Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types, while seemingly inert, is an active, growing, and changing part of the human body, in addition to being the body's primary calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli. In the correct homeostatic conditions, bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types can remodel in response to damage, stress, or hormonal signaling ( parathyroid Parathyroid The parathyroid glands are 2 pairs of small endocrine glands found in close proximity to the thyroid gland. The superior parathyroid glands are lodged within the parenchyma of the upper poles of the right and left thyroid lobes; the inferior parathyroid glands are close to the inferior tips or poles of the lobes. Parathyroid Glands: Anatomy hormone and calcitonin Calcitonin A peptide hormone that lowers calcium concentration in the blood. In humans, it is released by thyroid cells and acts to decrease the formation and absorptive activity of osteoclasts. Its role in regulating plasma calcium is much greater in children and in certain diseases than in normal adults. Other Antiresorptive Drugs). Osteocytes Osteocytes Mature osteoblasts that have become embedded in the bone matrix. They occupy a small cavity, called lacuna, in the matrix and are connected to adjacent osteocytes via protoplasmic projections called canaliculi. Bones: Development and Ossification located deep in the bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types sense damage and signal bone-lining cells that will begin the process of remodeling. This process is vital not only for damage repair but also to adapt to a new environment and conditions.
Last updated: Sep 1, 2022
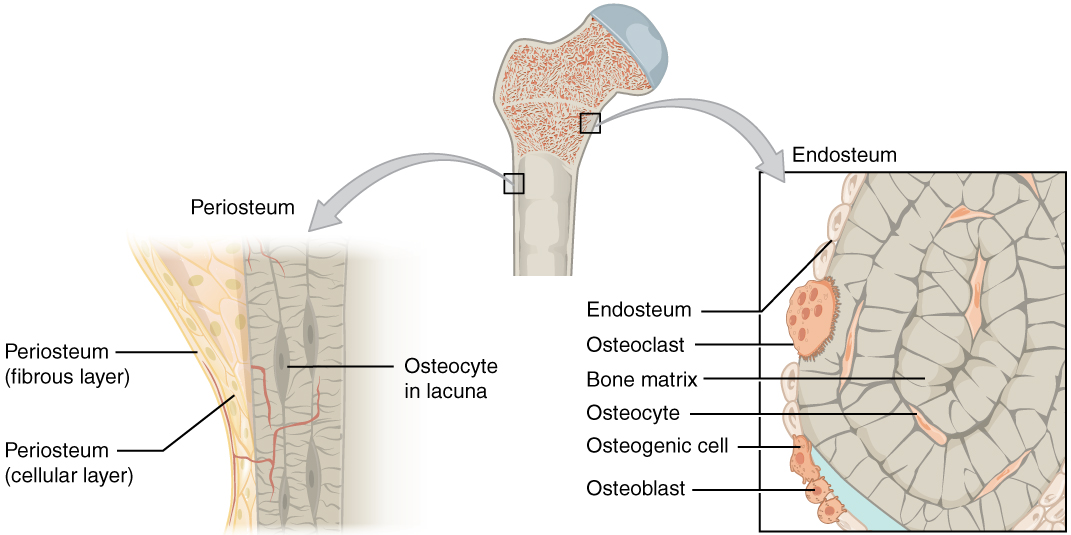
Bone anatomy:
Bones are covered in a layer called the periosteum, composed of fibrous and cellular layers. Below the periosteum is the endosteum, a complex architecture constructed on a mineral scaffold (the bony matrix) and composed of osteocytes, osteoclasts, and osteoblasts.
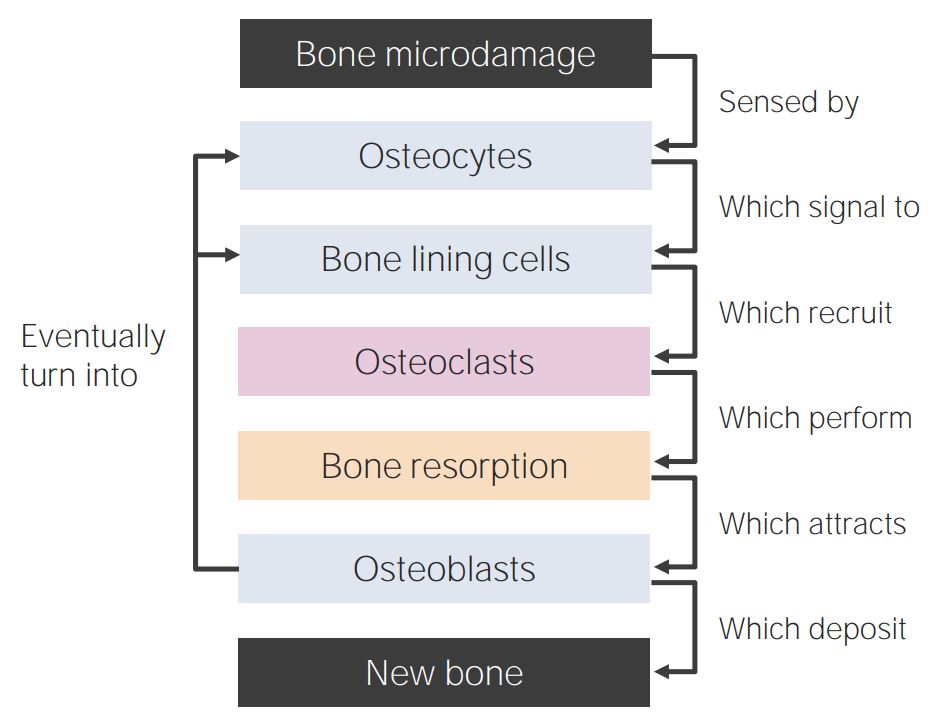
Bone-remodeling diagram
Bone remodeling begins with the osteocytes sensing microdamage. This process causes their apoptosis, which is concurrently sensed by bone-lining cells. These cells release chemoattractants, and osteoclasts group together in the damaged area to release calcium and phosphate. As soon as osteoclasts finish their work, osteoblasts begin recruiting the bone tissue. The process also traps some of the cells and forms a new lining by converting osteoblasts into osteocytes and bone-lining cells.
Signaling microdamage and activation:
Osteocytes at the site of microdamage undergo apoptosis.
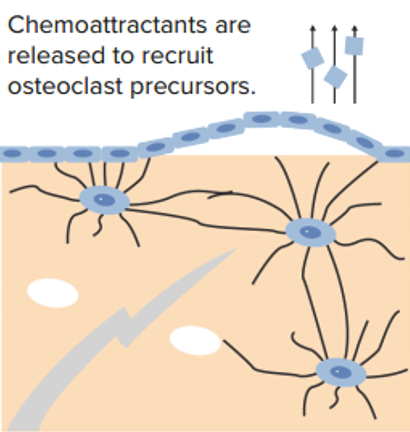
Bone-lining cells then digest underlying osteoid to expose mineral and lift off the surface.
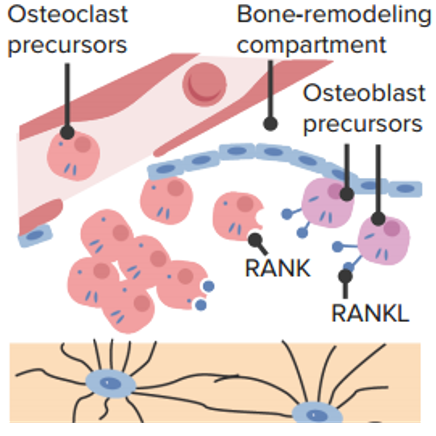
Osteoclast precursor recruitment:
Osteoclast precursors bind receptor activator of nuclear factor kappa B (RANK) ligand (RANKL) and coalesce to form an osteoclast.
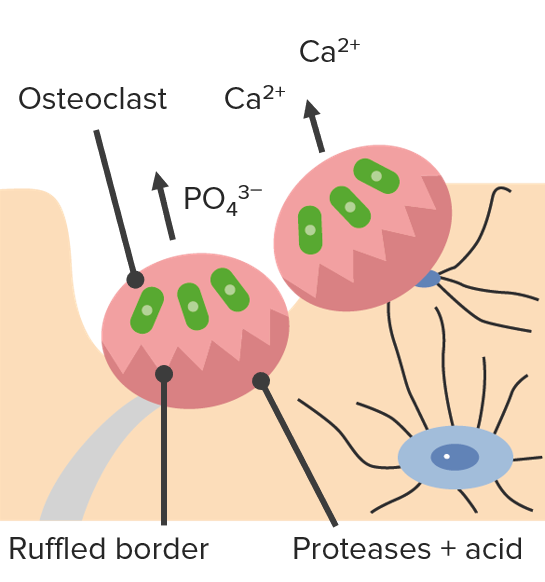
Absorption:
Osteoclasts digest minerals with acid, releasing Ca2+ and PO43–.
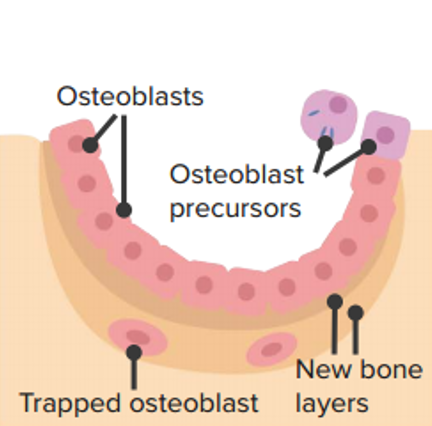
Deposition:
Osteoblast precursors become osteoblasts and lay down new osteoid. Osteoid mineralizes and forms new bone.
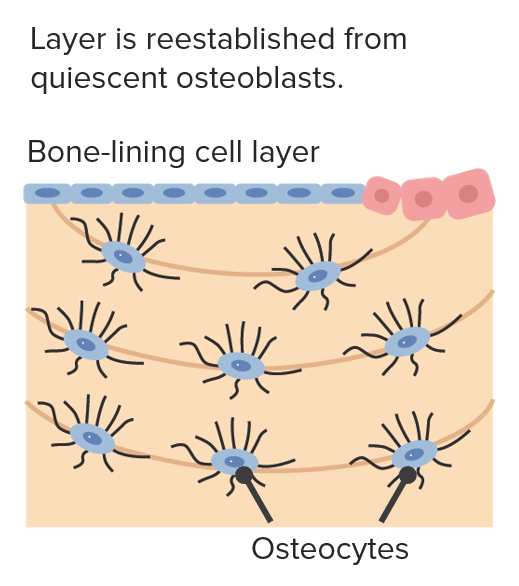
New bone:
Trapped osteoblasts become osteocytes and extend dendrites.