The branchial arches, also known as pharyngeal or visceral arches, are embryonic structures seen in the development of vertebrates that serve as precursors for many structures of the face, neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess, and head. These arches are composed of a central core of mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation, which is covered externally by ectoderm Ectoderm The outer of the three germ layers of an embryo. Gastrulation and Neurulation and internally by endoderm Endoderm The inner of the three germ layers of an embryo. Gastrulation and Neurulation. Indentations between arches are known as the pharyngeal clefts, or grooves, externally and the pharyngeal pouches internally. Each pharyngeal arch contains cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology and muscular components, which are supplied by a cranial nerve (derived from neural crest cells Neural crest cells Gastrulation and Neurulation), and an artery, known as a pharyngeal aortic arch Aortic arch Mediastinum and Great Vessels: Anatomy. Some of these aortic arches go on to form the great vessels near the heart.
Last updated: Oct 30, 2023
The morula Morula An early embryo that is a compact mass of about 16 blastomeres. It resembles a cluster of mulberries with two types of cells, outer cells and inner cells. Morula is the stage before blastula in non-mammalian animals or a blastocyst in mammals. Fertilization and First Week (ball of cells) undergoes a process called blastulation, in which a cavity begins to form. The cells then begin differentiating into outer and inner cell masses.

Progression of early human development from fertilization through the blastocyst stage:
During these stages, the embryo is surrounded by a layer of extracellular matrix known as the zona pellucida.
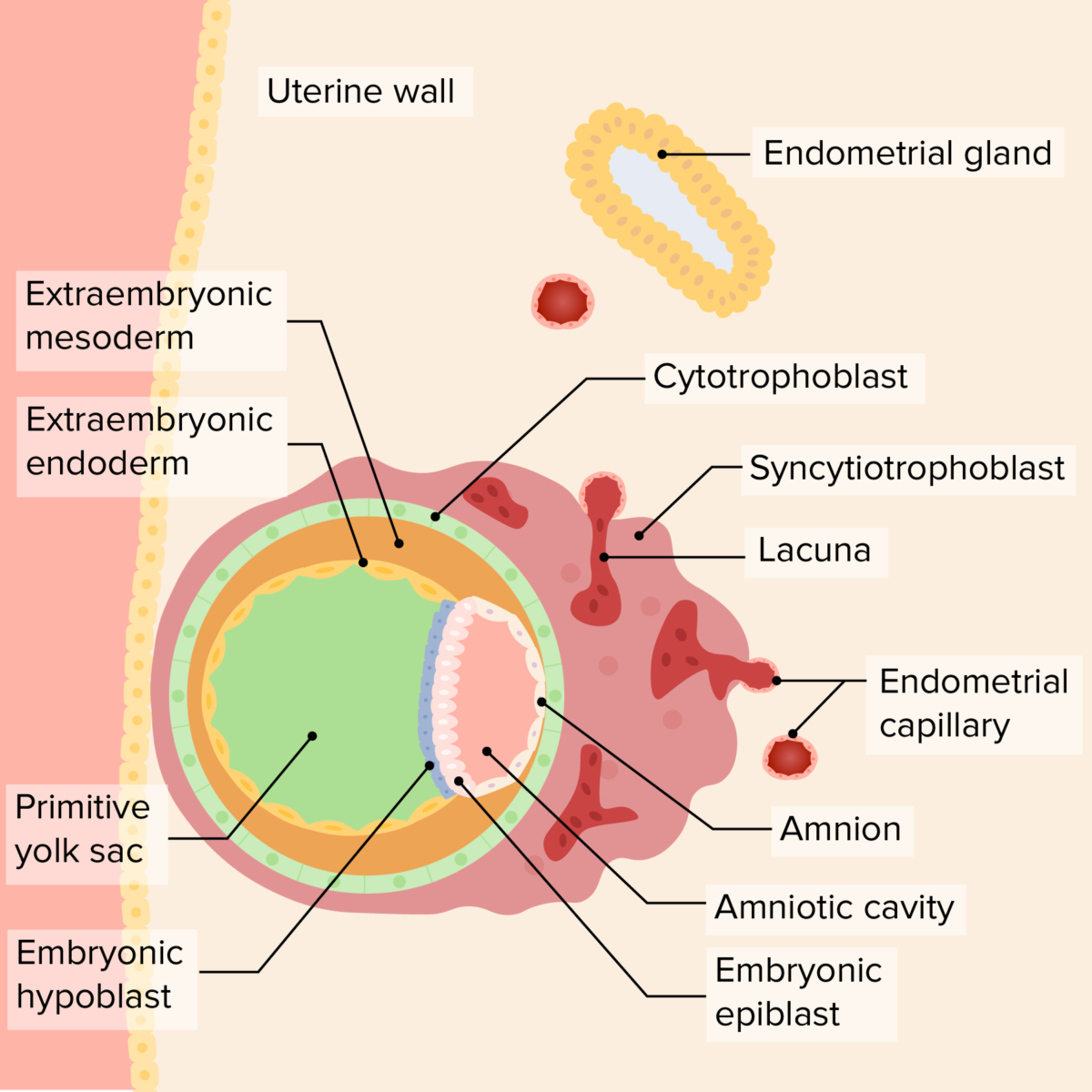
Relationship of the bilaminar disk, yolk sac, and amniotic cavity in the early embryo
Image by Lecturio. License: CC BY-NC-SA 4.0The bilaminar disk undergoes a process called gastrulation Gastrulation Both gastrulation and neurulation are critical events that occur during the 3rd week of embryonic development. Gastrulation is the process by which the bilaminar disc differentiates into a trilaminar disc, made up of the 3 primary germ layers: the ectoderm, mesoderm, and endoderm. Gastrulation and Neurulation to form the trilaminar disc Trilaminar disc Gastrulation and Neurulation. Cells from the epiblast Epiblast Embryoblast and Trophoblast Development layer migrate downward, replacing the hypoblast Hypoblast Embryoblast and Trophoblast Development ( endoderm Endoderm The inner of the three germ layers of an embryo. Gastrulation and Neurulation) and creating a 3rd layer in between ( mesoderm Mesoderm The middle germ layer of an embryo derived from three paired mesenchymal aggregates along the neural tube. Gastrulation and Neurulation).
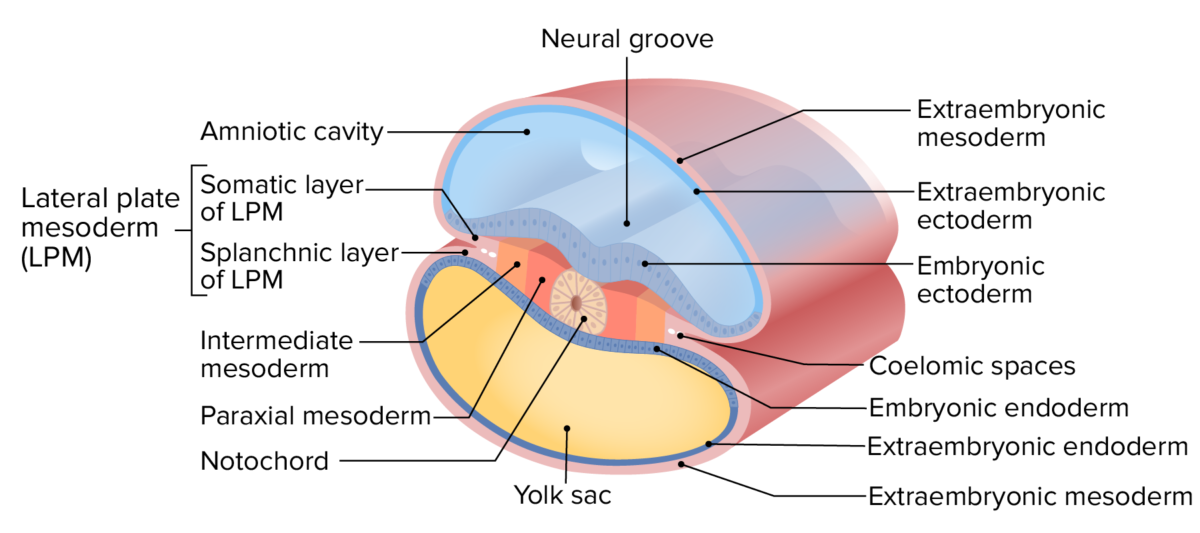
Layers of the trilaminar disc
Image by Lecturio.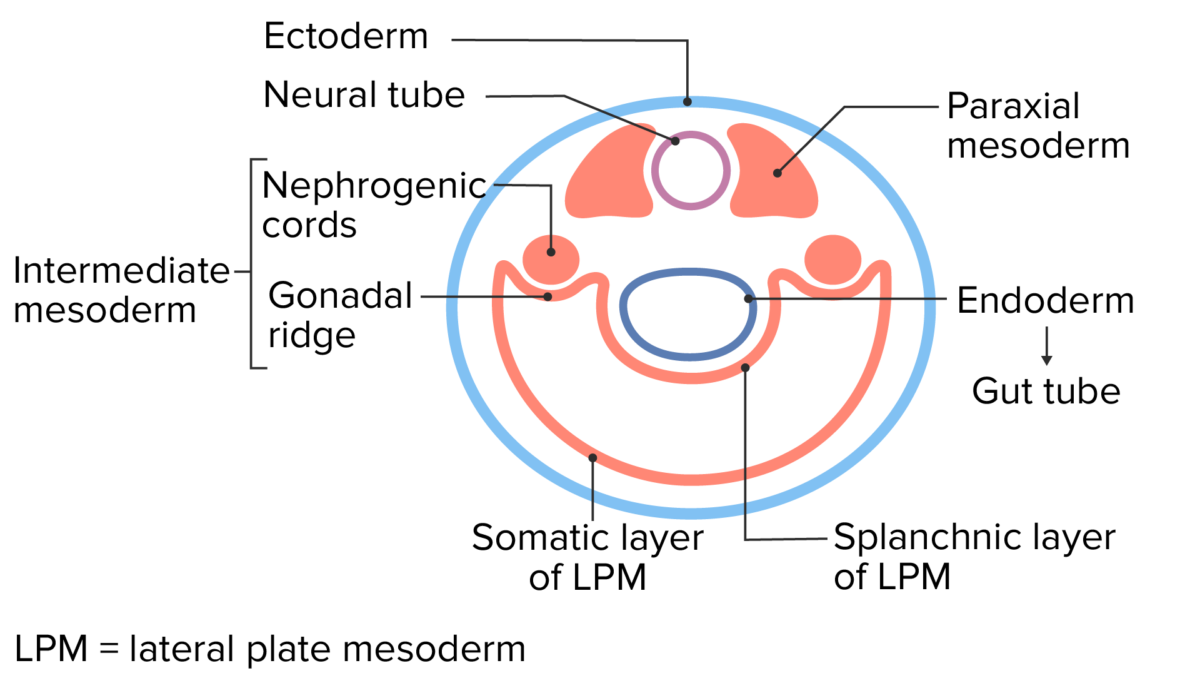
Cross-sectional view of the early embryo after it has undergone lateral folding
Image by Lecturio.The branchial (meaning “gills”) apparatus is also known as the pharyngeal apparatus in humans.
Development of the pharyngeal apparatus from the 3 germ layers
Image by Lecturio.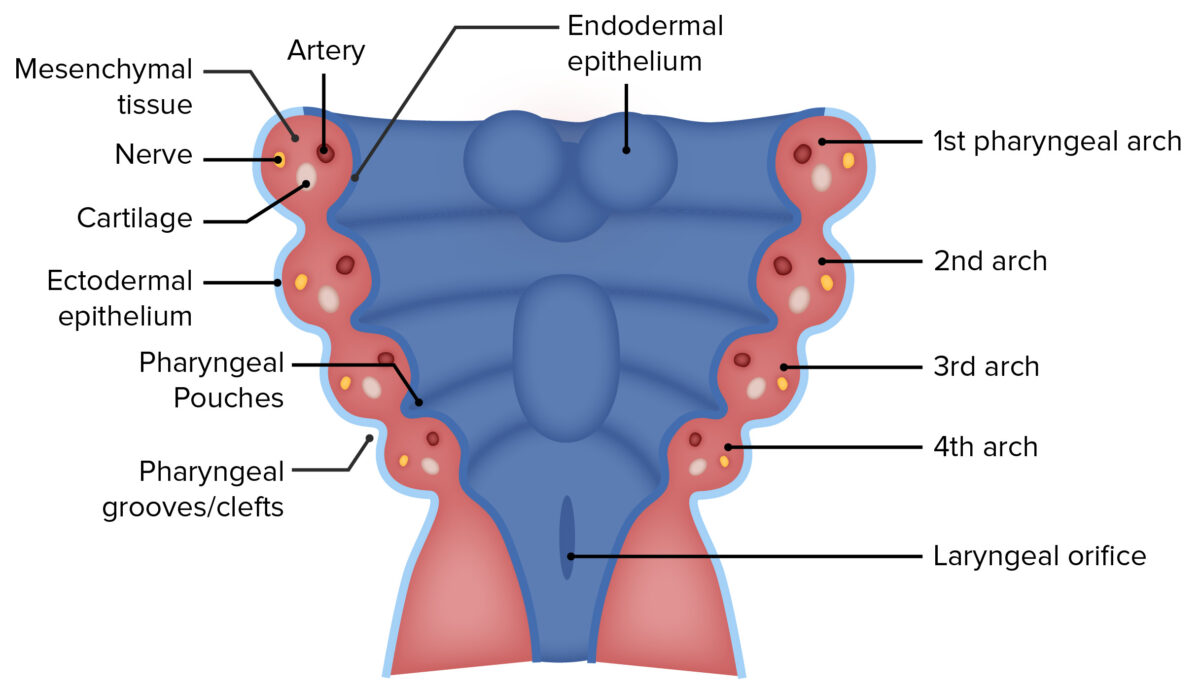
The branchial apparatus shown in cross section:
View is from the back (dorsal side) looking down.
Image by Lecturio.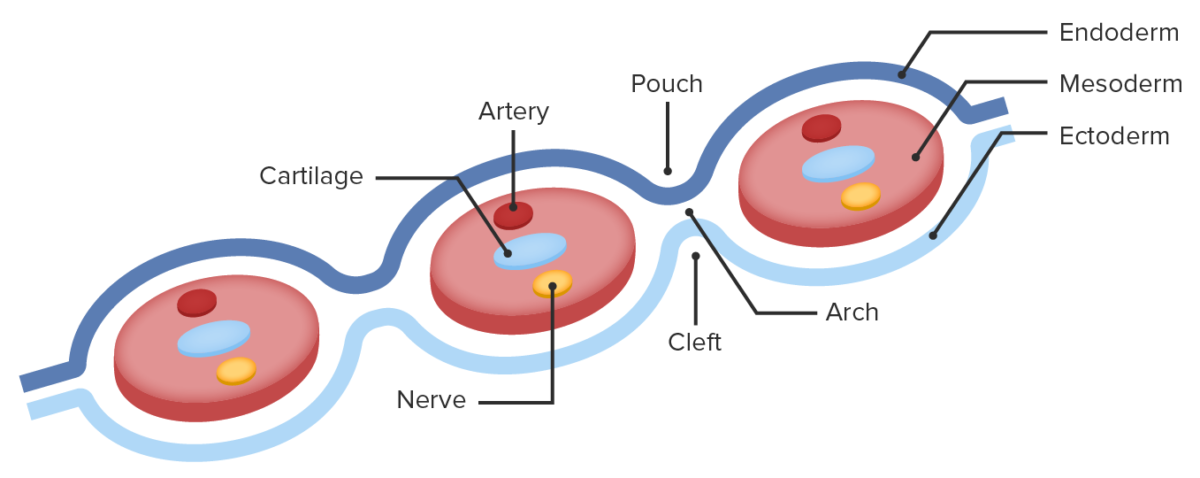
A side of the branchial apparatus in cross section, demonstrating the 3 germ layers, pharyngeal pouches, and clefts.
Image by Lecturio.The pharyngeal arches develop into key components of the head and neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess.
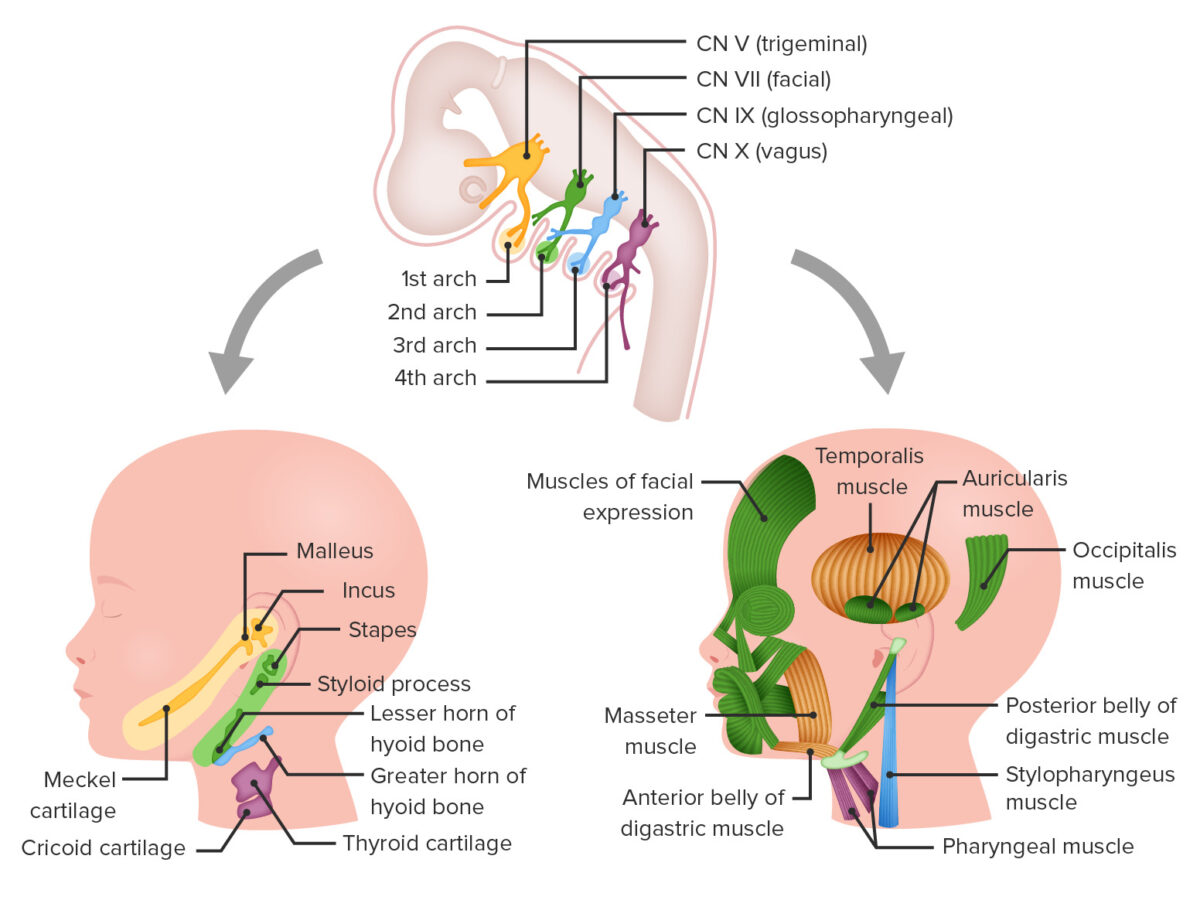
Derivatives of the pharyngeal arches and their associated cranial nerves (CNs)
Image by Lecturio.| Arch | Cartilage Cartilage Cartilage is a type of connective tissue derived from embryonic mesenchyme that is responsible for structural support, resilience, and the smoothness of physical actions. Perichondrium (connective tissue membrane surrounding cartilage) compensates for the absence of vasculature in cartilage by providing nutrition and support. Cartilage: Histology element | Musculature | Nerve |
|---|---|---|---|
| 1st |
|
|
CN V: mandibular branch of the trigeminal nerve Trigeminal nerve The 5th and largest cranial nerve. The trigeminal nerve is a mixed motor and sensory nerve. The larger sensory part forms the ophthalmic, mandibular, and maxillary nerves which carry afferents sensitive to external or internal stimuli from the skin, muscles, and joints of the face and mouth and from the teeth. Most of these fibers originate from cells of the trigeminal ganglion and project to the trigeminal nucleus of the brain stem. The smaller motor part arises from the brain stem trigeminal motor nucleus and innervates the muscles of mastication. The 12 Cranial Nerves: Overview and Functions |
| 2nd |
|
|
CN VII: facial nerve Facial nerve The 7th cranial nerve. The facial nerve has two parts, the larger motor root which may be called the facial nerve proper, and the smaller intermediate or sensory root. Together they provide efferent innervation to the muscles of facial expression and to the lacrimal and salivary glands, and convey afferent information for taste from the anterior two-thirds of the tongue and for touch from the external ear. The 12 Cranial Nerves: Overview and Functions |
| 3rd | Greater horn of the hyoid bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types | Stylopharyngeus muscle | CN IX: glossopharyngeal nerve Glossopharyngeal nerve The 9th cranial nerve. The glossopharyngeal nerve is a mixed motor and sensory nerve; it conveys somatic and autonomic efferents as well as general, special, and visceral afferents. Among the connections are motor fibers to the stylopharyngeus muscle, parasympathetic fibers to the parotid glands, general and taste afferents from the posterior third of the tongue, the nasopharynx, and the palate, and afferents from baroreceptors and chemoreceptor cells of the carotid sinus. Pharynx: Anatomy |
| 4th/6th |
|
|
CN X:
vagus nerve
Vagus nerve
The 10th cranial nerve. The vagus is a mixed nerve which contains somatic afferents (from skin in back of the ear and the external auditory meatus), visceral afferents (from the pharynx, larynx, thorax, and abdomen), parasympathetic efferents (to the thorax and abdomen), and efferents to striated muscle (of the larynx and pharynx).
Pharynx: Anatomy
|
Each branchial arch has its own pair of branchial arch arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology; there are 5 aortic arches in humans.
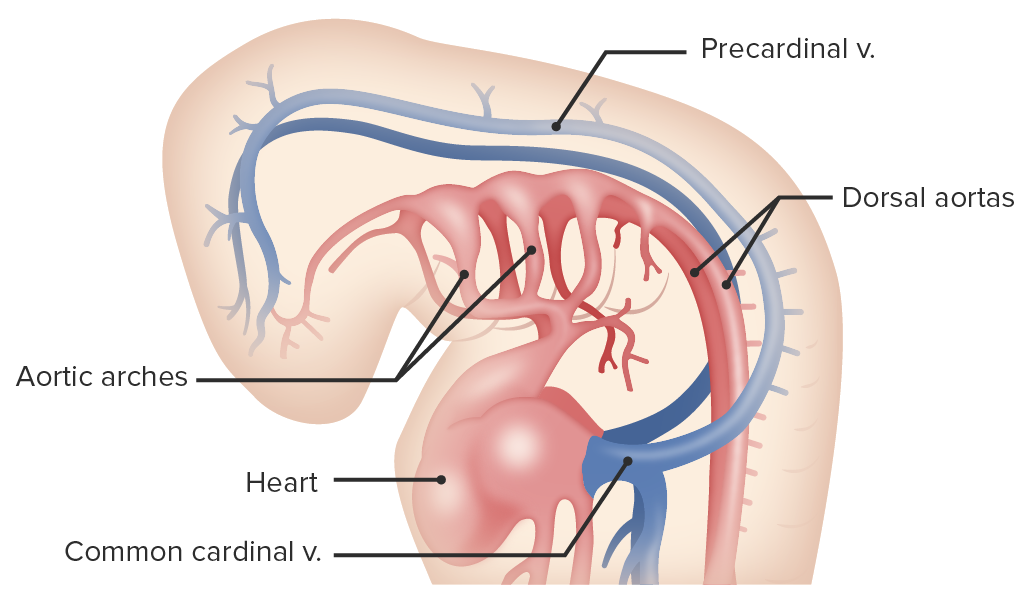
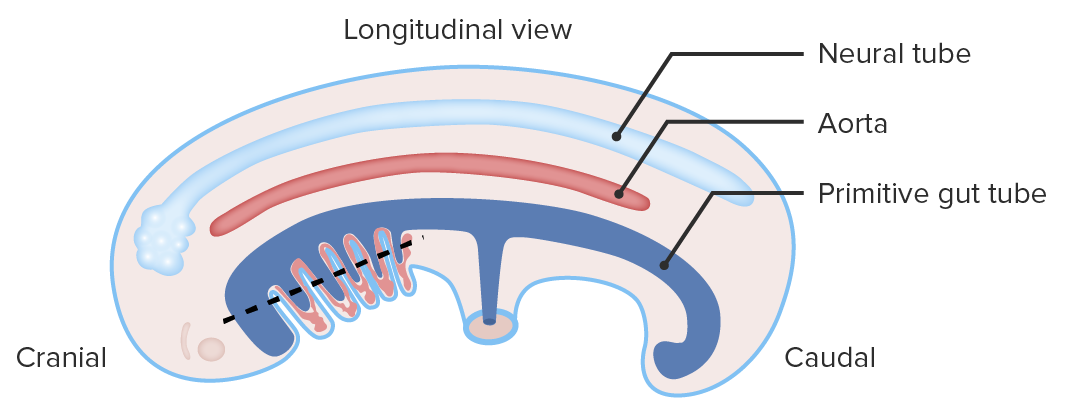
Diagram depicting the pharyngeal aortic arches in the developing embryo
Image by Lecturio.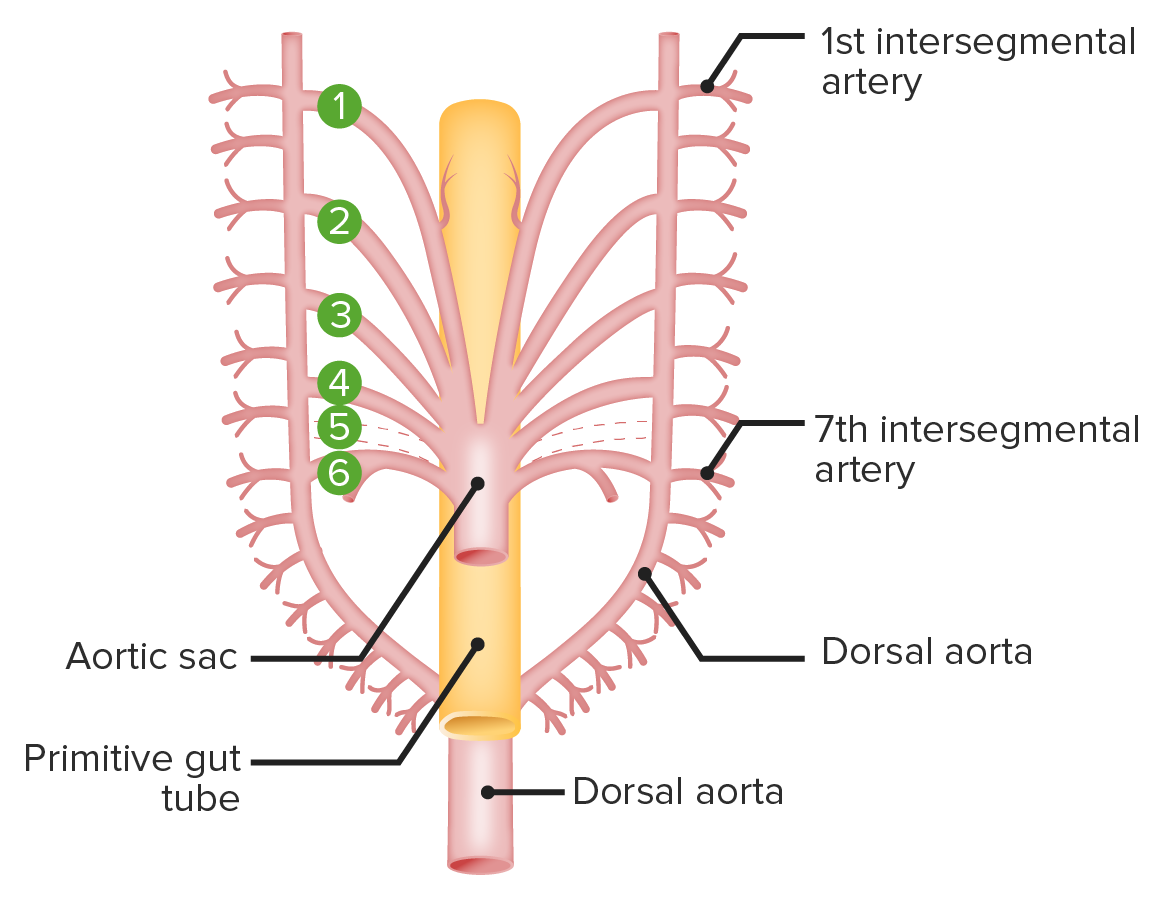
Diagram displays the structure and location of the aortic arches in the earliest stages of their development (numbered 1‒6):
Note that the 5th aortic arch does not develop in humans. The gut tube is located posterior to the arches and developing heart but anterior to the fused dorsal aorta. There are 2 dorsal aortas in the cranial portion of the embryo, 1 on the right and another on the left, which receive blood from the aortic arches.
Image by Lecturio.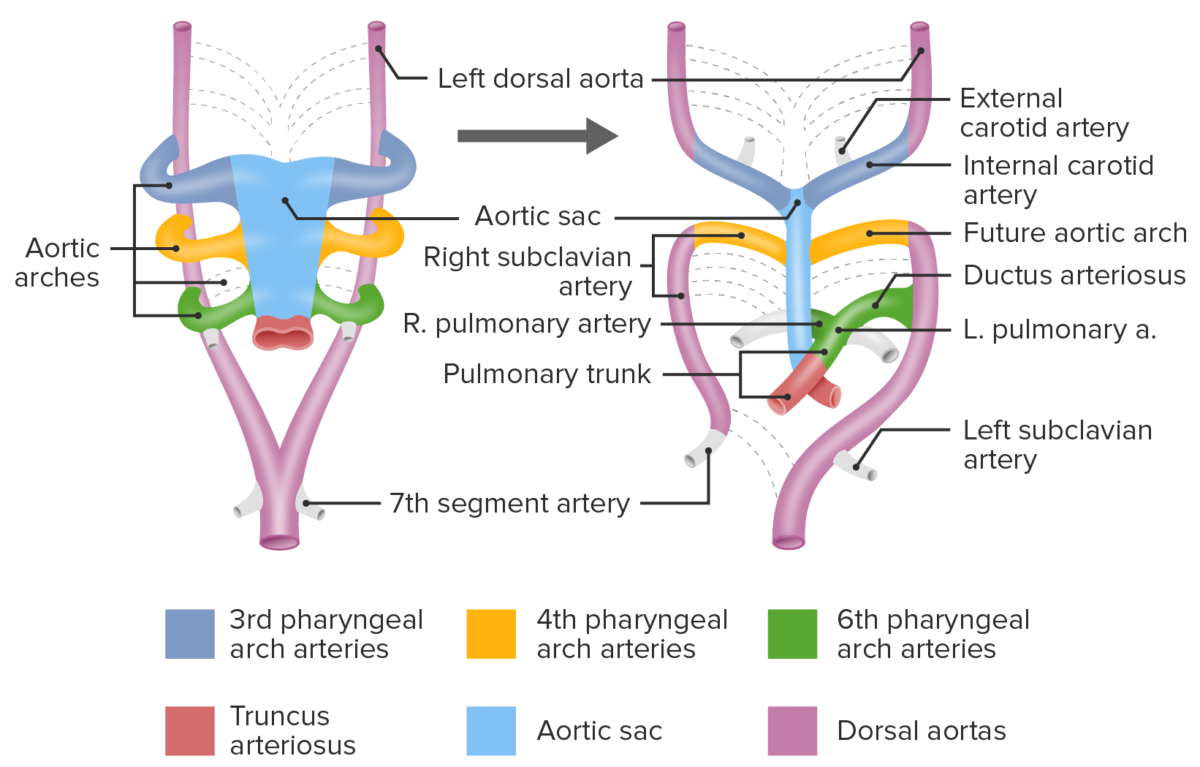
Diagram depicting formation, regression, and differentiation of the pharyngeal aortic arches
Image by Lecturio.The pharyngeal clefts are created by the invaginations of ectoderm Ectoderm The outer of the three germ layers of an embryo. Gastrulation and Neurulation on the external between the pharyngeal arches.
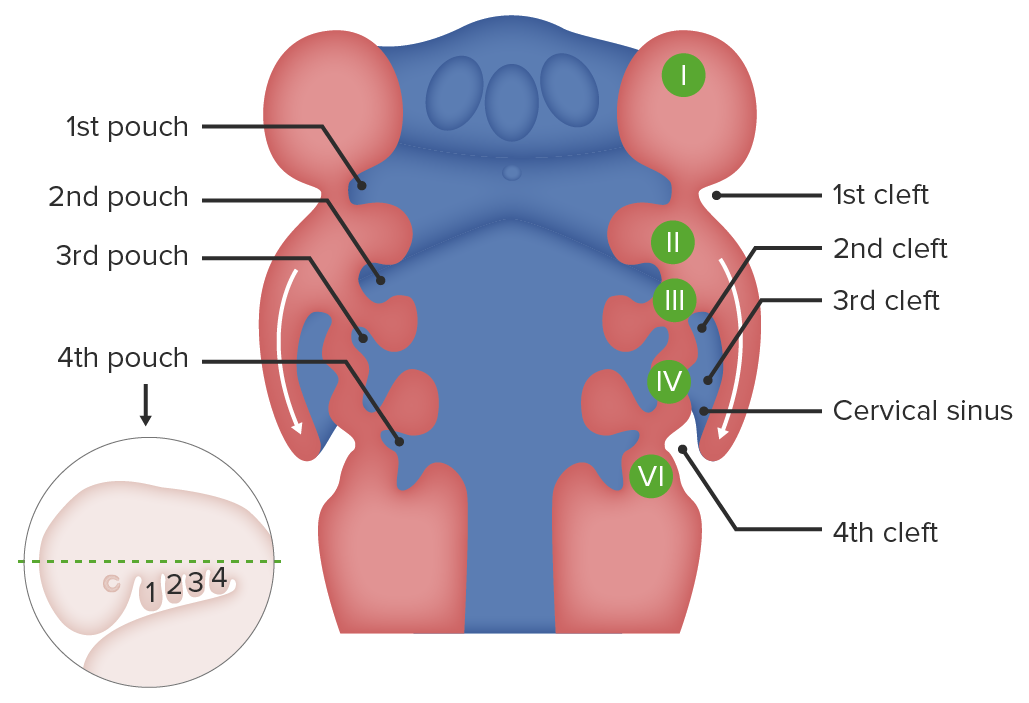
Development of the pharyngeal clefts
Image by Lecturio.The pharyngeal pouches are created by the outward folding of endoderm Endoderm The inner of the three germ layers of an embryo. Gastrulation and Neurulation between the pharyngeal arches.
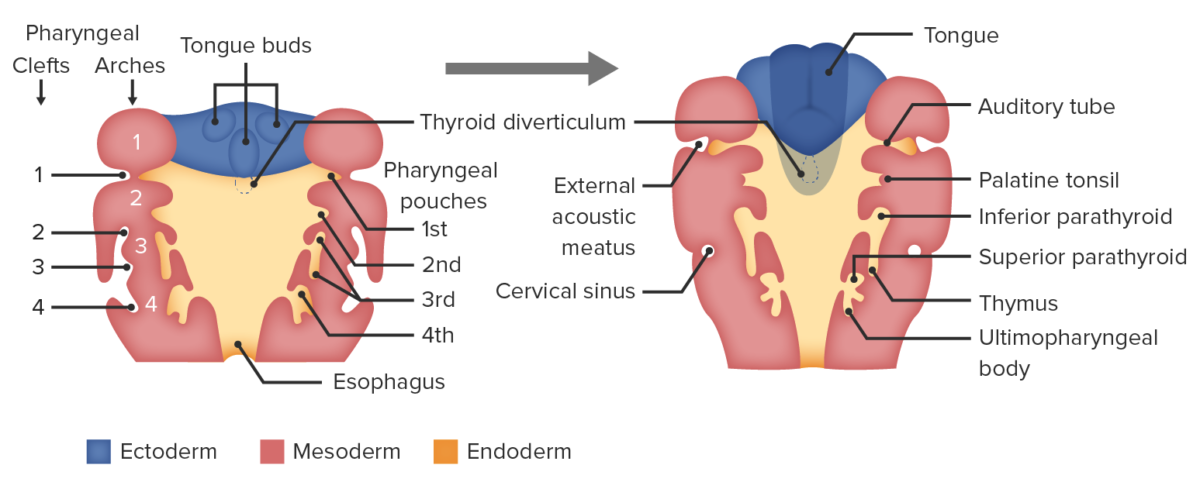
Development of the pharyngeal pouches
Image by Lecturio.