Hepatocellular carcinoma (HCC) typically arises in a chronically diseased or cirrhotic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy and is the most common primary liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy cancer. Diagnosis may include ultrasound, CT, MRI, biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma (if inconclusive imaging), and/or biomarkers. Treatment options include resection and chemo-/radiotherapy, and liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy transplantation in select cases. Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy metastases are much more common than primary liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy cancers and usually originate from colorectal, lung, breast, and pancreatic primary sites. Metastases are most commonly diagnosed by CT or PET PET An imaging technique that combines a positron-emission tomography (PET) scanner and a ct X ray scanner. This establishes a precise anatomic localization in the same session. Nuclear Imaging scans. Management depends on the type and stage of primary cancer.
Last updated: May 17, 2024
Cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis:
One-third of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis will develop HCC during their lifetime, including those caused by:
Other:
Hepatocytes Hepatocytes The main structural component of the liver. They are specialized epithelial cells that are organized into interconnected plates called lobules. Liver: Anatomy show “large-cell change” and “small-cell change” with abnormal architecture (thick trabeculae) microscopically.
Gross appearance:
Microscopic appearance:
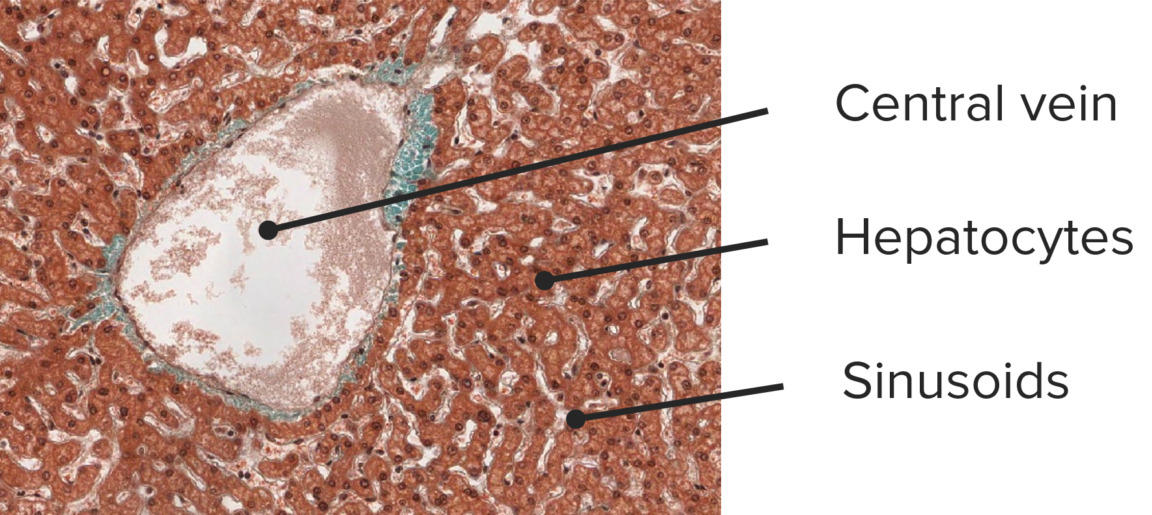
Histology of a normal liver:
microphotograph of a normal liver with a dilated central vein but normal architecture showing thin (single-cell layer) trabeculae (trichrome stain, 100x)
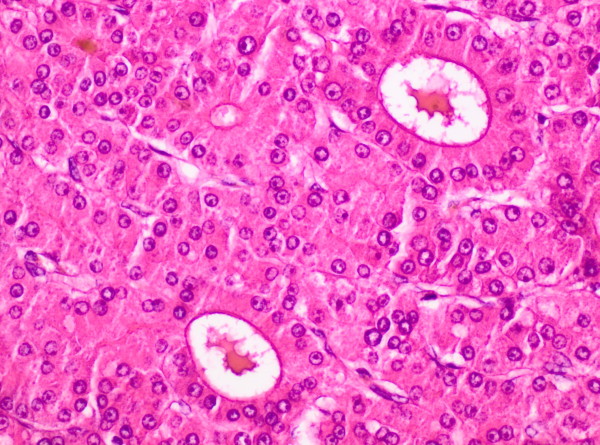
Histology of hepatocellular carcinoma (HCC):
microphotograph of a moderately differentiated HCC showing pattern of thickened (2–6 cell layers) trabeculae surrounded by flattened endothelial cells. Note the brown bile pigment in the top left and the 2 large pseudoglandular spaces containing pink proteinaceous material. The hepatocytes show moderate atypia. Compare the thickened trabeculae to the single-cell trabeculae in a normal liver.
Four possible clinical presentations for HCC:
Surveillance Surveillance Developmental Milestones and Normal Growth screening Screening Preoperative Care by ultrasound every 6 months is recommended for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship in the following high-risk groups:
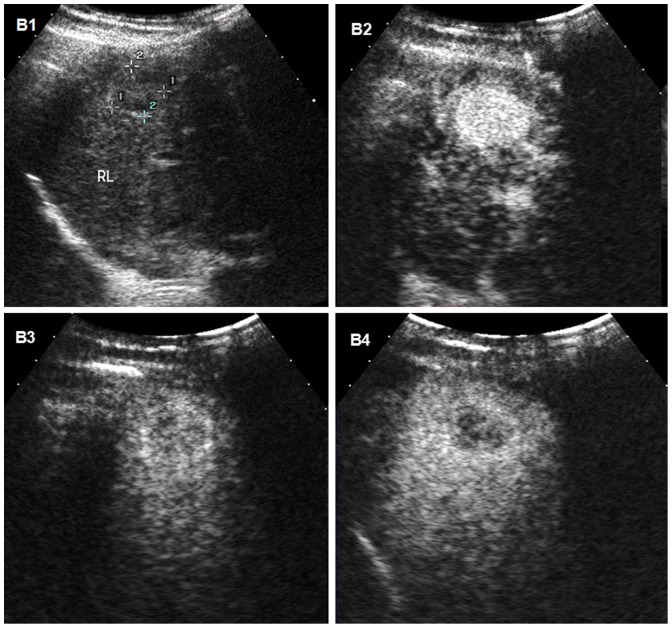
Hepatocellular carcinoma (HCC) on ultrasound: ultrasound images of HCC in the liver of a 31-year-old man with cirrhosis
B1: conventional ultrasound showing the mass as a poorly defined, hypoechoic nodule
B2, B3, B4: time-sequenced contrast-enhanced ultrasound (CEUS) images after injection of a microbubble contrast agent
B2: typical hypervascularity (enhancement) of HCC during the arterial phase at 95 sec after injection of the contrast agent
B3, B4: mass becoming hypoechoic in the portal and late phases
B4: late-phase image showing mild washout of contrast medium at 179 sec, which helps differentiate HCC from cholangiocarcinoma or metastatic tumor (more rapid washout times)
If ultrasound shows a lesion > 1 cm, dynamic contrast imaging by CT or MRI is performed.
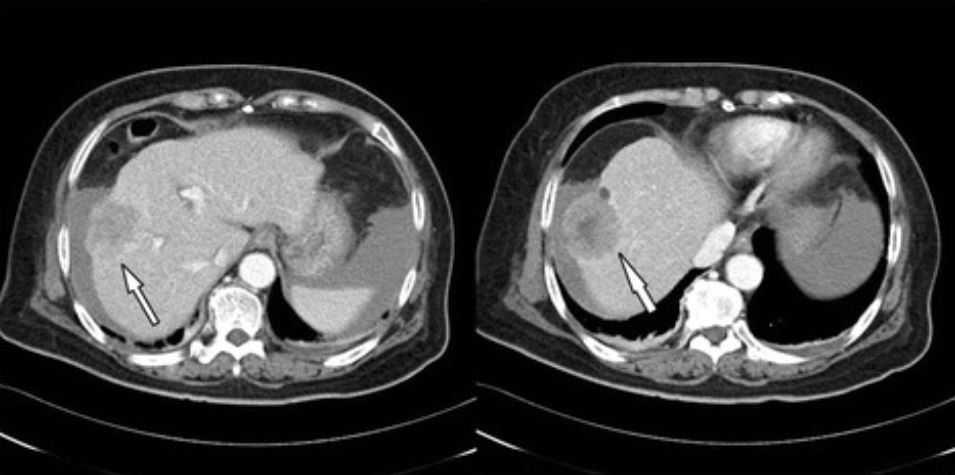
Hepatocellular carcinoma (HCC) on computed tomography (CT):
triphasic abdominal CT revealing a large tumor (4.8 cm in diameter) in the right lobe compatible with HCC (arrow)
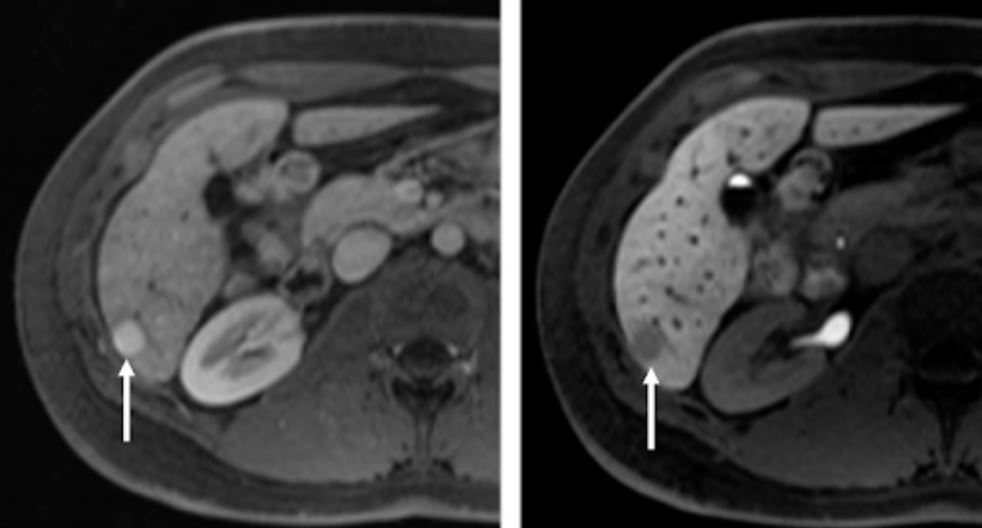
Typical magnetic resonance imaging (MRI) characteristics of hepatocellular carcinoma (HCC):
axial MRI of the liver after intravenous (IV) administration of a hepatocyte-specific contrast agent in arterial (left) and hepatobiliary (right) phases 20 min after IV contrast application
In segment 6, a hypervascular lesion is observed (left image, arrow pointing to the lesion).
In the hepatobiliary phase, the lesion (right image, arrow pointing to the lesion) is hypointense in relation to the surrounding liver secondary to reduced uptake of contrast agent due to loss of functioning hepatocytes in the poorly differentiated HCC lesion.
If imaging results are unequivocal, a biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is not always needed.
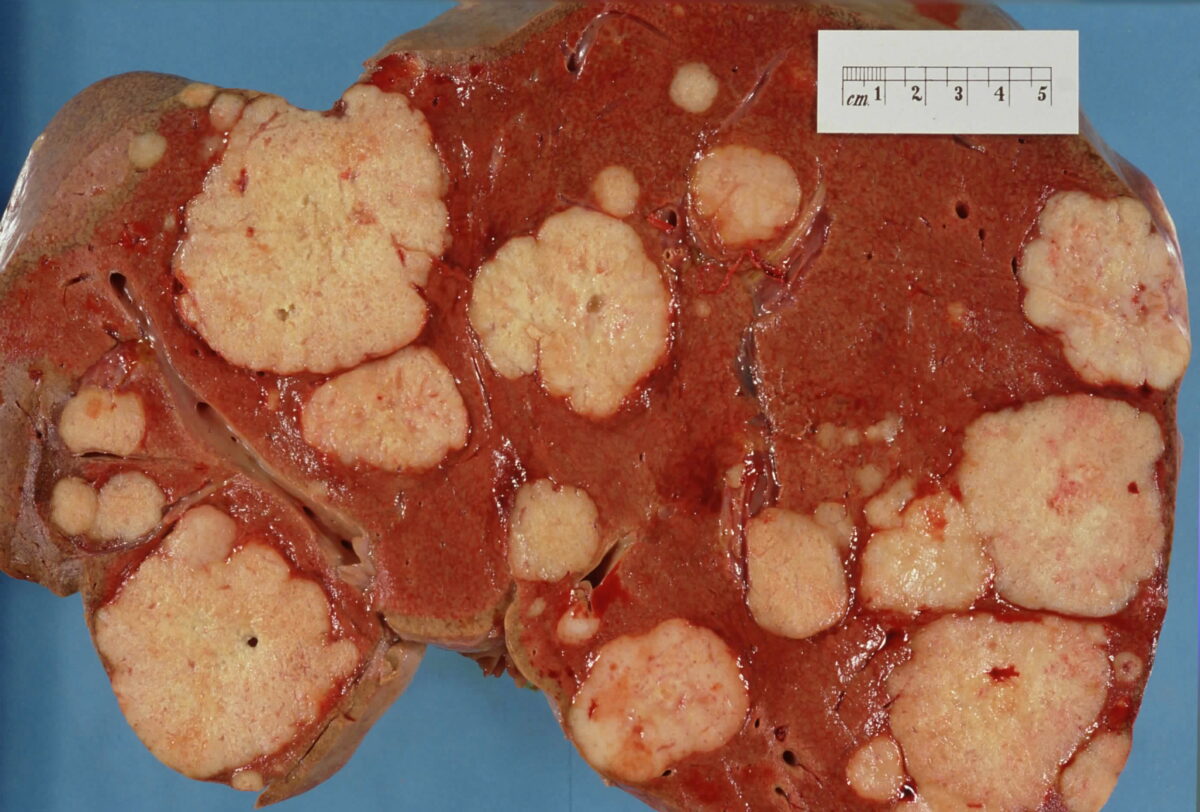
Gross specimen of the liver showing multiple metastatic tumors
Image: “Secondary tumor deposits in the liver from a primary cancer of the pancreas” by John Hayman. License: Public DomainThe following are important differential diagnoses of a solid mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast in the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy:
Benign Benign Fibroadenoma lesions:
Malignant lesions:
Cholangiocarcinoma Cholangiocarcinoma A malignant tumor arising from the epithelium of the bile ducts. Rare Malignant Liver Tumors ( bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy duct cancer): arises from epithelial cells of the intrahepatic and extrahepatic bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy ducts. Risk factors in the United States include primary sclerosing cholangitis Primary Sclerosing Cholangitis Primary sclerosing cholangitis (PSC) is an inflammatory disease that causes fibrosis and strictures of the bile ducts. The exact etiology is unknown, but there is a strong association with IBD. Patients typically present with an insidious onset of fatigue, pruritus, and jaundice, which can progress to cirrhosis and complications related to biliary obstruction. Primary Sclerosing Cholangitis and fibropolycystic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease (e.g., choledochal cysts Cysts Any fluid-filled closed cavity or sac that is lined by an epithelium. Cysts can be of normal, abnormal, non-neoplastic, or neoplastic tissues. Fibrocystic Change). Hepatolithiasis Hepatolithiasis Rare Malignant Liver Tumors (recurrent pyogenic cholangitis) is the biggest risk factor for cholangiocarcinoma Cholangiocarcinoma A malignant tumor arising from the epithelium of the bile ducts. Rare Malignant Liver Tumors in Asia ASIA Spinal Cord Injuries.