Scoliosis is a structural alteration of the vertebral column Vertebral column The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy characterized by a lateral spinal curvature of greater than 10 degrees in the coronal Coronal Computed Tomography (CT) plane. Scoliosis can be classified as idiopathic Idiopathic Dermatomyositis (in most cases) or secondary to underlying conditions. Other classifications are according to etiology, location, and severity. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with spinal asymmetry Asymmetry Examination of the Upper Limbs and often have associated pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. Diagnosis is initially clinical and is confirmed later by X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests. Management can be conservative or surgical, depending on the severity.
Last updated: Mar 29, 2023
Scoliosis is a lateral spinal curvature of the spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy greater than 10 degrees in the coronal Coronal Computed Tomography (CT) plane, usually accompanied by rotation Rotation Motion of an object in which either one or more points on a line are fixed. It is also the motion of a particle about a fixed point. X-rays of variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables amounts.
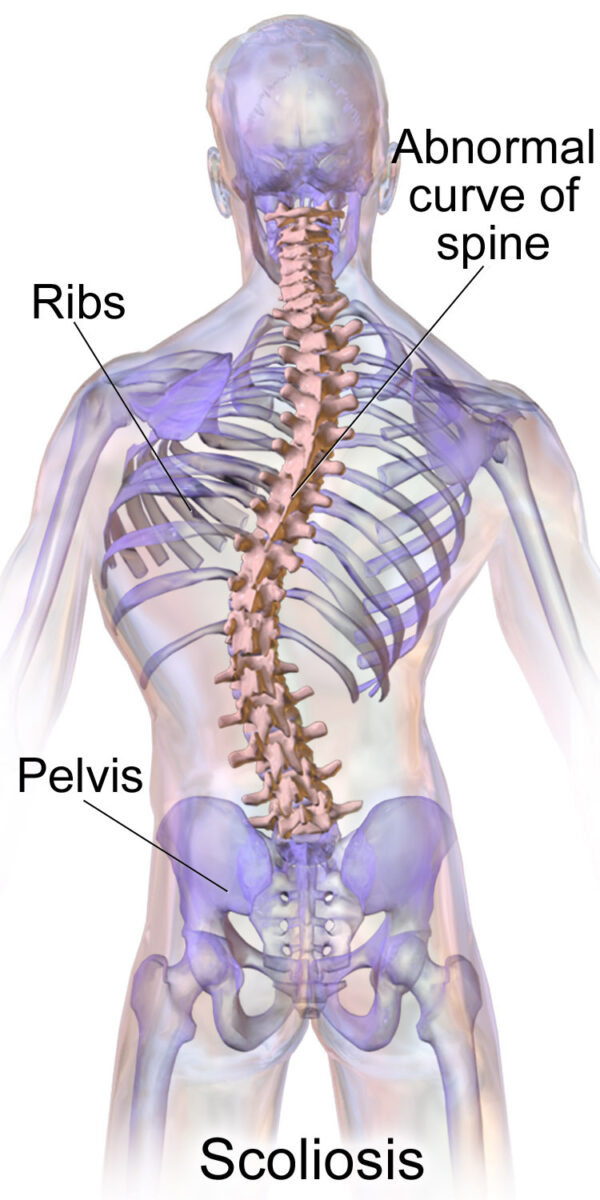
Scoliosis
Image: “Blausen 0785 Scoliosis 01” by Blausen. License: CC BY 3.0Scoliosis can develop de novo or as a continuation of congenital Congenital Chorioretinitis, idiopathic Idiopathic Dermatomyositis, or early-developed scoliosis. The uneven loading of the spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy produces and exacerbates the pathological curvature seen in scoliosis.
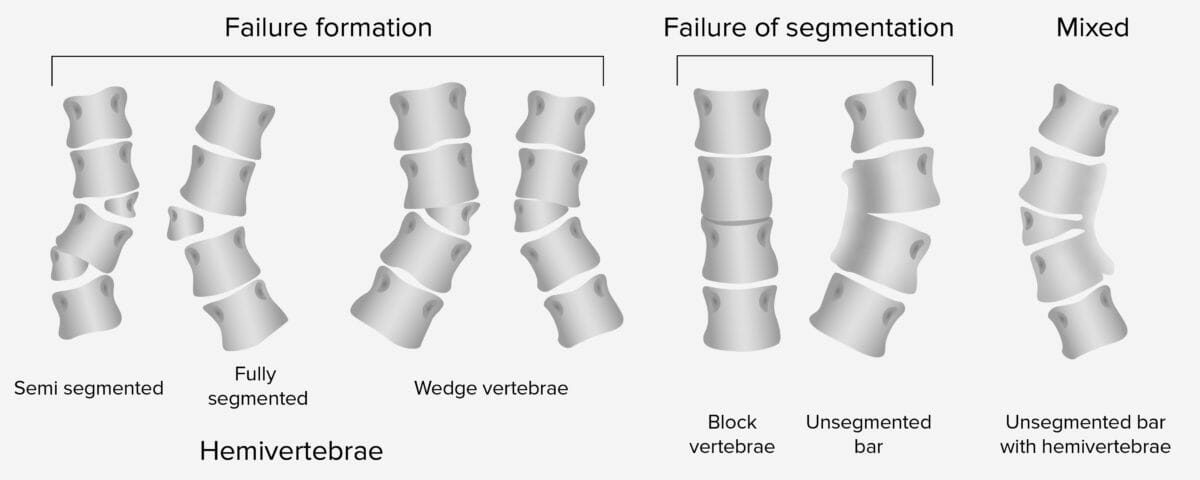
Classification of congenital scoliosis
Image by Lecturio.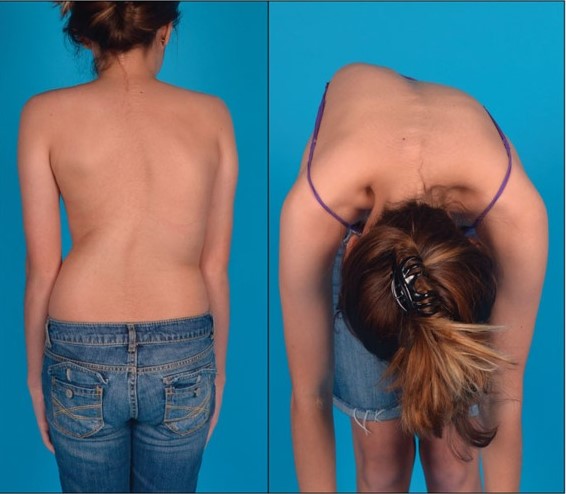
Patient with scoliosis performing the forward-bending, or Adams, test showing the “hump” that develops when the patient bends over, demonstrating a positive test for scoliosis
Image: “Idiopathic scoliosis in an adolescent female” by Sharma, S. et al. License: CC BY 4.0, cropped by Lecturio.
Measurement of the rib hump of a scoliosis patient in the forward bending position using a scoliometer: The examiner is looking for the highest reading detected in the thoracic spine.
Image: “Measurement of the rib hump of a scoliosis patient” by Izatt MT, Bateman GR, Adam CJ. License: CC BY 2.0
Measurement of the rib hump on a plaster model (left) and a scoliosis patient (right), using a smartphone and the Scoliogauge app in combination with an acrylic sleeve to reflect the dimensions of the traditional scoliometer
Image: “Measurement of the rib hump” by Izatt MT, Bateman GR, Adam CJ. License: CC BY 2.0Diagnosis is initially made clinically and later confirmed by X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests, which will show the presence of spinal curvature. Idiopathic Idiopathic Dermatomyositis scoliosis is a diagnosis of exclusion.

X-ray showing thoracic dextroscoliosis, or right thoracic spinal curvature
Image: “Idiopathic scoliosis in an adolescent female” by Sharma, S., et al. License: CC BY 4.0, cropped by Lecturio.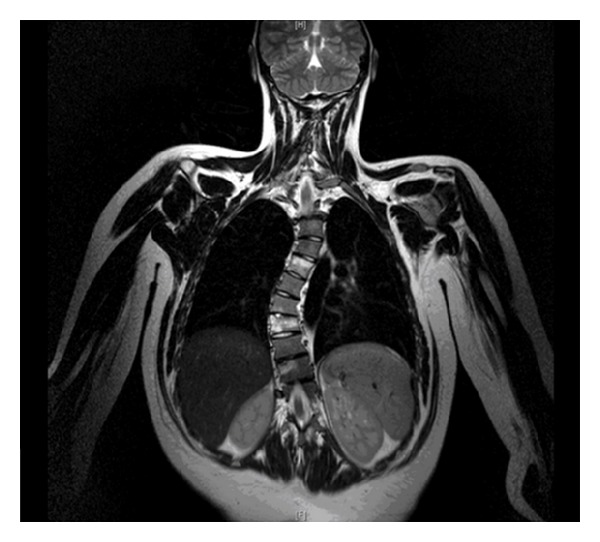
MRI of a patient with recurrent osteomyelitis causing thoracic dextroscoliosis
Image: “Coronal Thoracic Spine MRI image” by Alexander Armstrong et al. License: CC BY 3.0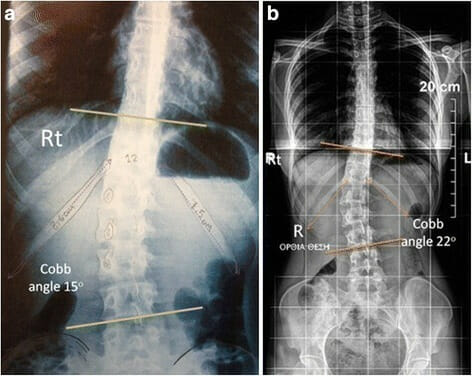
Right lumbar idiopathic curve with Cobb angle of 15° b: Right lumbar idiopathic curve with Cobb angle of 22°
Image: “Right lumbar idiopathic curve 15° of Cobb angle, the right 12th rib is longer, similarly in figure b, in a right lumbar idiopathic curve 22° of Cobb angle, the right 12th rib is longer” by Theodoros B Grivas. License: CC BY 4.0Management ranges from conservative to surgical depending on the degree of scoliosis.
The prognosis Prognosis A prediction of the probable outcome of a disease based on a individual’s condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas of scoliosis is dependent on the underlying cause, comorbidities Comorbidities The presence of co-existing or additional diseases with reference to an initial diagnosis or with reference to the index condition that is the subject of study. Comorbidity may affect the ability of affected individuals to function and also their survival; it may be used as a prognostic indicator for length of hospital stay, cost factors, and outcome or survival. St. Louis Encephalitis Virus, and deformity Deformity Examination of the Upper Limbs at the time of presentation.
The following conditions are associated with scoliosis: