Colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy polyps are growths of mucosal tissue in the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy, the most common site of polyps in the GI tract. Polyps can be classified as neoplastic or nonneoplastic and may be associated with genetic syndromes. Hyperplastic polyps are nonneoplastic and are the most common type overall, whereas adenomas are the most common type of neoplastic polyp and have the potential to progress to cancer. For most people without hereditary syndromes, colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy cancer screening Screening Preoperative Care should begin at age 45 and in adolescence for those with the rare familial adenomatous polyposis Familial Adenomatous Polyposis Familial adenomatous polyposis (FAP) is an autosomal dominant inherited genetic disorder that presents with numerous adenomatous polyps in the colon. Familial adenomatous polyposis is the most common of the polyposis syndromes, which is a group of inherited or acquired conditions characterized by the growth of polyps in the GI tract, associated with other extracolonic features. Familial Adenomatous Polyposis ( FAP FAP Familial adenomatous polyposis (FAP) is an autosomal dominant inherited genetic disorder that presents with numerous adenomatous polyps in the colon. Familial adenomatous polyposis is the most common of the polyposis syndromes, which is a group of inherited or acquired conditions characterized by the growth of polyps in the GI tract, associated with other extracolonic features. Familial Adenomatous Polyposis) syndrome. Diagnosis is by biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma, and management includes frequent surveillance Surveillance Developmental Milestones and Normal Growth in people with adenomatous polyps Adenomatous polyps Benign neoplasms derived from glandular epithelium. Colorectal Cancer or screening Screening Preoperative Care every 10 years in the general population until age 75.
Last updated: Jan 16, 2024
Each syndrome occurs in < 1% of the population and accounts for 5%–10% of CRCs.
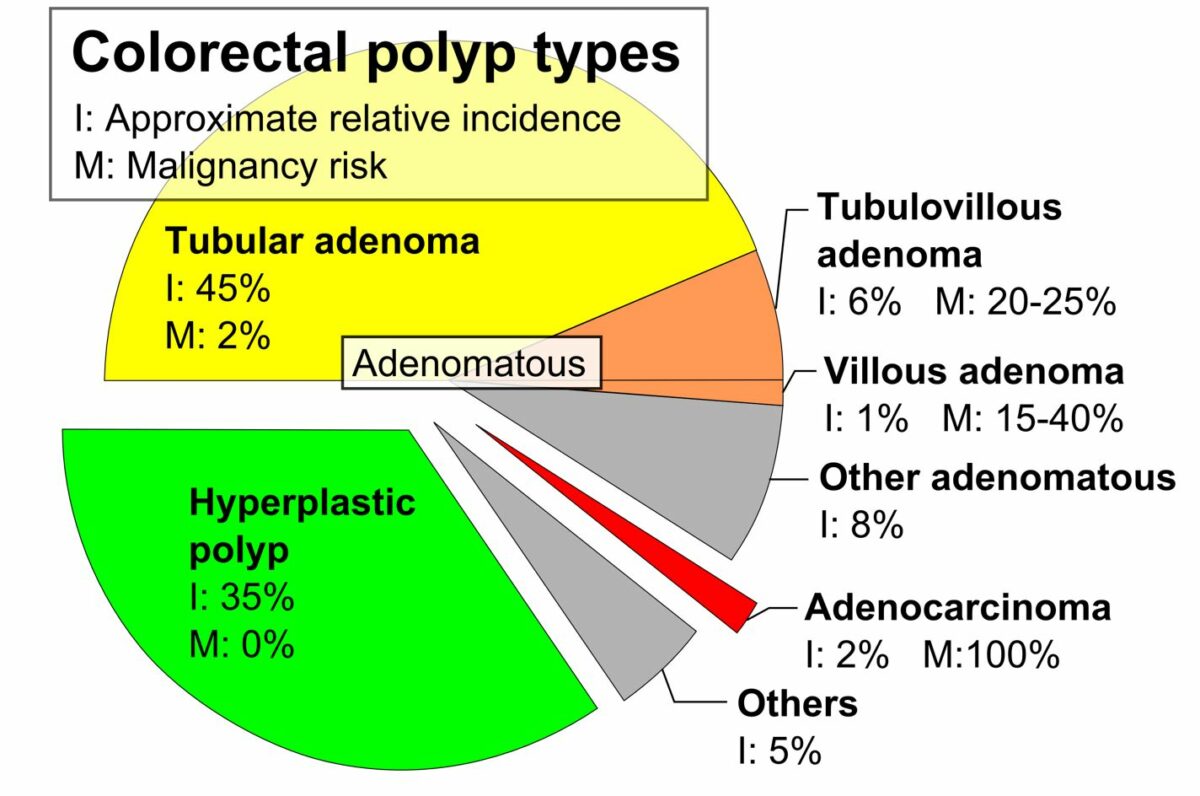
Colorectal polyp types, approximate relative incidence (I), and malignancy risk (M) (2019)
Image: “Pie chart of colorectal polyp etiologies” by Mikael Häggström. License: CC0 1.0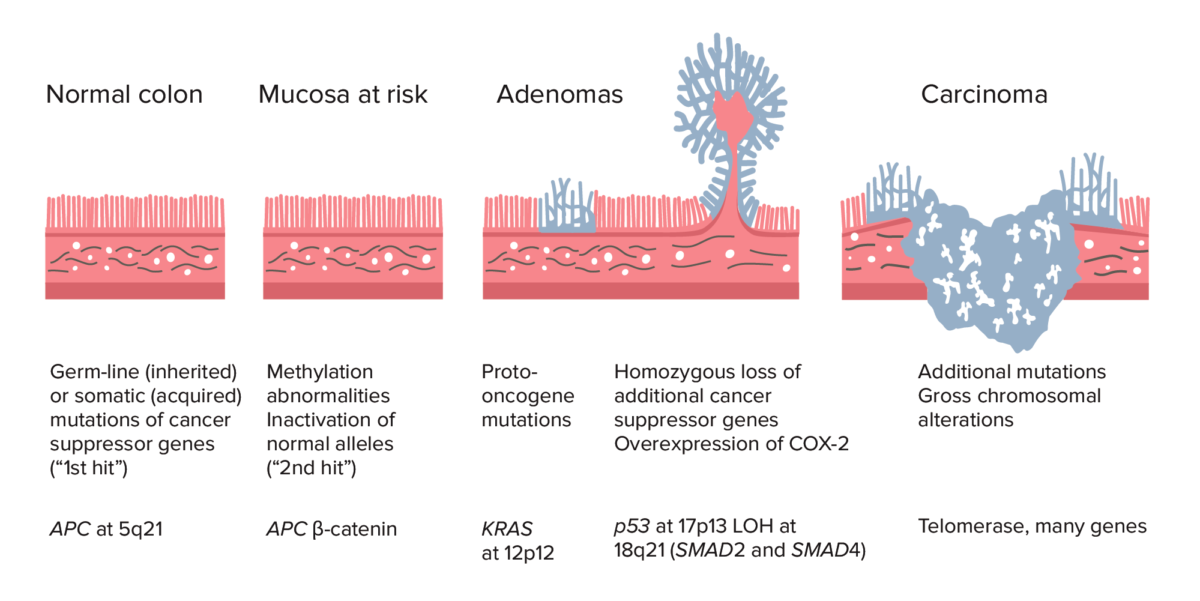
Adenoma–carcinoma sequence from normal colon to carcinoma:
Colorectal cancer (CRC) formation begins with APC gene mutation (inherited or acquired) and methylation abnormalities. Other changes can include KRAS gene mutation. Late in the process, p53 deletion, loss of heterozygosity (LOH) at 18q21 (involving SMAD2 and SMAD4), with overexpression of COX-2 can contribute to further growth and progression to cancer. The accumulation of mutations, rather than the timing of occurrence, is most crucial in carcinogenesis.
Most colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy polyps are asymptomatic and discovered on routine colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy cancer screening Screening Preoperative Care.
The definitive diagnosis and treatment of colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy polyps are achieved by endoscopic removal of the entire polyp.
Hyperplastic polyp of the rectum
Image: “Hyperplastic Polyp of the Rectum (14060044206)” by Ed Uthman. License: CC BY 2.0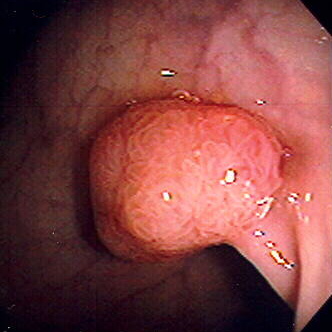
Colon polyp on a stalk (pedunculated)
Image: “Polyp” by Stephen Holland. License: 2.5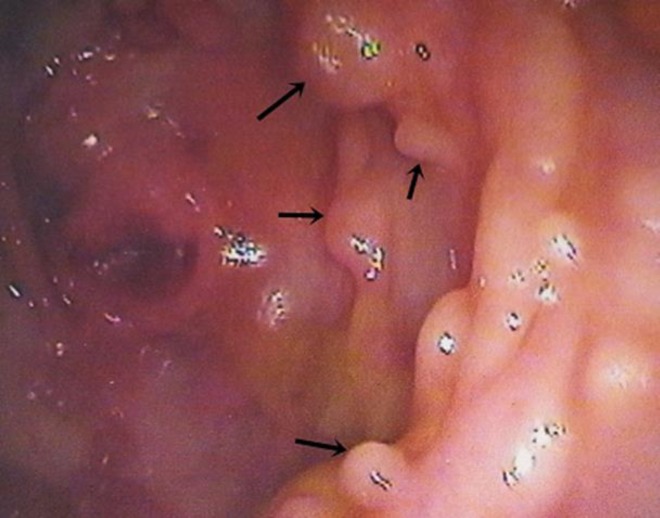
Multiple polyps in colon, ranging from 0.5 to 1 cm in diameter
Image: “Multiple polyps in colon” by Agrawal N, Santra T, Kar A, Guha P, Bar M, Adhikary A, Datta S. License: CC BY 3.0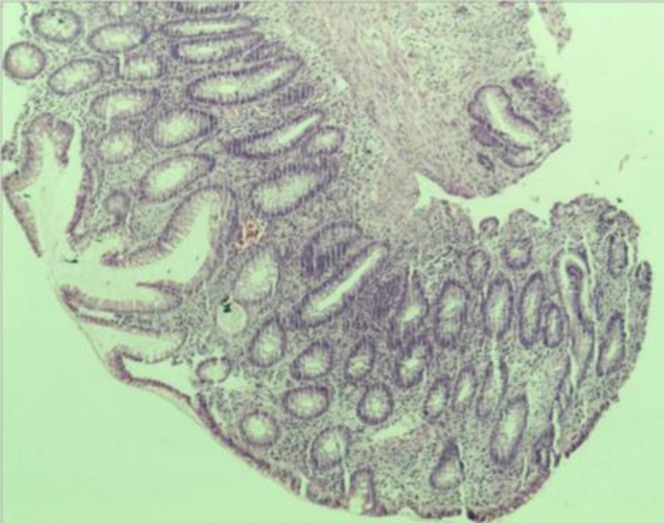
Biopsy from the sigmoid polyp revealing adenomatous polyp with no evidence of malignancy
Image: “Biopsy from sigmoid polyp revealing adenomatous polyp without any evidence of malignancy” by Agrawal N, Santra T, Kar A, Guha P, Bar M, Adhikary A, Datta S. License: CC BY 3.0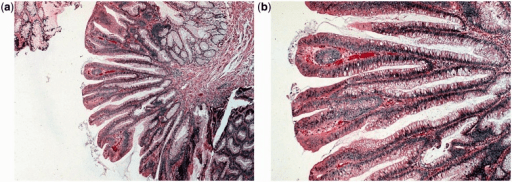
Villous adenoma: The histological appearance is of long finger-like projections.
a: low-power magnification view (H&E stain, 400x)
b: high-power magnification view (H&E stain, 2000x)
Tubular adenoma: The histological appearance is of branched tubular glands.
a: low-power magnification view (H&E stain, 400x)
b: high-power magnification view (H&E stain, 2000x)
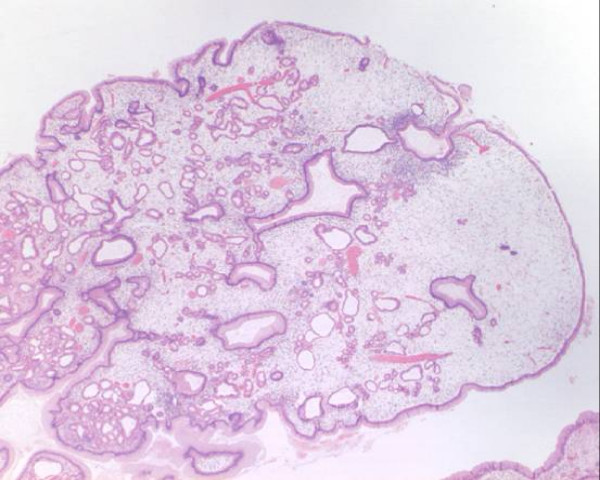
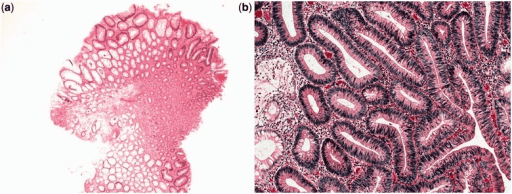
Histology of juvenile polyp showing characteristic cystically dilated glands:
Even at low power, the benign and non-neoplastic nature is supported by seeing only 1 layer of epithelial cells on the surface and lining the glandular spaces.

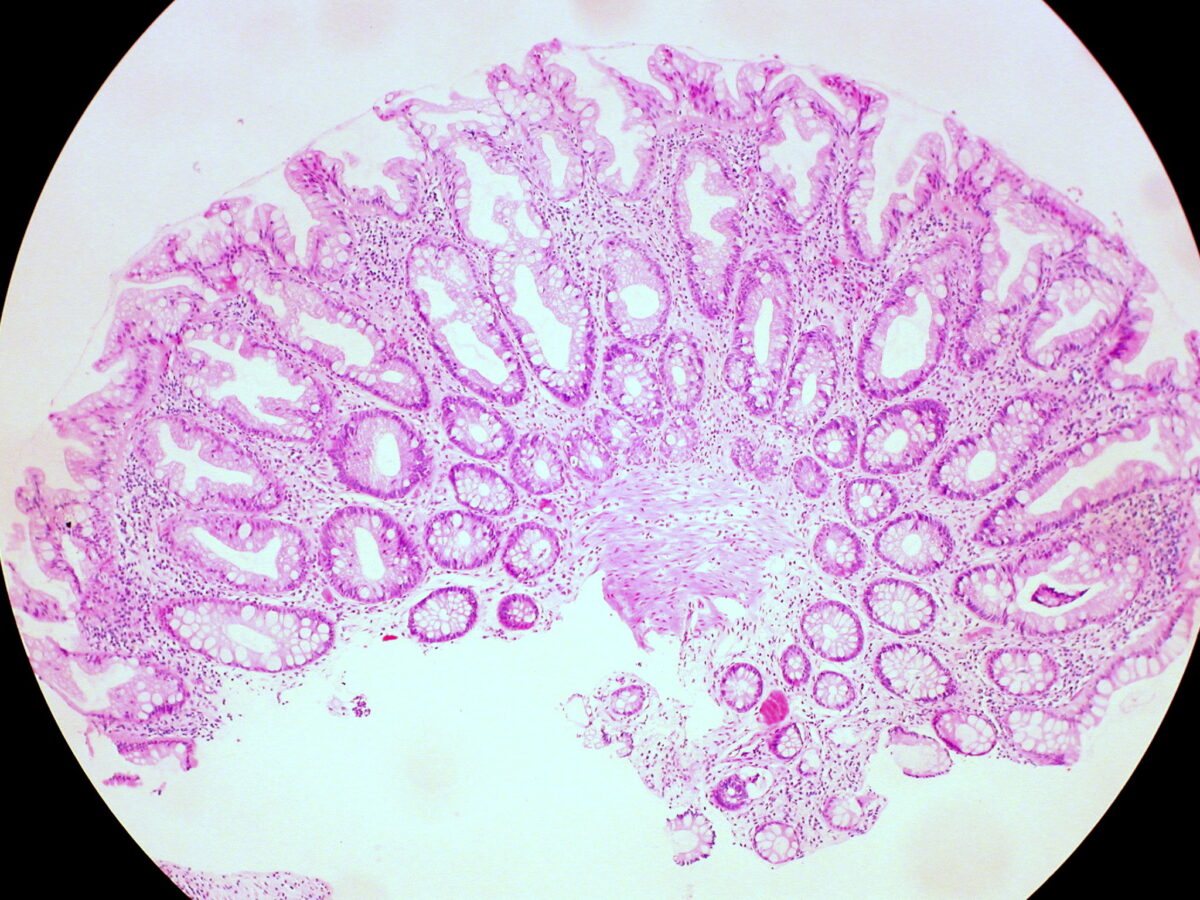
Tubulovillous polyp
Image: “Tubulovillous Polyp of the Colon 2” by Ed Uthman. License: Public Domain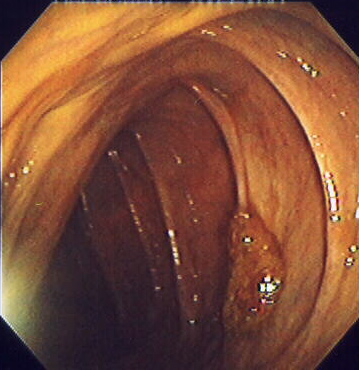
Sessile colon polyp seen on colonoscopy
Image: “Endomucosal resection 1” by Stephen Holland. License: 2.5Follow-up guidelines after colonoscopy Colonoscopy Endoscopic examination, therapy or surgery of the luminal surface of the colon. Colorectal Cancer Screening and polypectomy (based on 2020 Consensus Update by the U.S. Multi-Society Task Force on Colorectal Cancer Colorectal cancer Colorectal cancer (CRC) is the 2nd leading cause of cancer-related deaths in the United States. Colorectal cancer is a heterogeneous disease that arises from genetic and epigenetic abnormalities, with influence from environmental factors. Colorectal Cancer):
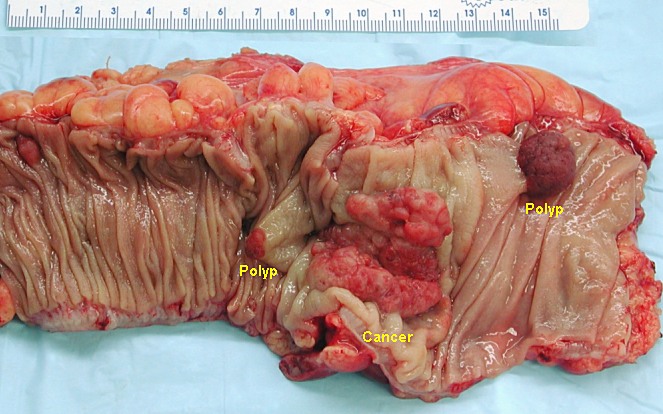
Segment of resected colon in the unfixed state containing an invasive colorectal carcinoma and 2 adenomatous polyps
Image: “Colon cancer” by Emmanuelm. License: CC BY 3.0