Hyperparathyroidism is a condition associated with elevated blood levels of parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy hormone (PTH). Depending on the pathogenesis of this condition, hyperparathyroidism can be defined as primary, secondary or tertiary. Primary hyperparathyroidism is an inherent disease of parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy glands associated with abnormal secretion Secretion Coagulation Studies of PTH. Secondary hyperparathyroidism results from abnormalities of calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes metabolism, which, if left untreated, can progress to tertiary hyperparathyroidism, which is associated with hypertrophy Hypertrophy General increase in bulk of a part or organ due to cell enlargement and accumulation of fluids and secretions, not due to tumor formation, nor to an increase in the number of cells (hyperplasia). Cellular Adaptation of the parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy gland and oversecretion of PTH even if the primary cause is eliminated. Diagnosis is based on biochemical parameters, which include serum PTH, calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes, and phosphate Phosphate Inorganic salts of phosphoric acid. Electrolytes levels as well as urinary calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes. Management relies mostly on surgical parathyroidectomy for primary and tertiary hyperparathyroidism. Management of secondary hyperparathyroidism is focused on treatment of the underlying disease.
Last updated: May 17, 2024
Hyperparathyroidism is a condition associated with elevated blood levels of parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy hormone (PTH).
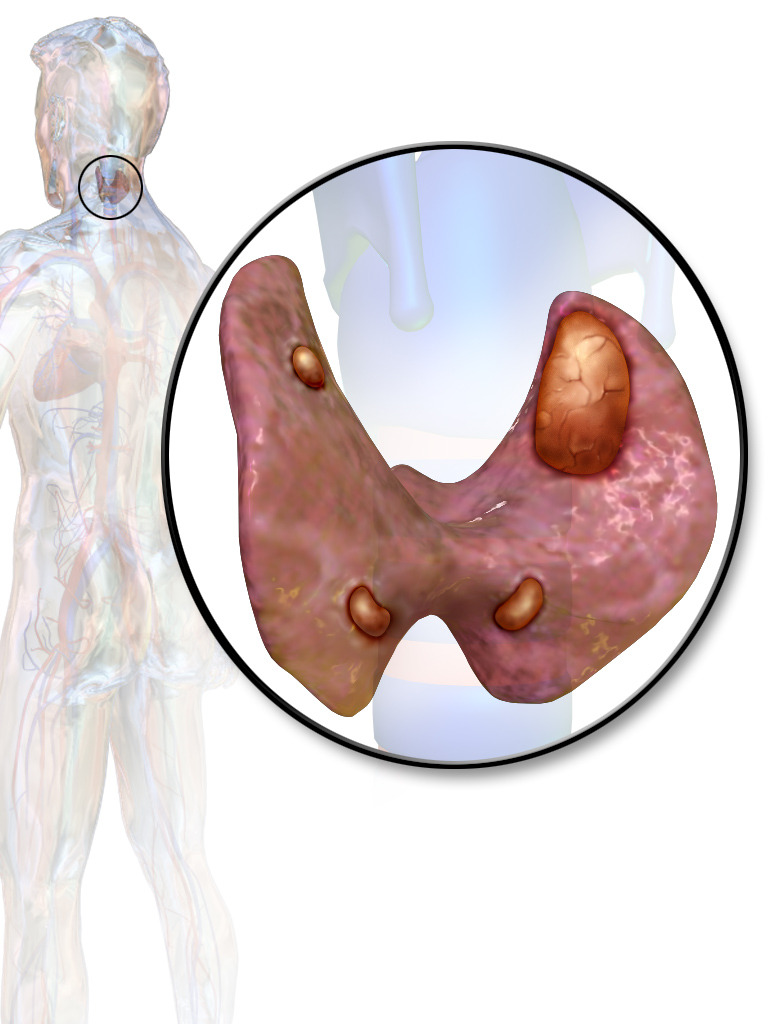
Parathyroid adenoma involving the left upper parathyroid gland
The other three glands are prominently displayed, but normal parathyroids are smaller than these appear to be (normal size, 3–5 mm; 30–60 mg each).
Primary hyperparathyroidism:
Secondary hyperparathyroidism:
Tertiary hyperparathyroidism:
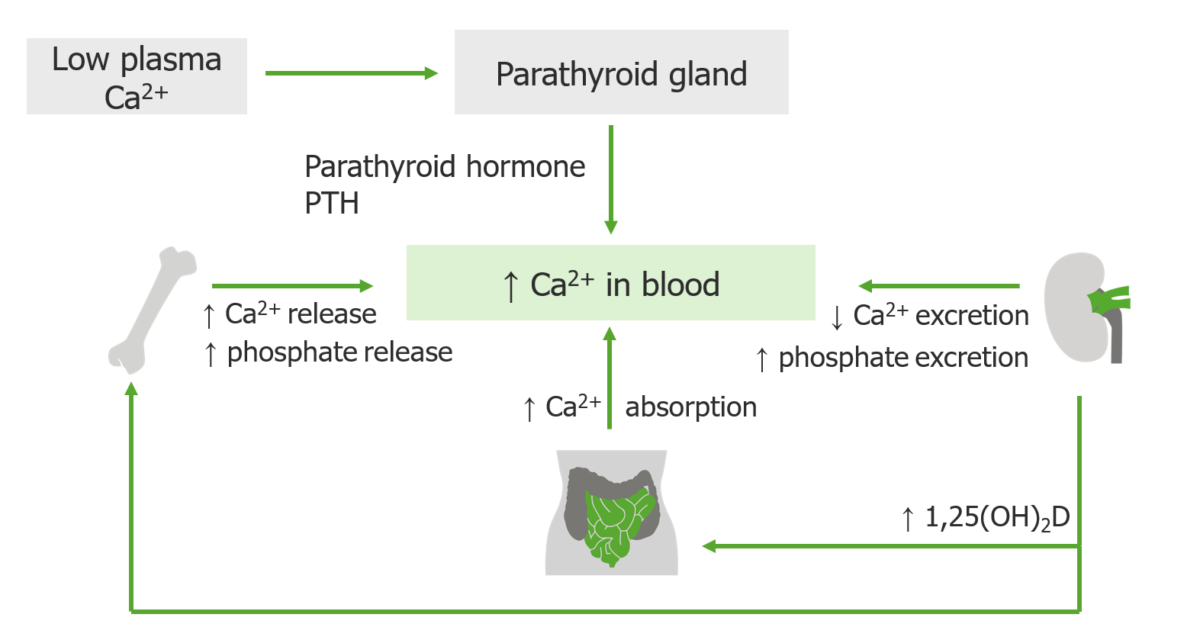
Parathyroid hormone has only one function: to correct hypocalcemia and maintain the serum level of calcium within narrow limits.
If the serum calcium is low, the four parathyroid glands secrete PTH, which is made and stored in the glands. When released, PTH works with and through vitamin D to restore the calcium level to normal.
Over 50% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are asymptomatic or present with nonspecific symptoms.
Mnemonic for PH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance: Stones, bones, groans, and moans:
Other symptoms include:
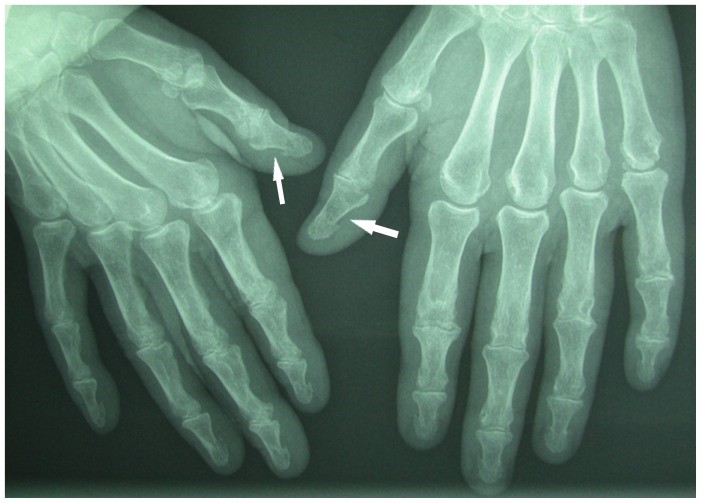
Hand radiograph in a 64-year-old woman with mild secondary hyperparathyroidism and a long history of knitting, showing subperiosteal bone resorption at both terminal thumb phalanges.
Bone resorption due to hyperparathyroidism is usually seen at the phalangeal tufts and the radial aspects of the middle phalanges of the second and the third fingers. The unusual location in the thumbs in this patient may be due to a combination of repetitive trauma and hyperparathyroidism.

X-rays of left lower limb in two orthogonal views showing osteitis fibrosa cystica presenting as a cystic/lytic bone space filled with brown fibrous tissue (arrows) known as a “brown tumor”:
Brown tumors are less commonly seen in hyperparathyroidism today because the disease is usually diagnosed at an earlier stage.
Medical management:
Surgery:
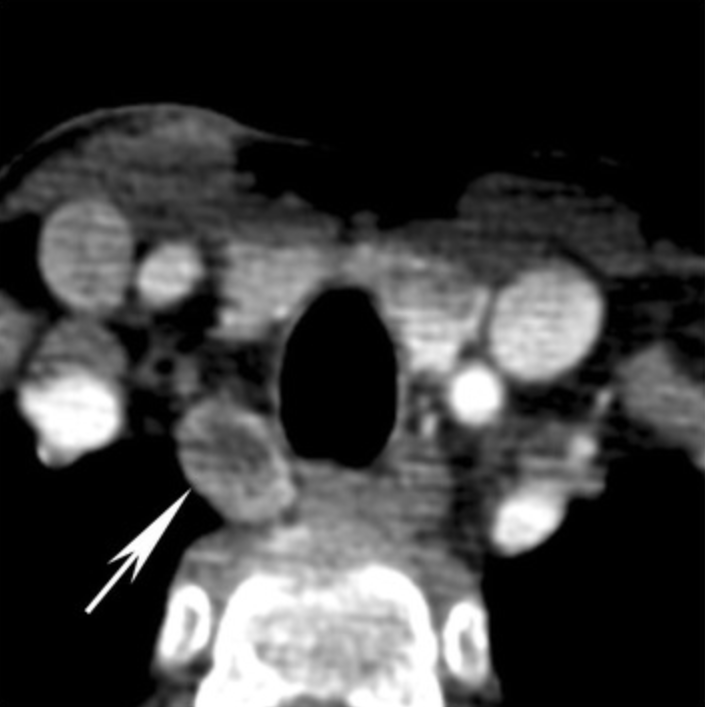
Parathyroid adenoma (arrow) with cystic change:
The tumor extends to the right tracheo-esophageal groove.
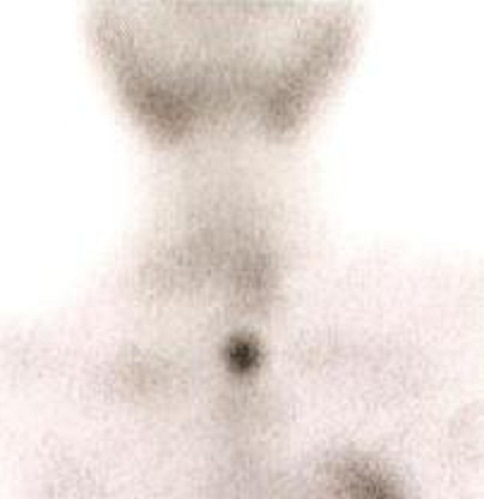
Sestamibi parathyroid scintigraphy revealed an increased focal uptake consistent with parathyroid adenoma at the left inferior pole of the thyroid gland
Image: “Serial pathologic fractures of five long bones on four separate occasions in a patient with primary hyperparathyroidism, challenges of management in a developing country: a case report” by Olatoke, S.A., et al. License: CC BY 2.0
a: Giant parathyroid adenoma following resection and fixation in formalin
b: Cross sections of the multiloculated mass
c: Low-power microscopic view of adenomatous cells at the top right portion of photograph, adjacent to pink thick fibrous tissue; a small cluster of compressed normal thyroid glandular tissue is in the left lower corner.
Medical management: