Influenza viruses Viruses Minute infectious agents whose genomes are composed of DNA or RNA, but not both. They are characterized by a lack of independent metabolism and the inability to replicate outside living host cells. Virology are members of the Orthomyxoviridae family and the causative organisms of influenza, a highly contagious febrile respiratory disease. There are 3 primary influenza viruses Viruses Minute infectious agents whose genomes are composed of DNA or RNA, but not both. They are characterized by a lack of independent metabolism and the inability to replicate outside living host cells. Virology (A, B, and C) and various subtypes, which are classified based on their virulent surface antigens, hemagglutinin Hemagglutinin Agents that cause agglutination of red blood cells. They include antibodies, blood group antigens, lectins, autoimmune factors, bacterial, viral, or parasitic blood agglutinins, etc. Measles Virus ( HA HA Hemolytic anemia (HA) is the term given to a large group of anemias that are caused by the premature destruction/hemolysis of circulating red blood cells (RBCs). Hemolysis can occur within (intravascular hemolysis) or outside the blood vessels (extravascular hemolysis). Hemolytic Anemia) and neuraminidase Neuraminidase An enzyme that catalyzes the hydrolysis of alpha-2, 3, alpha-2, 6-, and alpha-2, 8-glycosidic linkages (at a decreasing rate, respectively) of terminal sialic residues in oligosaccharides, glycoproteins, glycolipids, colominic acid, and synthetic substrate. Antivirals for Influenza (NA). Influenza typically presents with a fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, myalgia Myalgia Painful sensation in the muscles. Ion Channel Myopathy, headache Headache The symptom of pain in the cranial region. It may be an isolated benign occurrence or manifestation of a wide variety of headache disorders. Brain Abscess, and symptoms of an upper respiratory infection Upper respiratory infection Rhinitis. Symptoms of gastroenteritis Gastroenteritis Gastroenteritis is inflammation of the stomach and intestines, commonly caused by infections from bacteria, viruses, or parasites. Transmission may be foodborne, fecal-oral, or through animal contact. Common clinical features include abdominal pain, diarrhea, vomiting, fever, and dehydration. Gastroenteritis may also commonly occur in children. Influenza is usually a self-limiting Self-Limiting Meningitis in Children condition, though viral or secondary bacterial pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia may complicate the disease. Management is generally supportive, although NA inhibitors can be helpful if initiated within 48 hours of infection. Prevention relies on the annual vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination of the public and practicing good hygiene.
Last updated: May 16, 2024
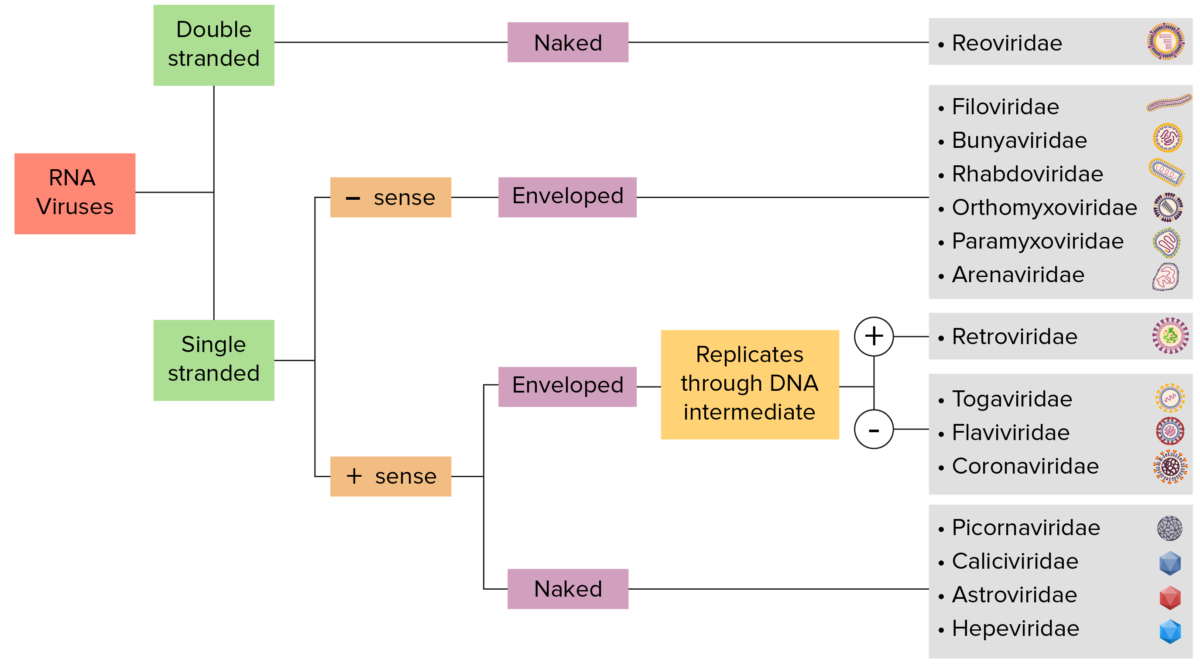
RNA virus identification:
Viruses can be classified in many ways. Most viruses, however, will have a genome formed by either DNA or RNA. RNA genome viruses can be further characterized by either a single- or double-stranded RNA. “Enveloped” viruses are covered by a thin coat of cell membrane (usually taken from the host cell). If the coat is absent, the viruses are called “naked” viruses. Viruses with single-stranded genomes are “positive-sense” viruses if the genome is directly employed as messenger RNA (mRNA), which is translated into proteins. “Negative-sense,” single-stranded viruses employ RNA dependent RNA polymerase, a viral enzyme, to transcribe their genome into messenger RNA.
The influenza virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology is a member of the Orthomyxoviridae family.
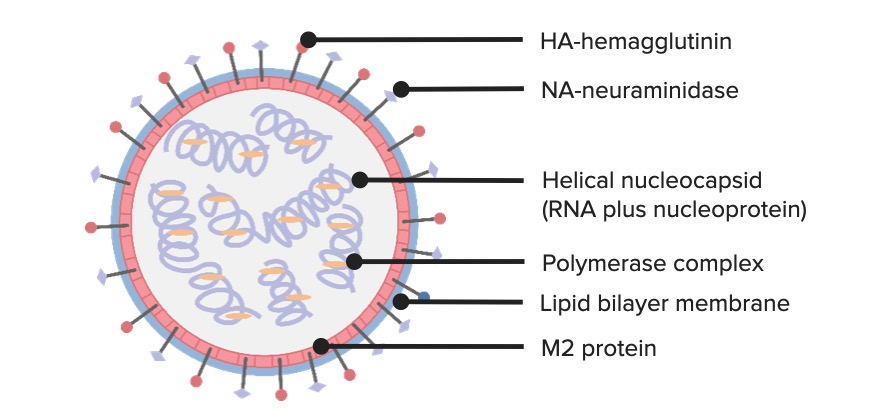
A diagram of the structure of the Influenza virus
Image by Lecturio. License: CC BY-NC-SA 4.0Influenza
viruses
Viruses
Minute infectious agents whose genomes are composed of DNA or RNA, but not both. They are characterized by a lack of independent metabolism and the inability to replicate outside living host cells.
Virology cause a febrile respiratory disease known as influenza.
There are 3 distinct clinically relevant species of the
virus
Virus
Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range.
Virology:
| Characteristics | Influenza A Influenza A Antivirals for Influenza | Influenza B | Influenza C |
|---|---|---|---|
| Natural hosts |
|
Humans only |
|
| Epidemiology | Antigenic shift and drift | Antigenic drift only | Antigenic drift only |
| Manifestations | Large epidemics and pandemics with significant mortality Mortality All deaths reported in a given population. Measures of Health Status | No pandemics; elderly and immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship | Mild disease without seasonality |
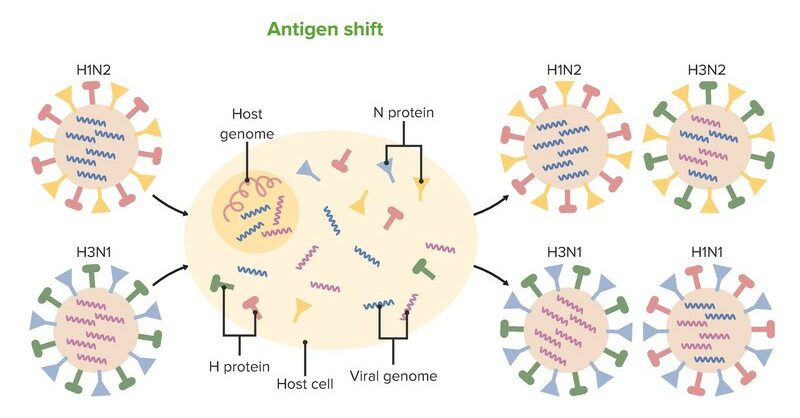
Antigenic shift:
Two or more different strains of a virus combine to form a new subtype that is radically different.
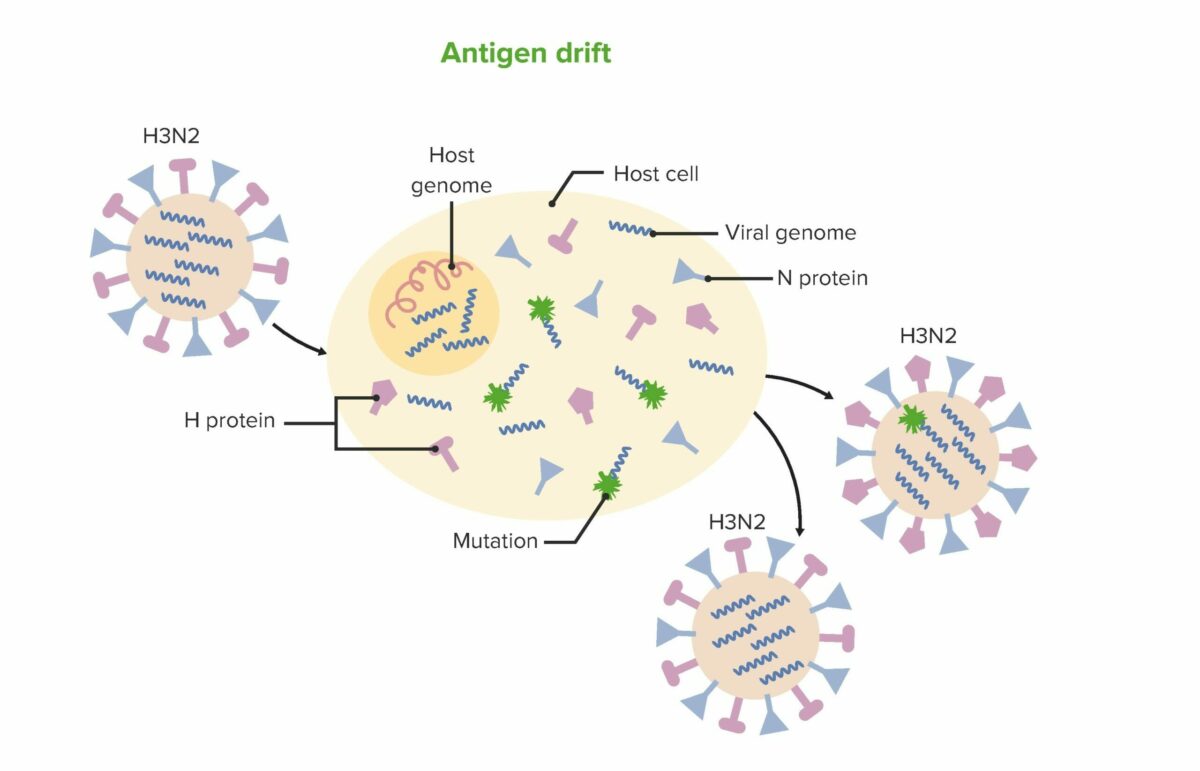
Antigenic drift:
Mutations accumulate in the viral genes that code for viral surface proteins resulting in new antigenic sites. Changes are generally minor.
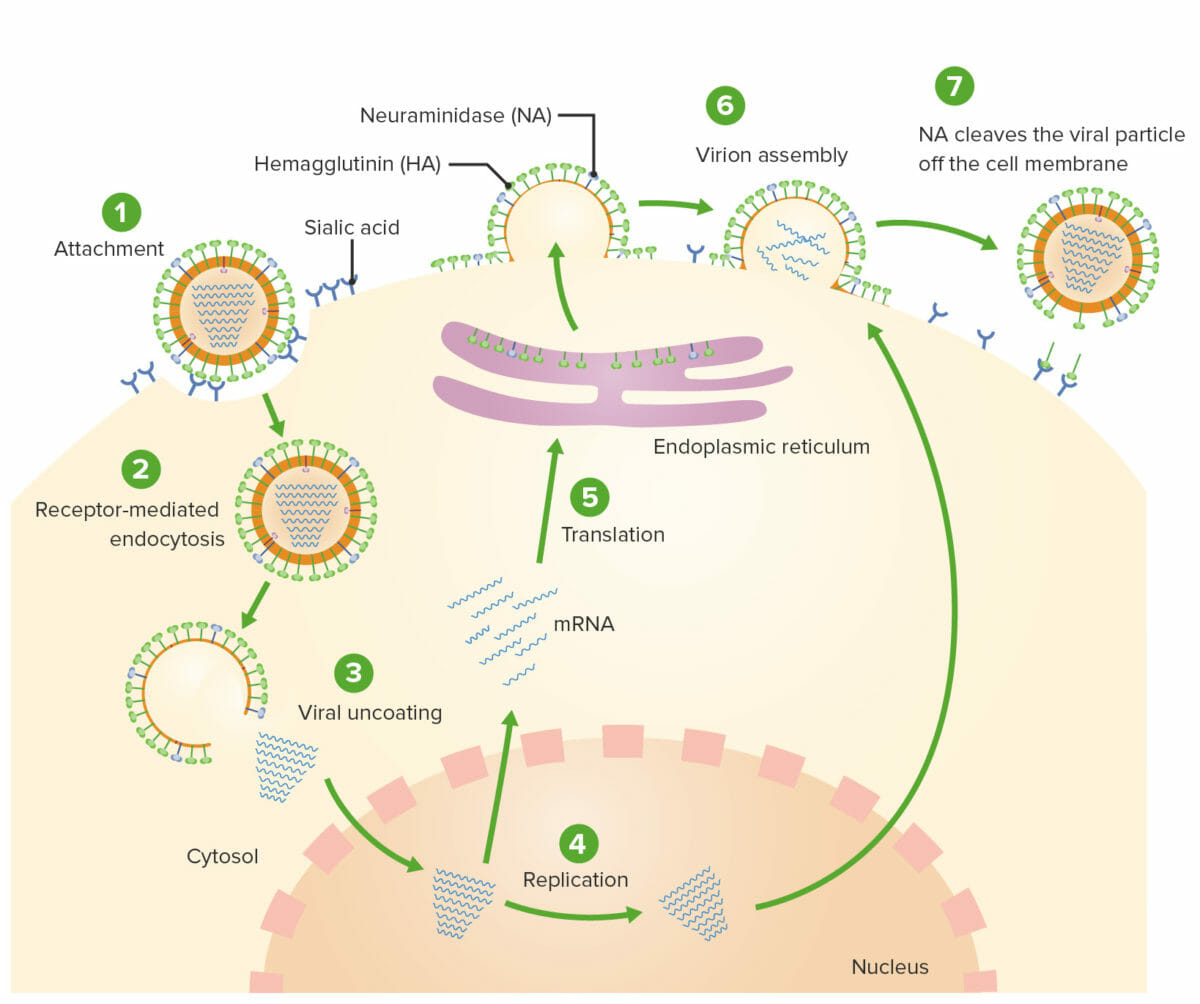
Influenza virus replication:
1: A viral particle attaches its hemagglutinin (HA) spikes to sialic acid-containing receptors on the surface of respiratory epithelial cells.
2: The viral particle is internalized via receptor-mediated endocytosis.
3: Once inside the cell, the M2 protein acts as an ion channel, allowing an influx of hydrogen particles, which results in uncoating of the virus.
4: The viral RNA then moves into the nucleus of the cell, where it is replicated and messenger RNA is synthesized.
5: The mRNA is then translated into new viral proteins using the cellular machinery.
6: Viral particles and newly replicated RNA are brought to the surface of the cell and assembled into virions.
7: As the new virus buds off of the respiratory epithelial cells, the hemagglutinin again binds to the sialic acid-containing receptors. The neuraminidase (NA) then cleaves the new viral particle off of the respiratory epithelial cell so it can go infect nearby cells.
Influenza A Influenza A Antivirals for Influenza and B create the same disease patterns.
Adults:
Children:
The diagnosis of influenza infection is typically made clinically; however, rapid diagnostic tests Diagnostic tests Diagnostic tests are important aspects in making a diagnosis. Some of the most important epidemiological values of diagnostic tests include sensitivity and specificity, false positives and false negatives, positive and negative predictive values, likelihood ratios, and pre-test and post-test probabilities. Epidemiological Values of Diagnostic Tests may be useful if the results will influence management.

Chest X-ray showing right lower lobe bacterial pneumonia
Image: “Chest radiography” by Department of Critical Care Medicine, University Hospital Thessaly, Larissa, Greece. License: CC BY 2.0
An AP supine radiograph on an intubated patient showing patchy consolidation in both lung fields, more prominent on the left due to hospital-acquired pneumonia
Image: “AP supine radiograph” by King Fahad Hospital, King Abdulaziz Medical City, Riyadh, Saudi Arabia. License: CC BY 2.0
Chest radiograph from a patient with viral pneumonia showing widespread bilateral interstitial infiltrates
Image: “Chest radiograph” by Department of Infectious Diseases, Leicester Royal Infirmary, Level 6 Windsor Building, Leicester, LE1 5WW, UK. License: CC BY 2.0The majority of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship require only supportive care and recover without complications. Antiviral Antiviral Antivirals for Hepatitis B medications are used in hospitalized or high-risk patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.