Bisphosphonates are pyrophosphate analogs most well-known for treating osteoporosis by preventing bone loss. Bisphosphonates end in the suffix “-dronate” or “-dronic acid" (e.g., alendronate, risedronate, pamidronate) and bind BIND Hyperbilirubinemia of the Newborn to hydroxyapatite crystals Hydroxyapatite crystals A group of compounds with the general formula m10(PO4)6(OH)2, where m is barium, strontium, or calcium. The compounds are the principal mineral in phosphorite deposits, biological tissue, human bones, and teeth. They are also used as an anticaking agent and polymer catalysts. Calcium Hemostasis and Bone Metabolism in bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types, inhibiting osteoclast-induced bone resorption Bone resorption Bone loss due to osteoclastic activity. Bones: Remodeling and Healing. Bisphosphonates are indicated for postmenopausal osteoporosis Postmenopausal osteoporosis Metabolic disorder associated with fractures of the femoral neck, vertebrae, and distal forearm. It occurs commonly in women within 15-20 years after menopause, and is caused by factors associated with menopause including estrogen deficiency. Osteoporosis, glucocorticoid-induced osteopenia Osteopenia Osteoporosis/ osteoporosis Osteoporosis Osteoporosis refers to a decrease in bone mass and density leading to an increased number of fractures. There are 2 forms of osteoporosis: primary, which is commonly postmenopausal or senile; and secondary, which is a manifestation of immobilization, underlying medical disorders, or long-term use of certain medications. Osteoporosis, and Paget disease of the bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types. Adverse effects include hypocalcemia Hypocalcemia Hypocalcemia, a serum calcium < 8.5 mg/dL, can result from various conditions. The causes may include hypoparathyroidism, drugs, disorders leading to vitamin D deficiency, and more. Calcium levels are regulated and affected by different elements such as dietary intake, parathyroid hormone (PTH), vitamin D, pH, and albumin. Presentation can range from an asymptomatic (mild deficiency) to a life-threatening condition (acute, significant deficiency). Hypocalcemia, hypophosphatemia Hypophosphatemia A condition of an abnormally low level of phosphates in the blood. Bartter Syndrome, avascular necrosis Avascular Necrosis Hip Fractures of the femur, and osteonecrosis of the jaw Jaw The jaw is made up of the mandible, which comprises the lower jaw, and the maxilla, which comprises the upper jaw. The mandible articulates with the temporal bone via the temporomandibular joint (TMJ). The 4 muscles of mastication produce the movements of the TMJ to ensure the efficient chewing of food. Jaw and Temporomandibular Joint: Anatomy. Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation include hypersensitivity reactions and esophageal disorders. Bisphosphonates may interact with aminoglycosides Aminoglycosides Aminoglycosides are a class of antibiotics including gentamicin, tobramycin, amikacin, neomycin, plazomicin, and streptomycin. The class binds the 30S ribosomal subunit to inhibit bacterial protein synthesis. Unlike other medications with a similar mechanism of action, aminoglycosides are bactericidal. Aminoglycosides, aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs), and proton pump Pump ACES and RUSH: Resuscitation Ultrasound Protocols inhibitors.
Last updated: Sep 1, 2022
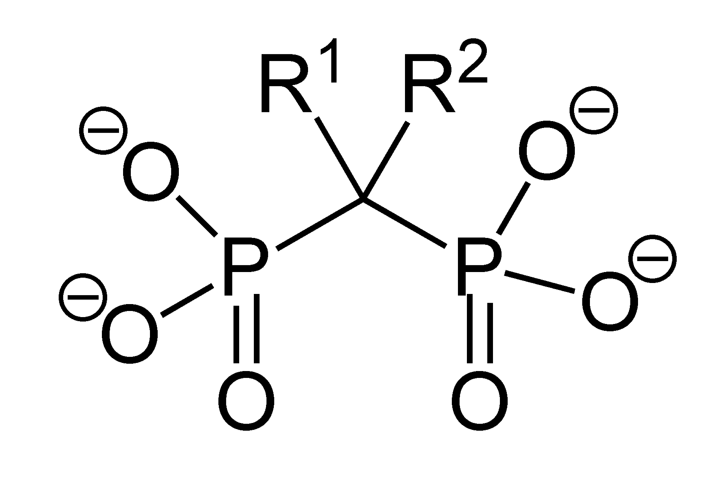
Structure of bisphosphonate:
The basic structure of bisphosphonate is centered around a common phosphorus-carbon-phosphorus bond, but the R groups may vary.
Bisphosphonates are classified by structure. Bisphosphonate compounds are either nitrogenous or nonnitrogenous. The nitrogenous subtype contains nitrogen Nitrogen An element with the atomic symbol n, atomic number 7, and atomic weight [14. 00643; 14. 00728]. Nitrogen exists as a diatomic gas and makes up about 78% of the earth’s atmosphere by volume. It is a constituent of proteins and nucleic acids and found in all living cells. Urea Cycle in the long chain (R2).
Bisphosphonates treat a number of conditions associated with bones:

A radiograph of avascular necrosis showing osteopenia, sclerosis, and rim calcification:
The classic sign of advanced disease is a crescent shape caused by subchondral bone accumulation and collapse of the articular surface.
| Medication | Classification | Half-life Half-Life The time it takes for a substance (drug, radioactive nuclide, or other) to lose half of its pharmacologic, physiologic, or radiologic activity. Pharmacokinetics and Pharmacodynamics elimination Elimination The initial damage and destruction of tumor cells by innate and adaptive immunity. Completion of the phase means no cancer growth. Cancer Immunotherapy | Indication |
|---|---|---|---|
| Alendronate | Nitrogenous | > 10 years |
|
| Risedronate | 480–561 hours (terminal) | ||
| Pamidronate | Approximately 28 hours | In addition to the above:
|
|
| Zoledronic acid | 146 hours (terminal) | ||
| Etidronate | Nonnitrogenous | 1–6 hours |
|
| Clodronate | 13 hours (terminal) |
|
|
| Tiludronate | 40–60 hours |