Paget disease of bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types (PDB), also known historically as osteitis deformans, is a focal disorder of bone metabolism Bone metabolism Bone is the primary storage site of calcium in the body; thus, bone metabolism plays a critical role in maintaining normal calcium levels. Bone metabolism (and thus calcium levels) are primarily regulated by 3 hormones, namely, calcitonin, parathyroid hormone (PTH), and vitamin D. Calcium Hemostasis and Bone Metabolism that affects about 2%–9% of people. Commonly affected areas include the skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy, spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy, pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 "hip" bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy, and long bones Long bones Length greater than width. Bones: Structure and Types of the lower extremity. The 2 main clinical manifestations of Paget disease are bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways and the consequences of bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types deformities, such as fractures, osteoarthritis Osteoarthritis Osteoarthritis (OA) is the most common form of arthritis, and is due to cartilage destruction and changes of the subchondral bone. The risk of developing this disorder increases with age, obesity, and repetitive joint use or trauma. Patients develop gradual joint pain, stiffness lasting < 30 minutes, and decreased range of motion. Osteoarthritis, or nerve impingement. The management includes bisphosphonates Bisphosphonates Bisphosphonates are pyrophosphate analogs most well-known for treating osteoporosis by preventing bone loss. Bisphosphonates end in the suffix "-dronate" or "-dronic acid" (e.g., alendronate, risedronate, pamidronate) and bind to hydroxyapatite crystals in bone, inhibiting osteoclast-induced bone resorption. Bisphosphonates, calcitonin Calcitonin A peptide hormone that lowers calcium concentration in the blood. In humans, it is released by thyroid cells and acts to decrease the formation and absorptive activity of osteoclasts. Its role in regulating plasma calcium is much greater in children and in certain diseases than in normal adults. Other Antiresorptive Drugs, and surgery for the management of fractures, deformities, and complications. The prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas for PDB is good, especially if treatment is started before major changes have occurred in the bones.
Last updated: Apr 27, 2025
Paget disease of bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types (PDB, also known as osteitis deformans) is a disorder of bone metabolism Bone metabolism Bone is the primary storage site of calcium in the body; thus, bone metabolism plays a critical role in maintaining normal calcium levels. Bone metabolism (and thus calcium levels) are primarily regulated by 3 hormones, namely, calcitonin, parathyroid hormone (PTH), and vitamin D. Calcium Hemostasis and Bone Metabolism affecting the aging skeleton.

Pagetic human femur (right side), posterior view
Left healthy femur from the same individual. Weight bearing on the irregularly thickened but structurally weak pagetic bone causes it to bow anteriorly.

Longitudinal section of a pagetic human femur from a 71-year-old woman. Note the irregularly thickened and focally porous cortex, the fibrotic marrow, and the curved shape.
Image: “Epidemiology and pathology of Paget’s disease of bone – a review” by Wiener Medizinische Wochenschrift. License: CC BY 4.0.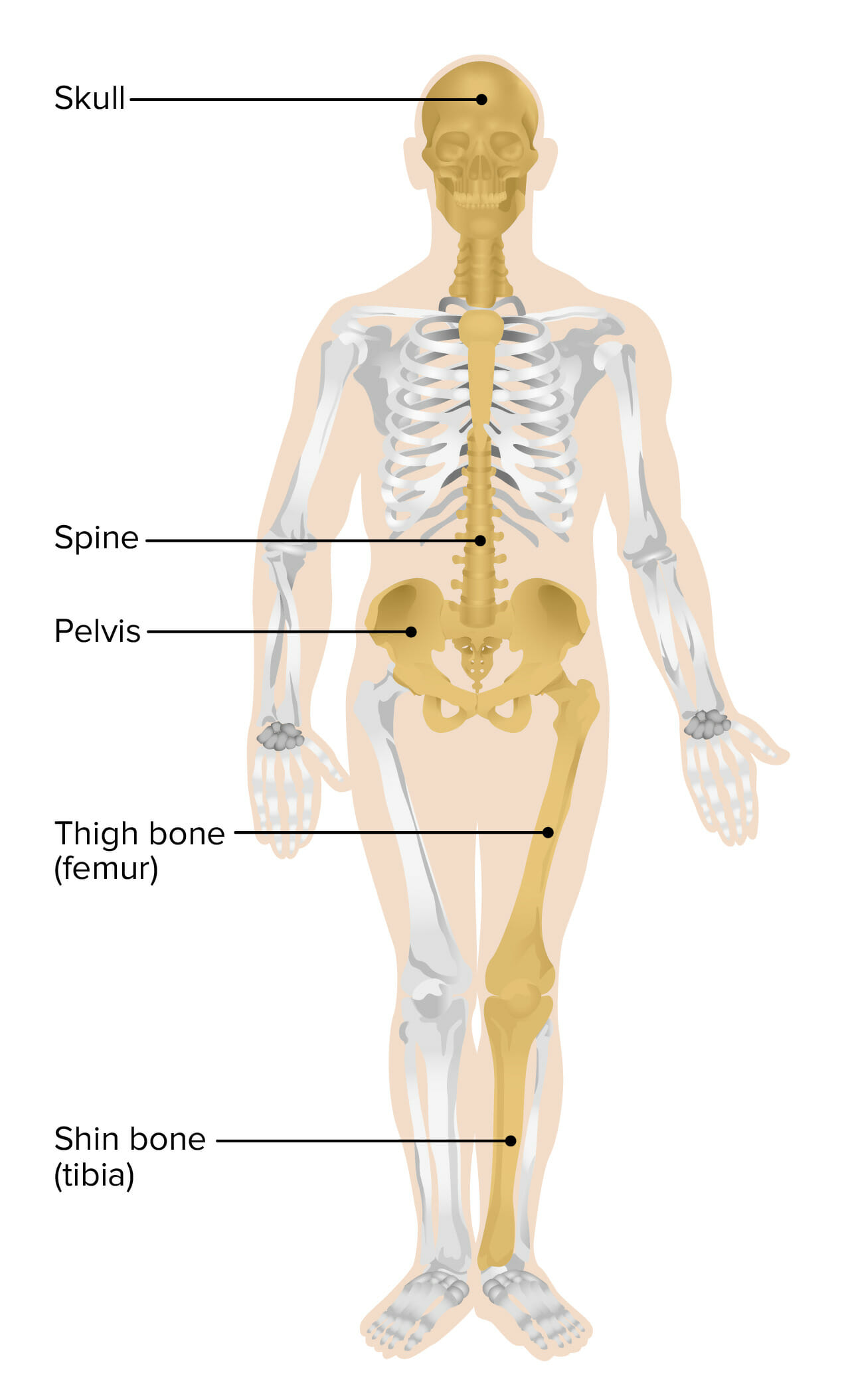
Most common sites involved in Paget disease of bone
Image by Lecturio.Over 70% of cases are asymptomatic.
Sites involved rarely change over a patient’s lifetime.
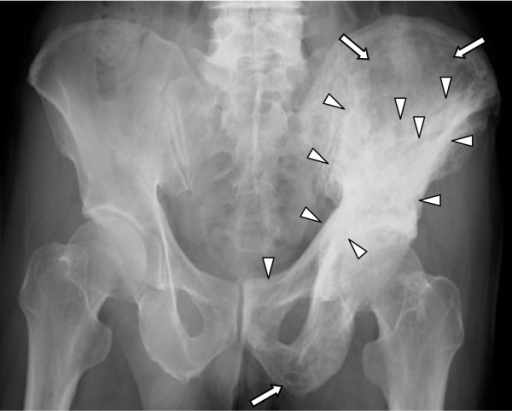
X-ray showing osteolytic (full arrows) and sclerotic (arrow heads) pagetic changes in the left acetabulum, half of the ilium, and the pubic bone
Image: “Five-year follow-up of Japanese patients with Paget’s disease of the bone after treatment with low-dose oral alendronate: a case series” by Iba K, Takada J, Wada T, Yamashita T. License: CC BY 2.0.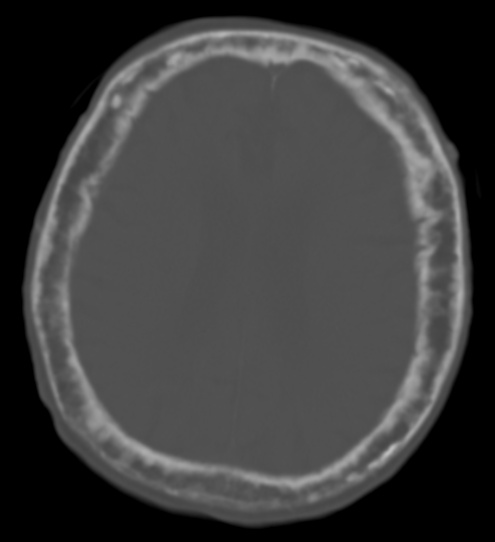
Paget’s disease of the calvarium incidentally noted on a CT scan
The calvarium is markedly thickened with a widened diploic space and ill-defined sclerotic and lucent areas throughout. The cortex is thickened and irregular. The focally thickened areas correspond to the “cotton wool spots” seen on plain films of the head.