Mycoplasma is a species of pleomorphic Pleomorphic Bacteroides bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology that lack a cell wall Cell wall The outermost layer of a cell in most plants; bacteria; fungi; and algae. The cell wall is usually a rigid structure that lies external to the cell membrane, and provides a protective barrier against physical or chemical agents. Cell Types: Eukaryotic versus Prokaryotic, which makes them difficult to target with conventional antibiotics (particularly penicillins Penicillins Beta-lactam antibiotics contain a beta-lactam ring as a part of their chemical structure. Drugs in this class include penicillin G and V, penicillinase-sensitive and penicillinase-resistant penicillins, cephalosporins, carbapenems, and aztreonam. Penicillins and other beta-lactam Beta-Lactam Penicillins antibiotics that target cell wall Cell wall The outermost layer of a cell in most plants; bacteria; fungi; and algae. The cell wall is usually a rigid structure that lies external to the cell membrane, and provides a protective barrier against physical or chemical agents. Cell Types: Eukaryotic versus Prokaryotic synthesis Synthesis Polymerase Chain Reaction (PCR)) and causes them to not gram stain Gram stain Klebsiella well. Mycoplasma bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology commonly target the respiratory and urogenital epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology. Mycoplasma pneumoniae (M. pneumoniae), the causative agent of atypical or “walking” pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia, is the most clinically relevant species. Antibiotics, particularly macrolides Macrolides Macrolides and ketolides are antibiotics that inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit and blocking transpeptidation. These antibiotics have a broad spectrum of antimicrobial activity but are best known for their coverage of atypical microorganisms. Macrolides and Ketolides, are the most effective mode of therapy.
Last updated: Jan 15, 2025
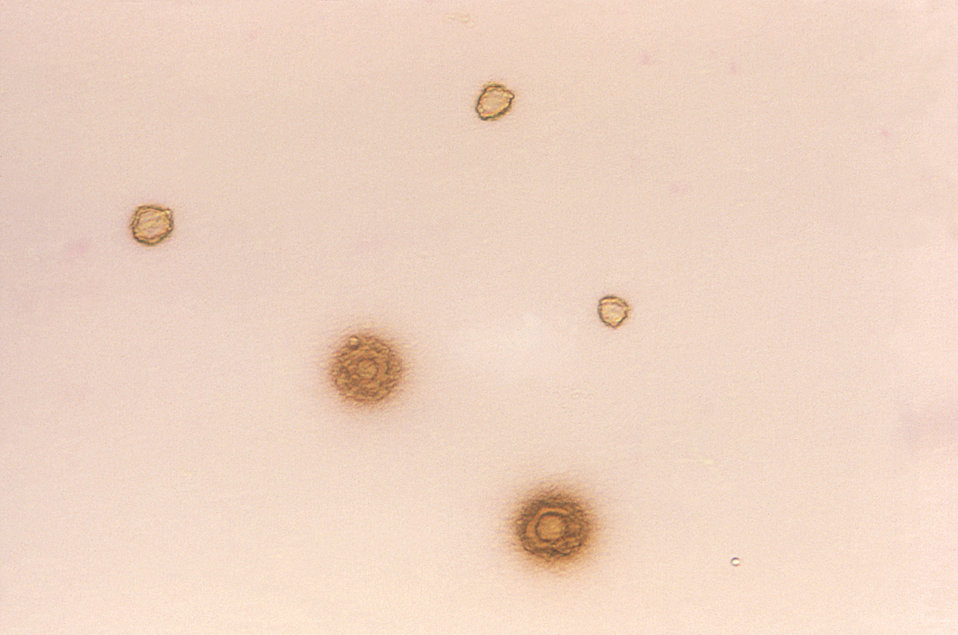
“Fried-egg” appearance of Mycoplasma hominis colonies
Image: “Gram-negative Mycoplasma hominis” by the CDC/ Dr. E. Arum. License: Public domain.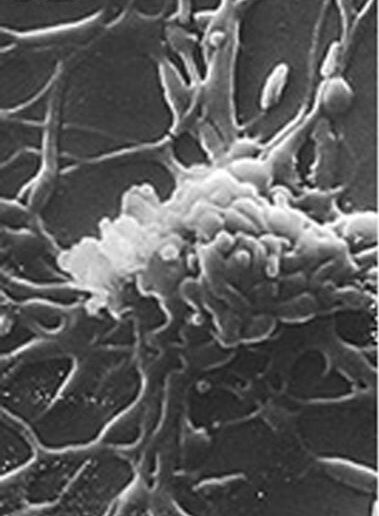
Scanning electron microscope image of M. pneumoniae, a pleomorphic bacterium lacking a cell wall, seen here in its filamentous form
Image: “Mycoplasma pneumoniae” by Rottem et al. License: CC BY 3.0, edited by Lecturio.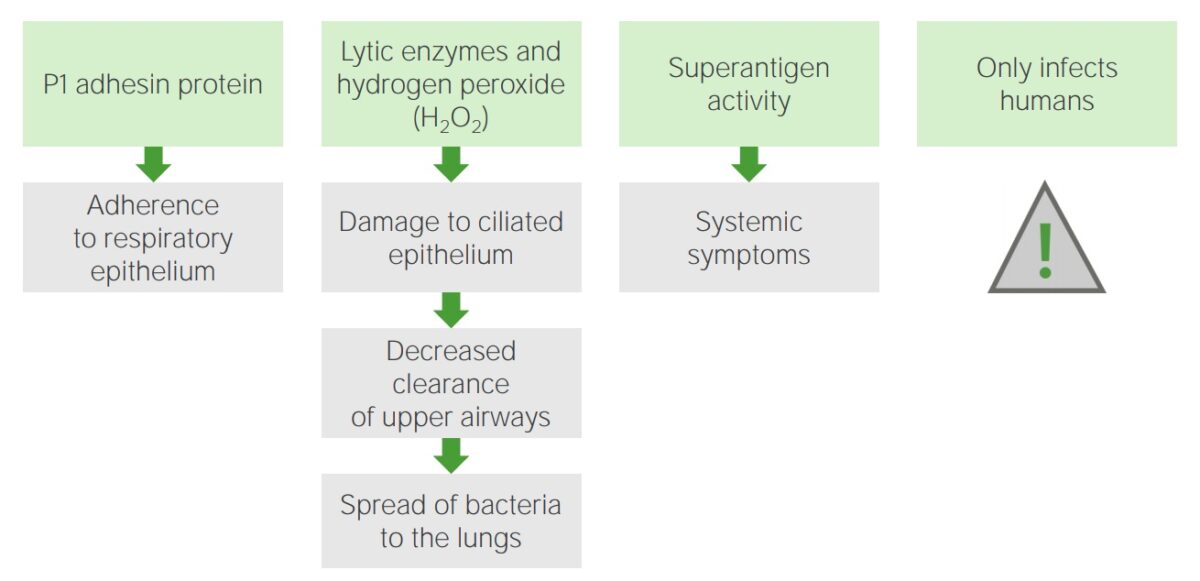
Mechanisms of pathogenesis: Mycoplasma pneumoniae
Image by Lecturio. License: CC BY-NC-SA 4.0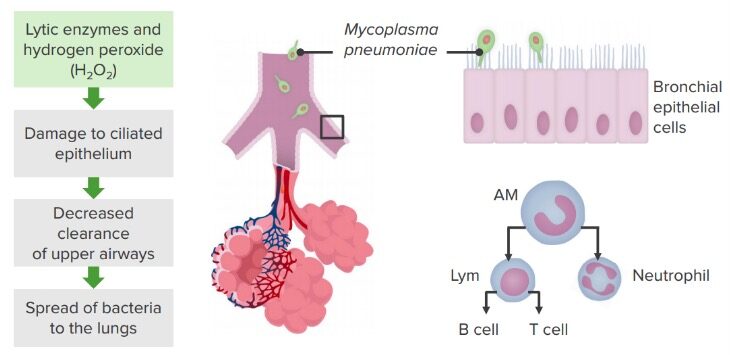
Mechanisms of pathogenesis: Mycoplasma pneumoniae
Image by Lecturio. License: CC BY-NC-SA 4.0Pathology caused by the M. pneumoniae bacterium is varied; however, diagnosis and treatment are standard:

M. pneumoniae-associated mucositis (MPAM): Erosive oral lesions are limited to the mucosa in this form of MPAM in a 24-year-old woman.
Image: “MPAM” by the Department of Pediatrics, Division of Pediatric Infectious Diseases and Immunology, Erasmus MC-Sophia Children’s Hospital, University Medical Center Rotterdam, Netherlands. License: CC BY 4.0.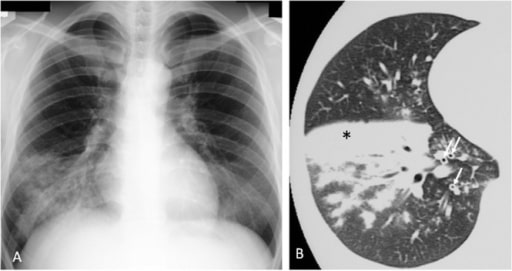
Mycoplasma pneumoniae pneumonia in a human. A: Chest X-ray shows infiltrates in the right lower lobe.
B: consolidation (∗) and bronchovascular bundles thickening (↑) on computed tomography (CT) scan
| Characteristics | Mycoplasma pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia | Pneumococcal pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia |
|---|---|---|
| Type of pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia | Atypical (interstitial) | Typical (alveolar) |
| Preceding pharyngitis Pharyngitis Pharyngitis is an inflammation of the back of the throat (pharynx). Pharyngitis is usually caused by an upper respiratory tract infection, which is viral in most cases. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, and hoarseness. Pharyngitis | Common | Never |
| Onset | Gradual | Sudden with chills Chills The sudden sensation of being cold. It may be accompanied by shivering. Fever |
| Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever | Low grade | High grade |
| Cough | Non-productive, paroxysmal | Productive |
| Pleuritic chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | Absent | Present |
| Leukocytosis Leukocytosis A transient increase in the number of leukocytes in a body fluid. West Nile Virus | Absent | Present |
| Age of highest incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency | Young adults < 30 years old | Older adults |
| Complications | Otitis media, erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion multiforme, hemolytic anemia Hemolytic Anemia Hemolytic anemia (HA) is the term given to a large group of anemias that are caused by the premature destruction/hemolysis of circulating red blood cells (RBCs). Hemolysis can occur within (intravascular hemolysis) or outside the blood vessels (extravascular hemolysis). Hemolytic Anemia, myocarditis Myocarditis Myocarditis is an inflammatory disease of the myocardium, which may occur alone or in association with a systemic process. There are numerous etiologies of myocarditis, but all lead to inflammation and myocyte injury, most often leading to signs and symptoms of heart failure. Myocarditis, pericarditis Pericarditis Pericarditis is an inflammation of the pericardium, often with fluid accumulation. It can be caused by infection (often viral), myocardial infarction, drugs, malignancies, metabolic disorders, autoimmune disorders, or trauma. Acute, subacute, and chronic forms exist. Pericarditis, bullous otitis media | Bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides, meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis, otitis media |