Back pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is a common complaint among the general population and is mostly self-limiting Self-Limiting Meningitis in Children. Back pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can be classified as acute, subacute, or chronic depending on the duration of symptoms. The wide variety of potential etiologies include degenerative, mechanical, malignant, infectious, rheumatologic, and extraspinal causes. A thorough history and physical examination is necessary to guide the diagnosis. Additional workup is not required unless evidence of severe diseases exists (e.g., neurologic deficits Neurologic Deficits High-Risk Headaches, urinary/ fecal incontinence Fecal incontinence Failure of voluntary control of the anal sphincters, with involuntary passage of feces and flatus. Pediatric Constipation, infectious symptoms, or malignancy Malignancy Hemothorax). Management varies depending on the cause, but most cases are managed with conservative measures and analgesics.
Last updated: Mar 29, 2023
Back pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is a common complaint among adults:
Back pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is classified based on the duration of symptoms:
Important, open-ended questions to ask when evaluating an individual with pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can be remembered with OPQRST mnemonic:
General examination:
Specific maneuvers:

Patrick’s test for evaluating sacroiliac or hip disorders as a potential cause of back pain. It is also known as the FABERE test (for flexion, abduction, external rotation, and extension).
Image by Lecturio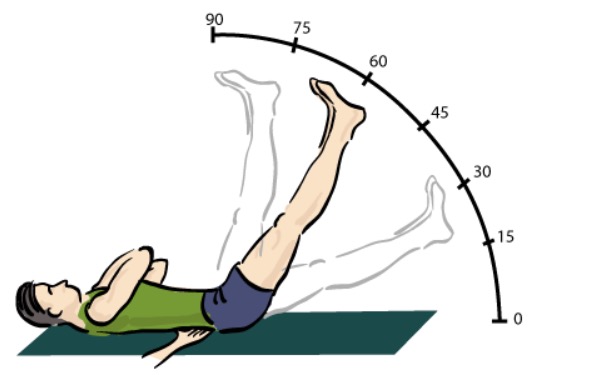
Straight leg-raising test for evaluating back pain:
A positive test occurs if radicular pain is elicited, most often between 30–60 degrees of elevation.
The following symptoms suggest serious pathology and should elicit an urgent evaluation:
The majority of individuals with back pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways do not require imaging.
Indications:
Imaging modalities:

Magnetic resonance imaging (MRI) of the cervical spine demonstrating an epidural abscess and vertebral osteomyelitis:
Arrows indicate high signal on vertebrae C4–C7 due to osteomyelitis; arrowheads mark the epidural abscess.
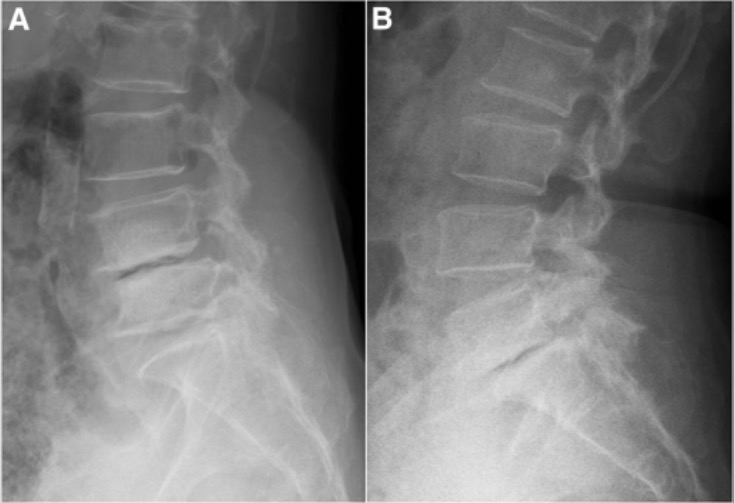
Radiograph images demonstrating spondylolisthesis:
A: degenerative spondylolisthesis at the L4–L5 level (note the narrow intervertebral space and forward displacement of the upper vertebra)
B: spondylolisthesis at L5–S1

Magnetic resonance imaging (MRI) showing intervertebral disk herniation and schwannoma:
a: T2-weighted sagittal image reveals L3–L4 disk herniation compressing the dural sac from the right side
b: a hyperintense, intradural mass at the same level 2 slices away
c: T1-weighted sagittal image demonstrating a hypointense mass behind the L3–L4 intervertebral disks