Chiari malformations (CMs) are a group of central nervous system Central nervous system The main information-processing organs of the nervous system, consisting of the brain, spinal cord, and meninges. Nervous System: Anatomy, Structure, and Classification (CNS) conditions characterized by the underdevelopment of the posterior cranial fossa Posterior cranial fossa The infratentorial compartment that contains the cerebellum and brain stem. It is formed by the posterior third of the superior surface of the body of the sphenoid (sphenoid bone), by the occipital, the petrous, and mastoid portions of the temporal bone, and the posterior inferior angle of the parietal bone. Skull: Anatomy with subsequent protrusion of neural structures through the foramen magnum. There are 4 types of CM, with type I being the most common. Headaches are the most common symptom. Diagnosis is made by clinical findings and confirmed by magnetic resonance imaging (MRI). Treatment is surgical, based on decompression of the posterior fossa and restoration of CNS flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure. Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas depends on the type of malformation.
Last updated: Jan 7, 2025
Chiari malformations (CMs) are a group of disorders defined by structural deficits in the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy leading to limited space in the posterior fossa, which forces cerebellar structures to protrude through the foramen magnum.
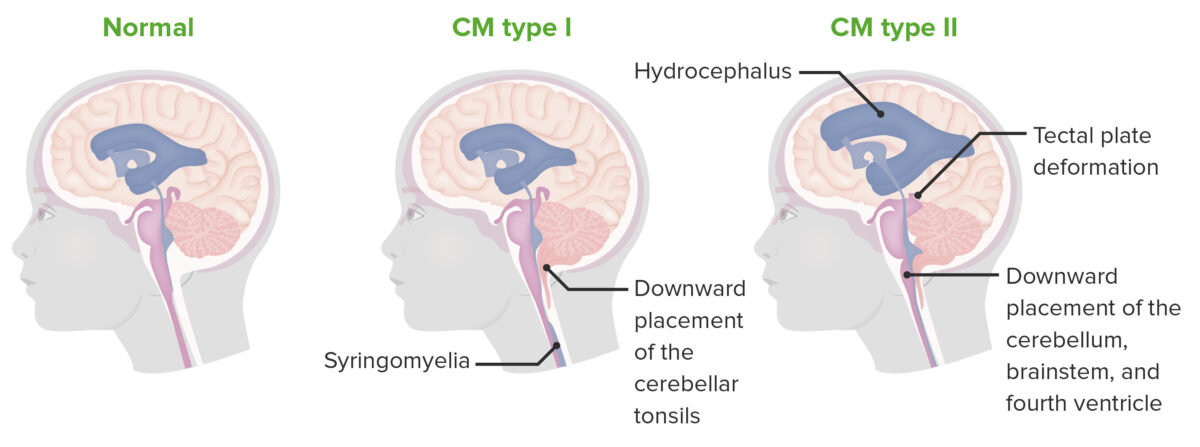
Chiari type I and II
Chiari malformations are characterized by an underdeveloped posterior cranial fossa, with subsequent protrusion of neural structures through the foramen magnum. Type 1 is characterized by herniation of the cerebellar tonsils only, while type 2 involves more structures.
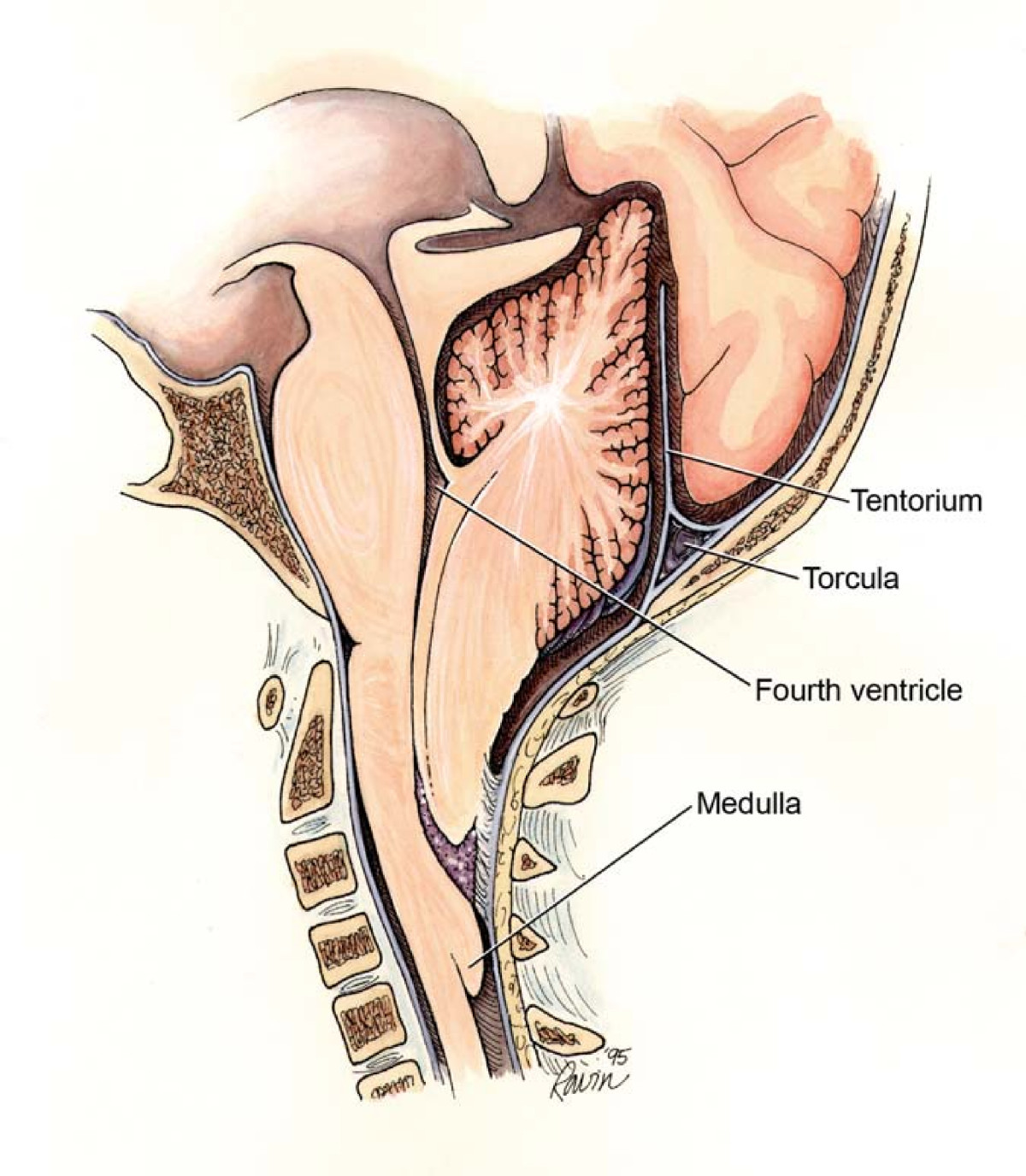
Chiari II malformation showing the points of potential obstruction that yield different subtypes of hydrocephalus
Image: “Chiari2” by Rekate HL. License: CC BY 2.0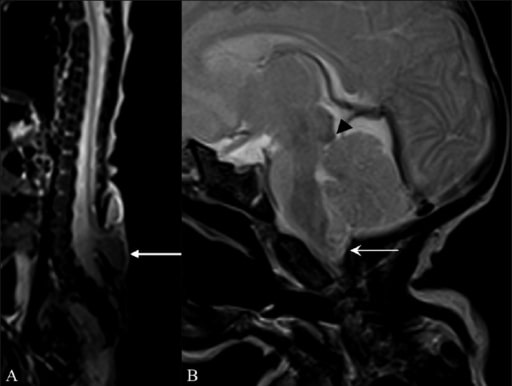
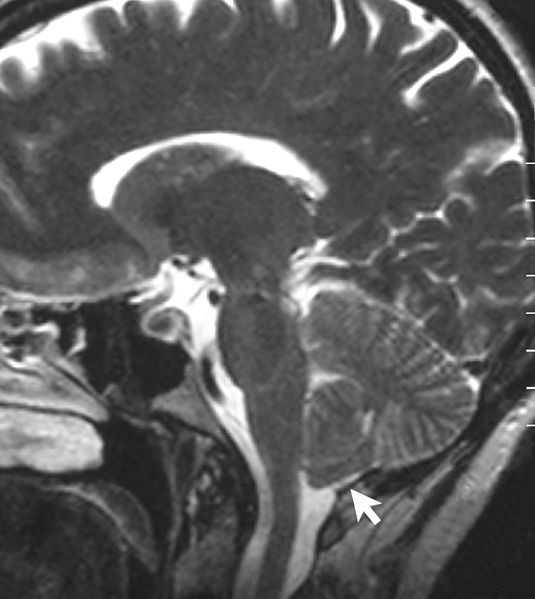
Magnetic resonance imaging (MRI) findings suggestive of Arnold–Chiari II malformation
Sagittal T2W whole-spine MRI (A) shows a meningomyelocele (arrow) opposite the L5 and S1 vertebrae. Sagittal T2W MRI of the brain (B) shows a small posterior cranial fossa, with herniation of the cerebellar vermis and tonsils (arrow) through the foramen magnum with tectal beaking (arrowhead).
Incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency:
Associated conditions:
Neurologic symptoms are caused by:
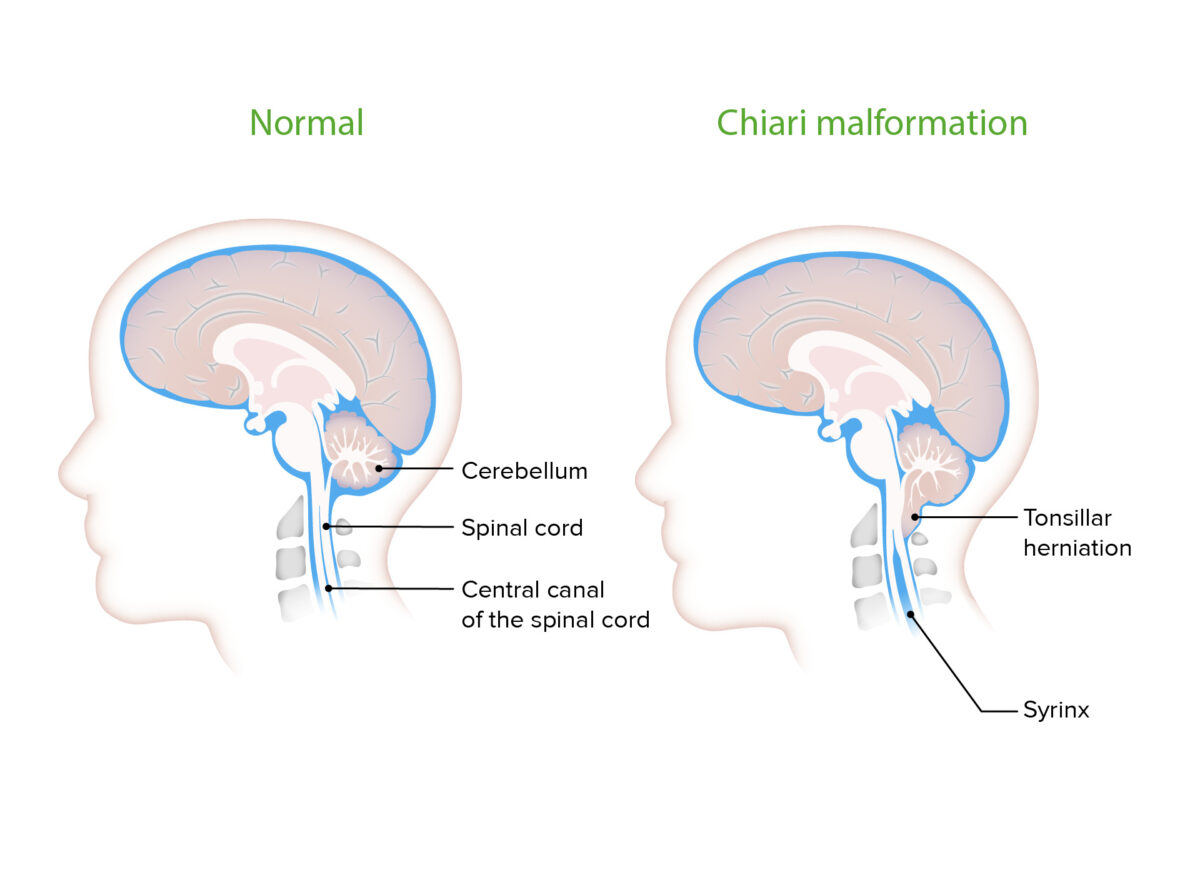
Syrinx seen with Chiari malformation
Cavities filled with cerebrospinal fluid (CSF) are commonly seen with CMs. They cause symptomatology commonly associated with the malformation by putting pressure on the surrounding neural tissue.
Symptoms:
Physical signs:
Symptoms:
Physical signs:
There is high infant mortality Mortality All deaths reported in a given population. Measures of Health Status with this type.
Symptoms:
Physical signs:
Magnetic resonace imaging scan showing a type I CM. Notice the tonsillar herniation.
Image: “Sagittal MRI scan of brain of patient with Chiari malformation” by Raymond F Sekula Jr et al. License: CC BY 2.0