The parathyroid glands are 2 pairs of small endocrine glands Endocrine glands Ductless glands that secrete hormones directly into the blood circulation. These hormones influence the metabolism and other functions of cells in the body. Glandular Epithelium: Histology found in close proximity to the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. The glands secrete parathyroid hormone, which plays a key role in regulating calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes levels.
Last updated: Nov 19, 2024
The parathyroid glands are derived from pharyngeal pouches Pharyngeal pouches Branchial Apparatus and Aortic Arches, which originate in the mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation.
Structure:
Relations: posterior aspect of the lateral lobes of the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland
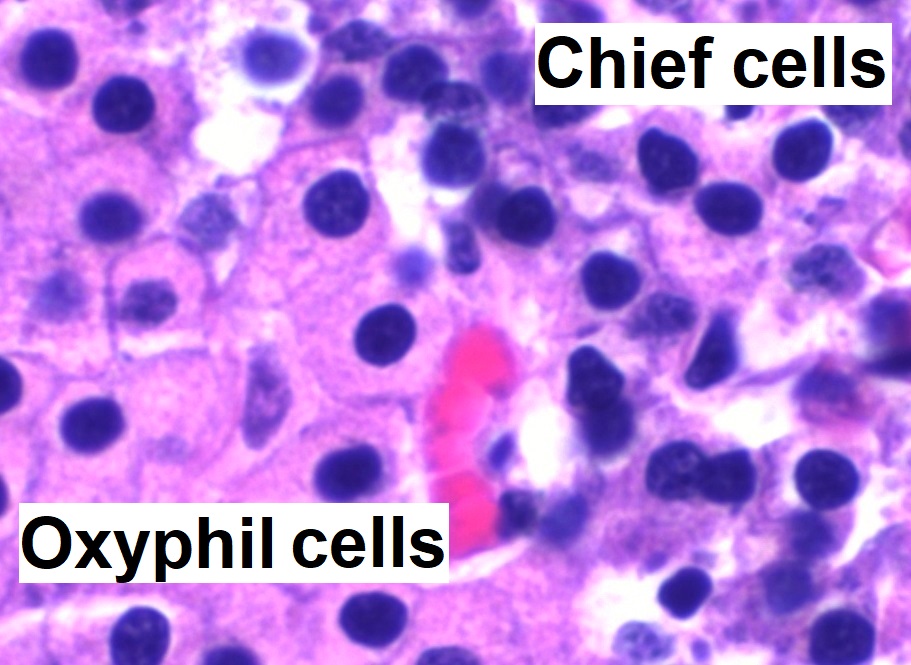
High magnification micrograph with hematoxylin and eosin (H&E) stain:
The small, dark cells are chief cells, which are responsible for secreting parathyroid hormone (PTH). The cells with the orange-/pink-stained cytoplasm are oxyphil cells.
Effects of the parathyroid glands are exerted through chief cells Chief cells Epithelial cells that line the basal half of the gastric glands. Chief cells synthesize and export an inactive enzyme pepsinogen which is converted into the highly proteolytic enzyme pepsin in the acid environment of the stomach. Stomach: Anatomy, which produce and secrete parathyroid hormone (PTH):