoplasmosis. Some of these infections can affect the fetus in utero and present as congenital abnormalities. Chorioretinitis ( posterior uveitis Posterior Uveitis Diseases of the Uvea):
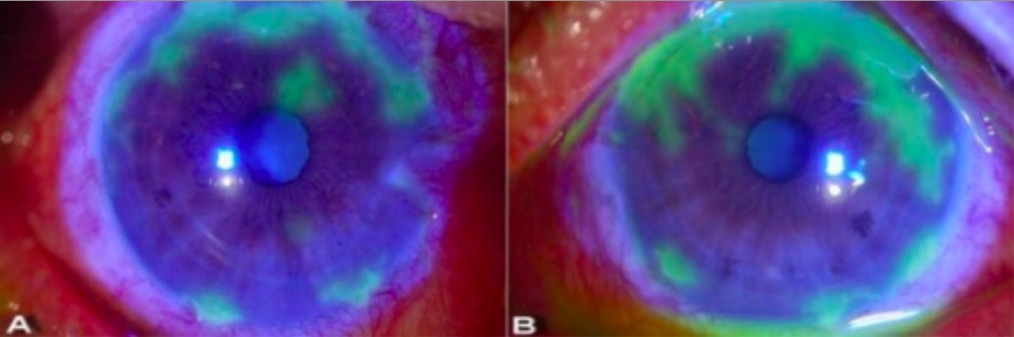
Slit-lamp examination showing dendritic lesions in herpetic keratitis:
Seen here as irregular geographic patterns of ulceration highlighted in green after the application of yellow-orange fluorescein dye. The dye is taken up by the damaged cornea (where the surface has been disrupted) and the area appears green under cobalt blue light.
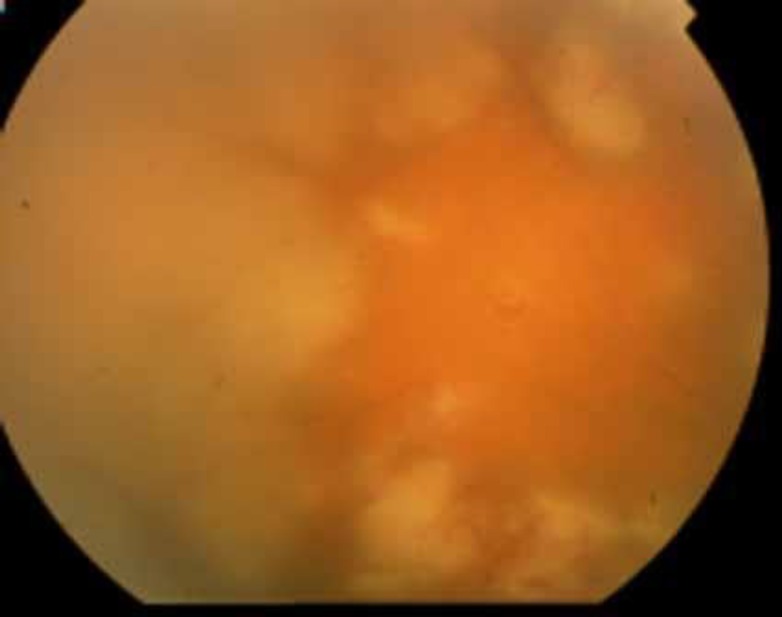
Fundoscopic image from a patient with acute retinal necrosis:
Characteristic confluent necrotic areas can be seen. Retinitis appears as deep, multifocal, yellow-white patches, typically beginning in the peripheral fundus and then becoming concentrically confluent and spreading toward the posterior pole.
Encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis:
Aseptic meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis:
Other manifestations:
Epiglottitis Epiglottitis Epiglottitis (or “supraglottitis”) is an inflammation of the epiglottis and adjacent supraglottic structures. The majority of cases are caused by bacterial infection. Symptoms are rapid in onset and severe. Epiglottitis or laryngitis Laryngitis Laryngitis is an inflammation of the larynx most commonly due to infection or trauma that can be either acute or chronic. In this condition, the 2 folds of mucous membranes that make up the vocal cords become inflamed and irritated. The inflammation results in a distortion of the voice produced, resulting in a hoarse sound or aphonia. Laryngitis (herpetic croup Croup Croup, also known as laryngotracheobronchitis, is a disease most commonly caused by a viral infection that leads to severe inflammation of the upper airway. It usually presents in children < 5 years of age. Patients develop a hoarse, "seal-like" barking cough and inspiratory stridor. Croup):
HSV pneumonitis Pneumonitis Human Herpesvirus 6 and 7:
HSV esophagitis Esophagitis Esophagitis is the inflammation or irritation of the esophagus. The major types of esophagitis are medication-induced, infectious, eosinophilic, corrosive, and acid reflux. Patients typically present with odynophagia, dysphagia, and retrosternal chest pain. Esophagitis:
Fulminant hepatitis Fulminant hepatitis Echovirus:
The conditions listed below are most commonly associated with HSV-2 infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. Again, keep in mind that HSV-1 can also be associated with many of these diagnoses.
Primary genital HSV-2 infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease:
Non-primary 1st episode infection (reactivation):

Penile blisters (arrows) due to a recurring herpes simplex-2 virus (HSV-2) infection
Image: “Penile blisters (arrows), due to a recurring herpes simplex-2 (HSV-2) virus infection” by CDC/ Susan Lindsley. License: Public Domain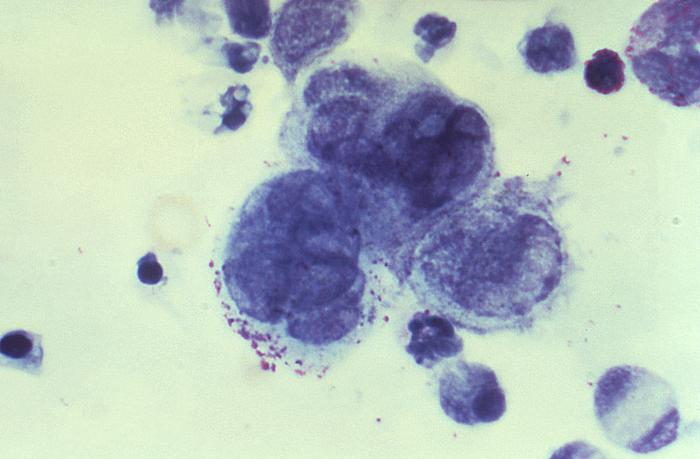
Image from a Tzanck smear obtained from a penile lesion:
Multinucleated giant cells are seen, indicating a herpes infection.
Antivirals:
Analgesics:
The table presented below compares and contrasts HSV-1 and HSV-2:
| Serotype | HSV-1 | HSV-2 |
|---|---|---|
| Transmission |
|
|
| Lytic infection | Mucoepithelial cells | Mucoepithelial cells |
| Latency | Trigeminal ganglia | Sacral ganglia |
| Diseases |
|
|
The table below compares the 9 herpesviruses considered endemic in humans. There are 115 different total known species of herpesviruses, which are grouped into 3 families:
| HHV | Common name | Primary target cells | Latency site | Clinical presentation* |
|---|---|---|---|---|
|
1 (alpha group) |
HSV-1 | Mucoepithelial cells | Dorsal root ganglia |
|
|
2 (alpha group) |
HSV-2 |
|
||
|
3 (alpha group) |
VZV |
|
||
|
4 (gamma group) |
EBV EBV Epstein-barr virus (EBV) is a linear, double-stranded DNA virus belonging to the herpesviridae family. This highly prevalent virus is mostly transmitted through contact with oropharyngeal secretions from an infected individual. The virus can infect epithelial cells and B lymphocytes, where it can undergo lytic replication or latency. Epstein-Barr Virus |
|
Memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment B cells B cells Lymphoid cells concerned with humoral immunity. They are short-lived cells resembling bursa-derived lymphocytes of birds in their production of immunoglobulin upon appropriate stimulation. B cells: Types and Functions |
|
|
5 (beta group) |
CMV |
|
Hematopoietic progenitor cells in bone marrow Bone marrow The soft tissue filling the cavities of bones. Bone marrow exists in two types, yellow and red. Yellow marrow is found in the large cavities of large bones and consists mostly of fat cells and a few primitive blood cells. Red marrow is a hematopoietic tissue and is the site of production of erythrocytes and granular leukocytes. Bone marrow is made up of a framework of connective tissue containing branching fibers with the frame being filled with marrow cells. Bone Marrow: Composition and Hematopoiesis |
|
|
6A, 6B (beta group) |
HHV-6 HHV-6 Human herpesvirus (HHV)-6 and HHV-7 are similar double-stranded DNA viruses belonging to the Herpesviridae family. Human herpesviruses are ubiquitous and infections are commonly contracted during childhood. Human Herpesvirus 6 and 7 | T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified – cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions | Monocytes Monocytes Large, phagocytic mononuclear leukocytes produced in the vertebrate bone marrow and released into the blood; contain a large, oval or somewhat indented nucleus surrounded by voluminous cytoplasm and numerous organelles. Innate Immunity: Phagocytes and Antigen Presentation | Roseola |
|
7 (beta group) |
HHV-7 HHV-7 Human herpesvirus (HHV)-6 and HHV-7 are similar double-stranded DNA viruses belonging to the Herpesviridae family. Human herpesviruses are ubiquitous and infections are commonly contracted during childhood. Human Herpesvirus 6 and 7 | T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified – cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions | ||
|
8 (gamma group) |
Kaposi Kaposi A multicentric, malignant neoplastic vascular proliferation characterized by the development of bluish-red cutaneous nodules, usually on the lower extremities, most often on the toes or feet, and slowly increasing in size and number and spreading to more proximal areas. The tumors have endothelium-lined channels and vascular spaces admixed with variably sized aggregates of spindle-shaped cells, and often remain confined to the skin and subcutaneous tissue, but widespread visceral involvement may occur. Hhv-8 is the suspected cause. There is also a high incidence in AIDS patients. AIDS-defining Conditions‘s sarcoma-associated herpesvirus |
|
B cells B cells Lymphoid cells concerned with humoral immunity. They are short-lived cells resembling bursa-derived lymphocytes of birds in their production of immunoglobulin upon appropriate stimulation. B cells: Types and Functions | Kaposi Kaposi A multicentric, malignant neoplastic vascular proliferation characterized by the development of bluish-red cutaneous nodules, usually on the lower extremities, most often on the toes or feet, and slowly increasing in size and number and spreading to more proximal areas. The tumors have endothelium-lined channels and vascular spaces admixed with variably sized aggregates of spindle-shaped cells, and often remain confined to the skin and subcutaneous tissue, but widespread visceral involvement may occur. Hhv-8 is the suspected cause. There is also a high incidence in AIDS patients. AIDS-defining Conditions sarcoma |