A goiter is a chronic enlargement of the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland due to nonneoplastic growth occurring in the setting of hypothyroidism Hypothyroidism Hypothyroidism is a condition characterized by a deficiency of thyroid hormones. Iodine deficiency is the most common cause worldwide, but Hashimoto's disease (autoimmune thyroiditis) is the leading cause in non-iodine-deficient regions. Hypothyroidism, hyperthyroidism Hyperthyroidism Hypersecretion of thyroid hormones from the thyroid gland. Elevated levels of thyroid hormones increase basal metabolic rate. Thyrotoxicosis and Hyperthyroidism, or euthyroidism. Morphologically, thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy enlargement can be diffuse (smooth consistency Consistency Dermatologic Examination) or nodular (uninodular or multinodular). Hashimoto’s thyroiditis Thyroiditis Thyroiditis is a catchall term used to describe a variety of conditions that have inflammation of the thyroid gland in common. It includes pathologies that cause an acute illness with severe thyroid pain (e.g., subacute thyroiditis and infectious thyroiditis) as well as conditions in which there is no clinically evident inflammation and the manifestations primarily reflect thyroid dysfunction or a goiter (e.g., painless thyroiditis and fibrous Riedel's thyroiditis). Thyroiditis is associated with a benign Benign Fibroadenoma hypothyroid goiter, while Graves’ disease Graves’ disease A common form of hyperthyroidism with a diffuse hyperplastic goiter. It is an autoimmune disorder that produces antibodies against the thyroid stimulating hormone receptor. These autoantibodies activate the TSH receptor, thereby stimulating the thyroid gland and hypersecretion of thyroid hormones. These autoantibodies can also affect the eyes (Graves ophthalmopathy) and the skin (Graves dermopathy). Thyrotoxicosis and Hyperthyroidism produces a toxic or hyperthyroid goiter. Nontoxic goiter is euthyroid Euthyroid Thyroiditis and is usually due to iodine Iodine A nonmetallic element of the halogen group that is represented by the atomic symbol I, atomic number 53, and atomic weight of 126. 90. It is a nutritionally essential element, especially important in thyroid hormone synthesis. In solution, it has anti-infective properties and is used topically. Thyroid Hormones deficiency (the most common cause of goiter). Diagnostic tests Diagnostic tests Diagnostic tests are important aspects in making a diagnosis. Some of the most important epidemiological values of diagnostic tests include sensitivity and specificity, false positives and false negatives, positive and negative predictive values, likelihood ratios, and pre-test and post-test probabilities. Epidemiological Values of Diagnostic Tests include thyroid function tests Thyroid Function Tests Blood tests used to evaluate the functioning of the thyroid gland. Ion Channel Myopathy and measurement of thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions. Ultrasound, CT, and/or MRI help if lab results are ambiguous and if worrisome features such as obstructive symptoms are present. Radioactive iodine uptake Radioactive Iodine Uptake Thyrotoxicosis and Hyperthyroidism distinguishes hyperthyroid causes. Treatment depends on the underlying condition; options include observation, medication, surgery, and radioiodine ablation Radioiodine Ablation Thyrotoxicosis and Hyperthyroidism.
Last updated: May 17, 2024
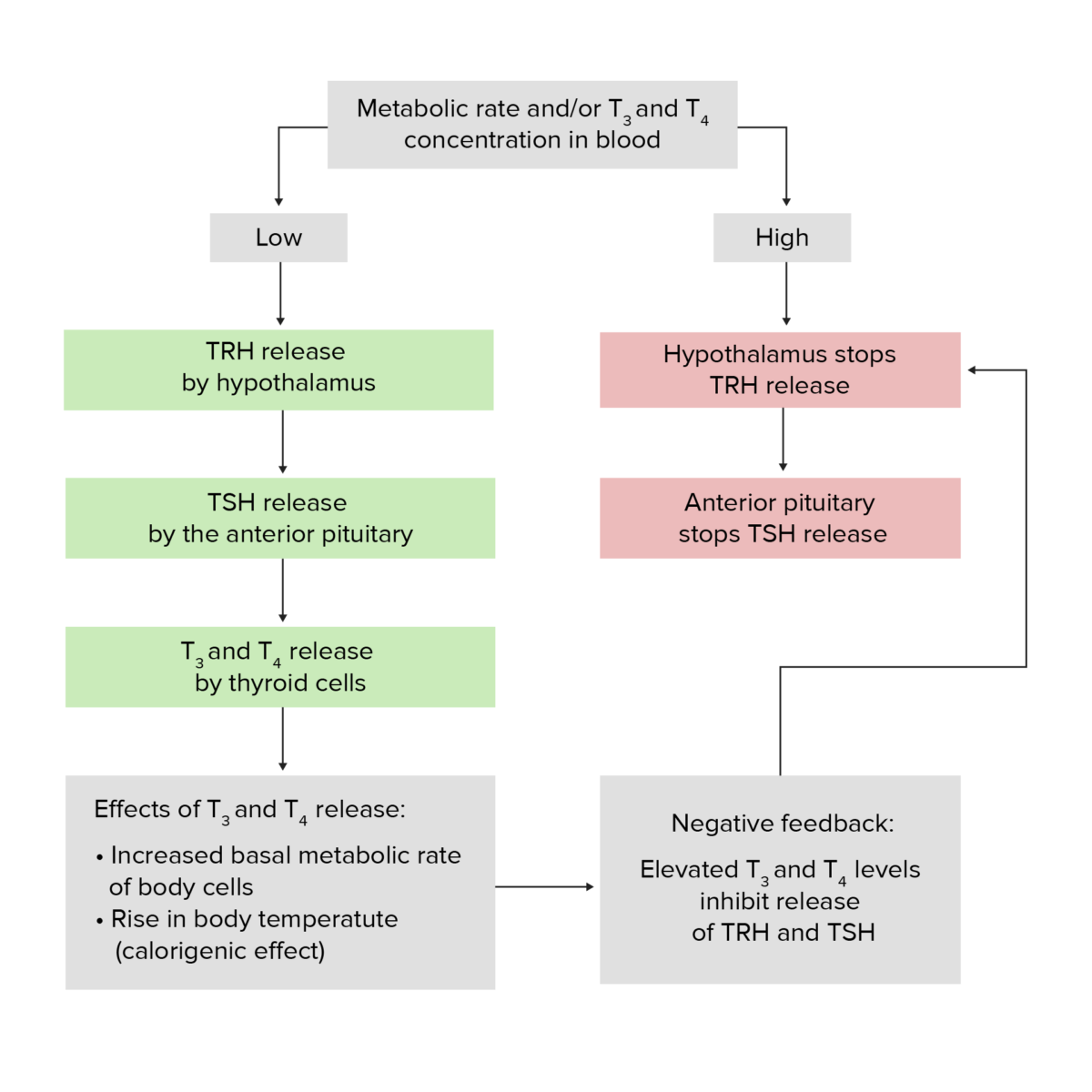
Hypothalamic–pituitary–thyroid axis feedback loop:
When the thyroid hormones are low, the hypothalamus releases TRH, and this triggers the pituitary gland to secrete TSH. This stimulates the thyroid gland to produce T4 and T3. Approximately ⅓ of the T4 produced is converted to the much more bioactive form T3.
Increase in free or unbound T3/T4 creates negative feedback, inhibiting the release of TRH and TSH.
| Grade | Severity of goiter |
|---|---|
| 0 | No goiter |
| 1 |
|
| 2 | Clearly visible swelling Swelling Inflammation in the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess when the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess is in a normal position and is consistent with an enlarged thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland when the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess is palpated |
Identify thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy function and possible underlying cause:
Identify goiter size and presence of nodule Nodule Chalazion with its characteristics and obstructive effect:
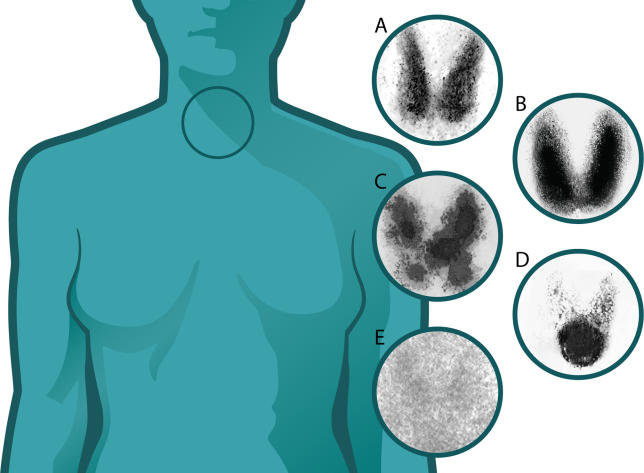
Thyroid uptake scans:
(A) Normal
(B) Graves’ disease: diffuse increased uptake in both thyroid lobes
(C) Toxic multinodular goiter: “hot” and “cold” areas of uneven uptake
(D) Toxic adenoma: increased uptake in a single nodule with suppression of the surrounding thyroid
(E) Thyroiditis: decreased or absent uptake

Goiter with obstructive effect:
CT of the neck illustrating compression of the trachea and esophagus by the goiter
Evaluate worrisome features (suspected malignancy Malignancy Hemothorax) with fine-needle aspiration biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma: