A Meckel’s diverticulum Diverticulum A pouch or sac opening from the colon. Diverticular Disease is a persistent remnant of the omphalomesenteric (vitelline) duct. A Meckel’s diverticulum Diverticulum A pouch or sac opening from the colon. Diverticular Disease is usually located in the antimesenteric border of the ileum Ileum The distal and narrowest portion of the small intestine, between the jejunum and the ileocecal valve of the large intestine. Small Intestine: Anatomy. The mucosal lining of the diverticulum Diverticulum A pouch or sac opening from the colon. Diverticular Disease may contain heterotopic Heterotopic Transplantation of tissue typical of one area to a different recipient site. The tissue may be autologous, heterologous, or homologous. Organ Transplantation mucosa (most commonly gastric). Though frequently asymptomatic, a Meckel’s diverticulum Diverticulum A pouch or sac opening from the colon. Diverticular Disease can cause ulceration Ulceration Corneal Abrasions, Erosion, and Ulcers and present with lower gastrointestinal (GI) bleeding. Other complications include diverticulitis Diverticulitis Inflammation of a diverticulum or diverticula. Diverticular Disease or small bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis ( SBO SBO Small bowel obstruction (SBO) is an interruption of the flow of the intraluminal contents through the small intestine, and is classified as mechanical (due to physical blockage) or functional (due to disruption of normal motility). The most common cause of SBO in the Western countries is post-surgical adhesions. Small bowel obstruction typically presents with nausea, vomiting, abdominal pain, distention, constipation, and/or obstipation. Small Bowel Obstruction). A Meckel’s scan can detect the diverticulum Diverticulum A pouch or sac opening from the colon. Diverticular Disease in hemodynamically stable patients Hemodynamically Stable Patients Blunt Chest Trauma. For those with active bleeding, arteriography is the diagnostic option. The treatment for a symptomatic Meckel’s diverticulum Diverticulum A pouch or sac opening from the colon. Diverticular Disease is surgery.
Last updated: Jan 18, 2024
A Meckel’s diverticulum Diverticulum A pouch or sac opening from the colon. Diverticular Disease is a persistent remnant of the omphalomesenteric duct. A Meckel’s diverticulum Diverticulum A pouch or sac opening from the colon. Diverticular Disease is a true diverticulum Diverticulum A pouch or sac opening from the colon. Diverticular Disease (contains all layers of the bowel wall), arising from the antimesenteric surface of the middle-to-distal ileum Ileum The distal and narrowest portion of the small intestine, between the jejunum and the ileocecal valve of the large intestine. Small Intestine: Anatomy.
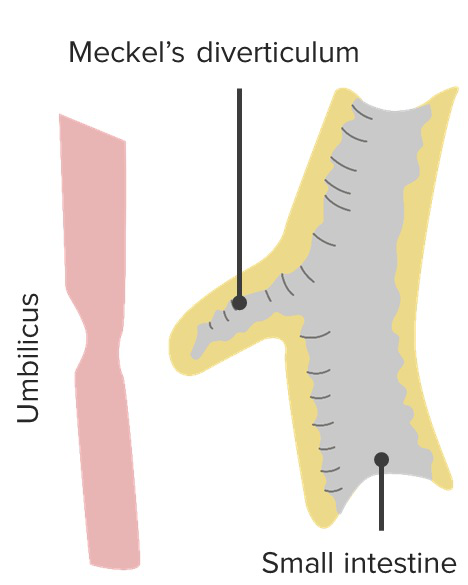
A Meckel’s diverticulum
Image by Lecturio.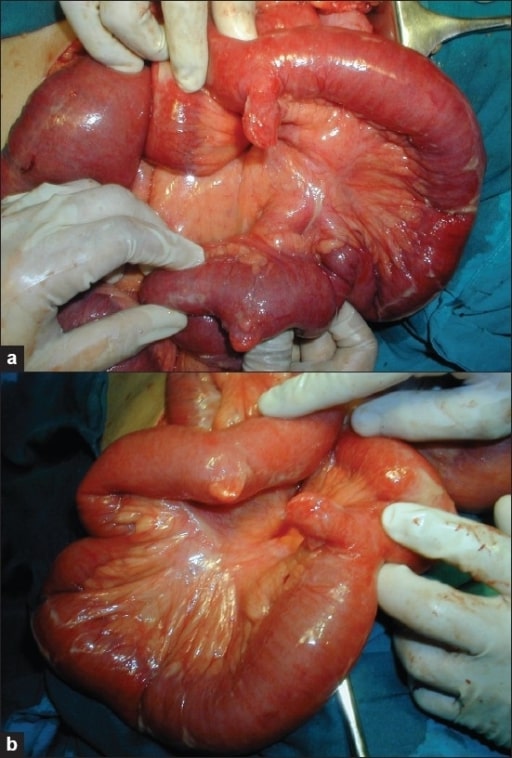
Images (a) and (b) showing a double Meckel’s diverticulum
Image: “Photograph showing double Meckel’s diverticulum” by the Department of General Surgery, Fr. Muller Medical College Hospital, Kankanady, Mangalore (D.K.), Karnataka, India. License: CC BY 2.0.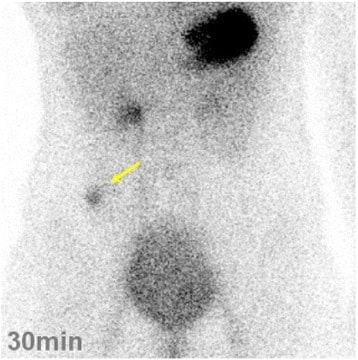
Technetium-99m pertechnetate scintigraphy image showing a hot spot (yellow arrow) on the right lower abdomen: This 14-year-old patient presented with tarry stools and was diagnosed with a Meckel’s diverticulum.
Image: “Intestinal hemorrhage” by the Department of Gastrointestinal and Hepato-Biliary-Pancreatic Surgery, Nippon Medical School, 1-1-5, Sendagi, Bunkyo-ku, Tokyo, 113-8603 Japan: Seiichi Shinji. License: CC BY 4.0.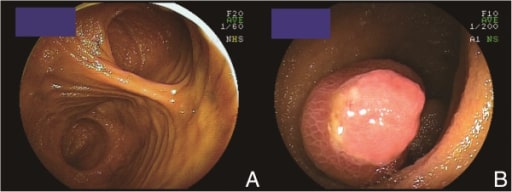
A Meckel’s diverticulum observed by double-balloon enteroscopy:
A: 1 lumen, located at the bottom of the screen, became a blind end.
B: an inverted Meckel’s diverticulum with ulceration
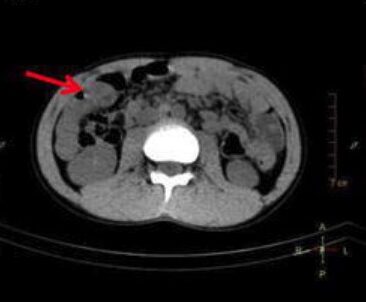
Computed tomography (CT) scan demonstrating a Meckel’s diverticulum: a blind-ending tubular structure in the right abdomen (arrow)
Image: “Axial SPECT/CT” by the Department of Nuclear Medicine, China-Japan Union Hospital, Jilin University, 126 Xiantai Avenue, Changchun, 130033 China: Qian Xie. License: CC BY 4.0, edited by Lecturio.
A Meckel’s diverticulum (perforated by a fish bone) as viewed during surgery
Image: “Meckel’s diverticulum” by the Department of General Surgery, General Hospital of Thessaloniki, O Agios Dimitrios Kanari 7 Stavroupoli, Thessaloniki PC56430, Greece. License: CC BY 2.0.