Graves' disease is an autoimmune disorder characterized by the presence of circulating thyroid-stimulating hormone (TSH) receptor antibodies, which cause the thyroid gland to hyperfunction. Clinical features include those of hyperthyroidism, as well as orbitopathy, goiter, and dermopathy/pretibial myxedema. Diagnosis is by thyroid laboratory tests showing a low TSH, elevated thyroid hormones (thyroxine (T4) and triiodothyronine (T3)) and thyrotropin-receptor antibodies (TRAbs; particularly the thyroid-stimulating immunoglobulins subtype). If initial tests are nondiagnostic, radioactive iodine uptake (increased uptake) and thyroid ultrasound (diffuse thyroid enlargement) provide diagnostic information. Treatment options include antithyroid drugs, radioiodine ablation, and surgery.
Last updated: May 17, 2024
Graves’ disease is an autoimmune disorder Autoimmune Disorder Septic Arthritis in which antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions against the thyroid-stimulating hormone Thyroid-stimulating hormone A glycoprotein hormone secreted by the adenohypophysis. Thyrotropin stimulates thyroid gland by increasing the iodide transport, synthesis and release of thyroid hormones (thyroxine and triiodothyronine). Thyroid Hormones (TSH) receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors cause the thyroid Thyroid The thyroid gland is one of the largest endocrine glands in the human body. The thyroid gland is a highly vascular, brownish-red gland located in the visceral compartment of the anterior region of the neck. Thyroid Gland: Anatomy gland to hyperfunction. The syndrome may have the following features:
Susceptibility to Graves’ disease is considered to be a combination of multiple factors.
Risk factors:
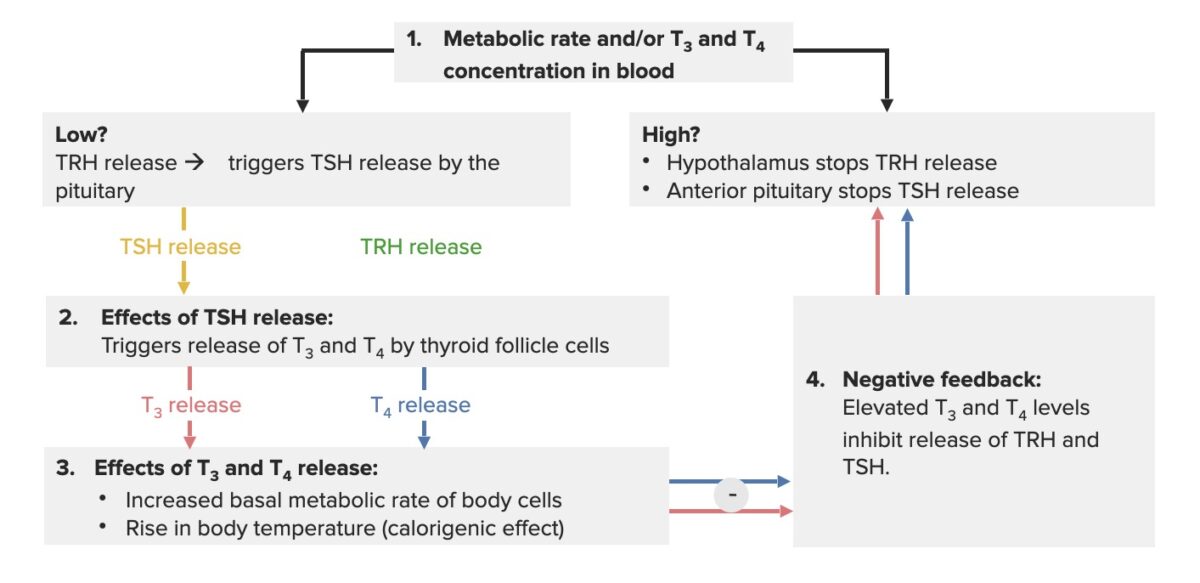
Hypothalamus-pituitary-thyroid axis feedback loop:
When the thyroid hormones are low, the hypothalamus releases thyrotropin-releasing hormone (TRH), which triggers the pituitary gland to secrete TSH. The effect of this process is that the thyroid gland produces thyroxine (T4) and triiodothyronine (T3) (more T4 is produced, as it gets converted to T3). The increase in thyroid hormones (free or unbound T3/T4) creates a negative feedback, inhibiting TRH and TSH release.
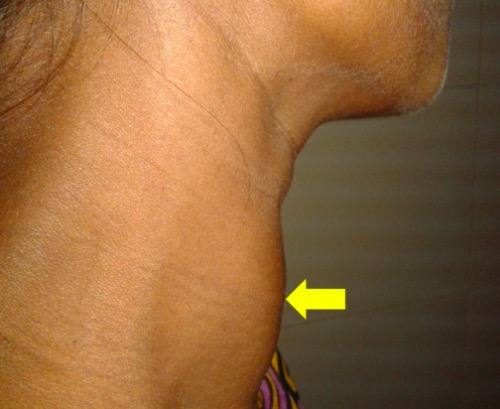
Goiter: diffusely enlarged thyroid gland (arrow) in a 30-year-old pregnant woman
Image: “Diffusely enlarged thyroid gland” by Department of Cardiology, Dhaka Medical College Hospital, Dhaka, Bangladesh. License: CC BY 4.0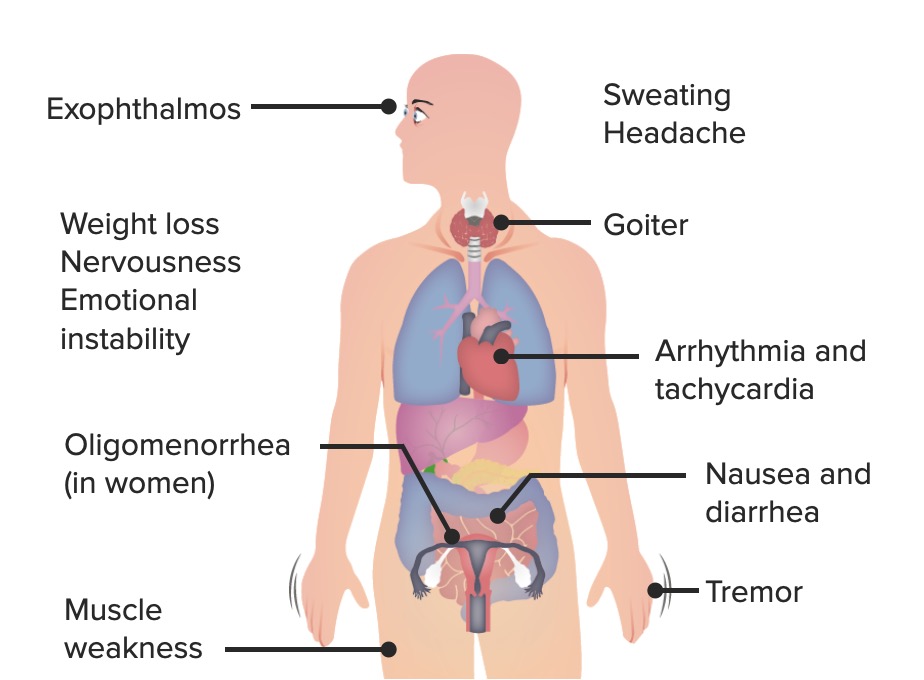
The most common signs and symptoms of Graves’ disease
Image by Lecturio.
Ophthalmologic effect of Graves’ disease: bilateral infiltrative thyroid-associated ophthalmopathy in a 33-year-old woman
Image: “Thyroid-associated ophthalmopathy” by Esra Şahlı and Kaan Gündüz. License: CC BY 2.5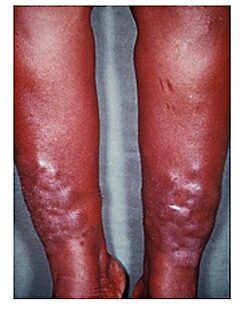
Myxedema
Image: “Myxedema” by Herbert L. Fred, MD and Hendrik A. van Dijk. License: CCC BY 2.0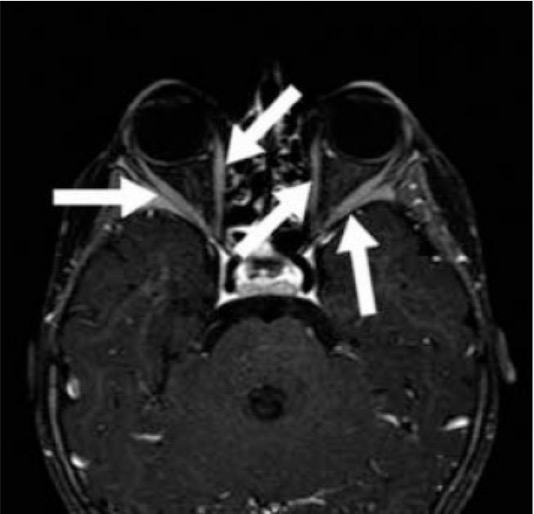
Graves’ orbitopathy: Contrast-enhanced axial MRI of a 2-year-old patient with Graves’ disease shows marked enhancement of extraocular muscles (arrows) of bilateral orbits.
Image: “T1 weighted fat saturated contrast enhanced axial MR” by Mustafa Kemal University School of Medicine, Department of Nuclear Medicine, Hatay, Turkey. License: CC BY 2.5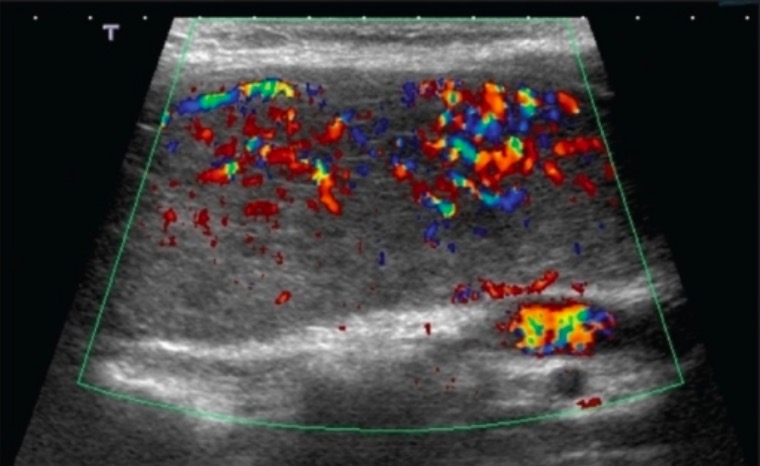
Thyroid ultrasonography with Doppler in Graves’ disease: a 28-year-old woman with Graves’ disease whose ultrasound with Doppler finding shows diffuse colour flow representing intense vascularity (“thyroid inferno”)
Image: “Ultrasound of the thyroid” by Saleh Aldasouqi et al. License: CC BY 2.0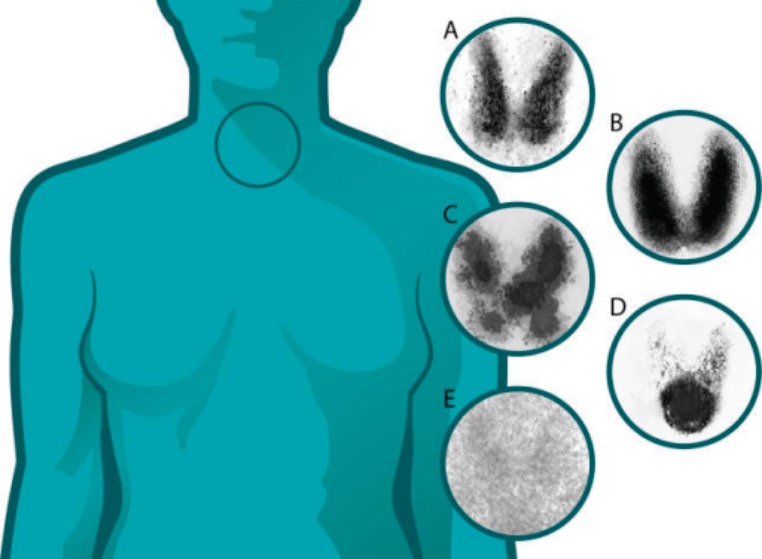
Thyroid uptake scans (thyroiditis versus other thyroid diseases):
A: normal
B: Graves’ disease: diffuse increased uptake in both thyroid lobes
C: toxic multinodular goiter: “hot” and “cold” areas of uneven uptake
D: toxic adenoma: increased uptake in a single nodule with suppression of the surrounding thyroid
E: thyroiditis: decreased or absent uptake